Journal of
eISSN: 2373-6410


Case Report Volume 14 Issue 1
1Department of Internal Medicine, Serviço de Saúde da Região Autónoma da Madeira, Portugal
2Department of Intensive Medicine, Serviço de Saúde da Região Autónoma da Madeira, Portugal
3Department of Radiology, Madeira Medical Center, Portugal
Correspondence: Rafael Nascimento, Department of Internal Medicine, Serviço de Saúde da Região Autónoma da Madeira, Portugal
Received: December 19, 2023 | Published: January 9, 2024
Citation: Gouveia F, Ferreira SD, Lemos C, et al. Takayasu arteritis - a case report of neurological clinical manifestation in an elderly patient. J Neurol Stroke. 2024;14(1):1-3. DOI: 10.15406/jnsk.2024.14.00570
Takayasu Arteritis is a chronic granulomatous inflammatory arteriopathy that affects the aorta and its main branches, leading to arterial stenosis and sometimes thrombosis, with the left subclavian artery being the most frequently involved. Clinical manifestations are insidious, nonspecific, and variable, depending on the arterial territory affected, without any pathognomonic finding. It is a rare disease, with an annual incidence of 2.6 cases per million people, being more common in Southeast Asia and affecting predominantly women, especially at reproductive age. However, it is believed that this disease is underdiagnosed, especially in the most advanced age groups.
Keywords: takayasu arteritis, autoimmune diseases, neurological manifestation, vasculitis, inflammatory arteriopathy, elderly patient
Takayasu arteritis (TA) is a chronic inflammatory arteriopathy affecting the aorta and its major branches, leading to arterial stenosis and thrombosis. The disease's origin is complex, and influenced by genetic and environmental factors. Inflammation initiates in the adventitial layer through an autoimmune mechanism, resulting in the thickening of the vessel wall and contributing to vascular destruction and aneurysm formation. TA can manifest as localized or involve the entire vessel, with initial lesions often observed in the left subclavian artery, progressing to other major arteries. TA is a rare disease (annual incidence of 2.6 cases per million), with a higher prevalence in Southeast Asia, predominantly affecting women of reproductive age. Symptoms have a subacute onset and lack specific features, causing potential delays in diagnosis.
Clinical manifestations include various vascular symptoms and neurological involvement in about 20% of cases. Diagnosing TA poses challenges due to the difficulty of obtaining large artery biopsies. Imaging studies such as Angio-Tomography (Angio-CT) and Magnetic Resonance Imaging (MRI) play a crucial role in diagnosis, helping determine disease extent and differentiate from other vasculitis. The 1995 diagnostic criteria proposed by Sharma et al focus on major and minor criteria. Primary treatment involves high-dose corticosteroid therapy, with progressive weaning recommended. Additional immunosuppressants may be considered based on case reports. Surgical intervention is reserved for inactive diseases with severe ischemic complications, utilizing either endovascular or surgical approaches based on the extent of injuries.
TA is underdiagnosed, especially in the most advanced age groups. The clinical manifestations are insidious and non-specific, especially neurological manifestations, which makes diagnosis a challenge in the case report.
An 87-year-old female Caucasian patient was referred by her primary care doctor to the Internal Medicine consultation for repeated syncope associated with unilateral transient amaurosis. She had a history of peripheral venous disease and depression and was currently taking Pentoxifylline 400mg id, Donepezil 50mg id, and
Sertraline 50mg id. The main physical examination remarks were immeasurable blood pressure in both upper limbs as well as the absence of bilateral radial, brachial, and axillary pulses, with maintained femoral pulses. No changes on cardiac auscultation, carotid murmurs and no other relevant changes.
Blood tests revealed no changes, except an Erythrocyte sedimentation rate (ESR) of 56m, and C-reactive protein (CRP) of 44 mg/L. Plasma and urinary catecholamine levels were within the reference values. The autoimmunity study was negative. The electrocardiogram showed sinus rhythm, with a heart rate of 73 beats per minute, with no changes in rhythm, conduction, or ventricular repolarization. The 24-hour Holter confirmed the baseline sinus rhythm and some periods of 2nd-degree atrioventricular block Mobitz I during sleep. To complete de cardiac study, an echocardiogram was performed, which revealed mild mitral-aortic degenerative changes, aortic valve fibrosis, mitral ring calcification, mild regurgitation, and an enlarged left atrium. For the absence of palpable pulses, an Arterial Eco-Doppler of the Upper Limbs was performed, revealing a significant stenosis of the axillary arteries bilaterally, more severe on the right and with distal hemodynamic compromise. To exclude a Giant Cell Arteritis a Cerebral Vessel Wall MRI was performed and excluded changes in the temporal artery. Lastly, the Thoracic and Abdominal Angio-CT showed a diffuse thickening of the aorta wall, (Figure 1), stenosis of the left subclavian artery (Figure 2 & 3) with an inflammatory component, reduction in the caliber of the right subclavian artery and severe stenosis of the renal artery (Figure 4), thus suggesting a Takayasu Disease.
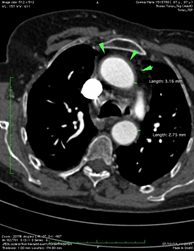
Figure 1 On axial Angio-CT slice, Diffuse thickening of the ascendent and descending aorta are indicated by green arrowheads and green line.
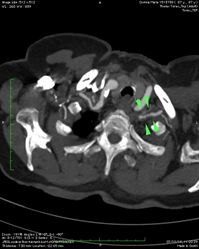
Figure 2 On axial Angio-CT slice, stenosis of the left subclavian artery with an inflammatory component is indicated by green arrows.
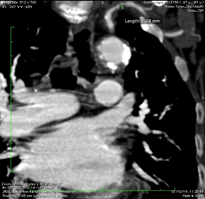
Figure 3 On coronal Angio-CT slice, stenosis of the left subclavian artery with an inflammatory component is indicated by a green arrow.

Figure 4 On coronal Angio-CT slice, severe stenosis of the right renal artery is indicated by a green arrow.
Consequently, the patient has corticosteroid therapy with prednisolone at a dose of 1mg/kg/day. At a 6-month follow-up, the patient reported zero syncope episodes, upper arm pulses were palpable and blood tests showed a reduction in both rate ESR and CRP.
TA is a chronic granulomatous inflammatory arteriopathy that affects the aorta and its main branches, leading to arterial stenosis and sometimes thrombosis.1 Its pathophysiology is unclear and appears to be influenced by genetic and environmental factors.1 The wall of the great arteries consists of three main layers: the adventitia, middle, and internal, which are irrigated by the vasa vasorum found in the adventitia layer.1
Vascular inflammation due to lymphocyte reaction begins in the adventitial layer by an unknown process.1 These lymphocytes subsequently migrate to the middle layer, triggering a TH1and TH17 response, culminating in the differentiation of fibroblasts into myoblasts, which migrate back to the adventitia layer, thickening the vessel wall, and, through the action of proteolytic enzymes, cause vascular destruction and aneurysm formation.1,2 The inflammation may be localized or can involve the entire vessel.1-2 Despite the great variability of this disease, the initial lesions most often occur in the proximal or medial portion of the left subclavian artery, progressing to the carotid, vertebral, and aorta arteries.1–5
The annual incidence of TA is about 2.6 cases per million people, is more common in Southeast Asia, and affects predominantly women, especially at reproductive age. However, it is believed that this disease is underdiagnosed, especially in the most advanced age groups.2 The onset of symptoms in TA tends to be subacute, with no pathognomonic features, which may delay the diagnosis from months to years.1–5 They are the result of the progression of narrowing, occlusion, or dilatation of the arteries.2,3 As examples we have absent or weak peripheral pulses, limb claudication, arterial bruit, discrepant blood pressure between arms, hypertension, angina, dyspnea, abdominal pain, skin lesions, lightheadedness, vertigo, syncope, and strokes.3,4 Approximately 20% of patients with diagnostic data present neurological symptoms, which may be the presenting symptoms of the disease.6 In the case of our patient, repeated syncope associated with amaurosis was the reason for referral for study. Constitutional symptoms, such as weight loss, low-grade fever, and fatigue are frequent, particularly in the disease's early stages.3,4
Since a biopsy of large arteries is not easy to obtain, imaging studies are essential for the diagnosis of TA, allowing the extent of the disease to be determined and the differential diagnosis to be made with other diseases, particularly other vasculitis.7 Radiologic changes can be investigated by Angio-CT, which allows assessment of the arterial wall to be assessed and inflammatory activity may be detected with contrast uptake. Angio-MRI also assesses the lumen and the vascular wall, and inflammatory activity can be detected by gadolinium uptake. Angiography is indicated for preoperative evaluation in surgical treatment,2,3 however, angiography for diagnosis is currently no longer recommended.8 Histological evaluation is not routinely performed in patients with AT, as this is only possible if surgery is necessary or during an autopsy.9
The most recent diagnostic criteria for TA, proposed by Sharma et al in 1995, defines a high probability of disease when 2 major criteria, 1 major and 2 minor criteria, or 4 minor criteria are met (Table 1).4 The most commonly used initial treatment is high-dose corticosteroid therapy (1mg/kg of prednisolone or equivalent), which is associated with a very favorable response, acting on the previously described TH17 pathway.5 Although dose reduction may be associated with relapses, progressive weaning is suggested.5 Other immunosuppressants can be used, particularly Tocilizumab, according to experience based on case reports. Surgical treatment is indicated for inactive disease for severe ischemic complications, with the endovascular approach indicated for areas of localized stenosis and the surgical approach for large injuries.5 Overall, the evidence suggests a poorer prognosis in patients with significant vascular complications, a progressive disease course, and advanced age.9
|
Three major criteria |
|
|
Left mid-subclavian artery lesion |
The most severe stenosis or occlusion present in the mid portion from the point 1cm proximal to the vertebral artery orifice up to that 3 cm distal to the orifice determined by angiography. |
|
Right mid-subclavian artery lesion |
The most severe stenosis or occlusion present in the mid portion from the right vertebral artery orifice to the point 3 cm distal to orifice determined by angiography. |
|
Characteristic signs and symptoms of at least one-month duration |
These include limb claudication, pulselessness or pulse differences in limbs, an unobtainable or significant blood pressure difference (> 10 mmHg systolic blood presence difference in limb), fever, neck pain, transient amaurosis, blurred vision, syncope, dyspnea or palpitations. |
|
Ten minor criteria |
|
|
High ESR |
Unexplained persistent high ESR > 20 mm/h (Westergren) at diagnosis or presence of the evidence in the patient's history. |
|
Carotid artery tenderness |
Unilateral or bilateral tenderness of common arteries on palpation. Neck muscle tenderness is unacceptable. |
|
Hypertension |
Persistent blood pressure> 140/90 mmHg brachial or > 160/90 mmHg popliteal. |
|
Aortic regurgitation or Annuloaortic ectasia |
By auscultation or Doppler echocardiology or angiography; By angiography or two-dimensional echocardiography. |
|
Pulmonary artery lesion |
Lobar or segmental arterial occlusion or equivalent determined by angiography or perfusion scintigraphy, or presence of stenosis, aneurysm, luminal irregularity, or any combination in the pulmonary trunk or unilateral or bilateral pulmonary arteries determined by angiography. |
|
Left-mid common carotid lesion |
Presence of the most severe stenosis or occlusion in the mid portion of 5 cm in length from the point 2 cm distal to its orifice determined by angiography. |
|
Distal brachiocephalic trunk lesion |
The presence of the most severe stenosis or occlusion in the distal third determined by angiography. |
|
Descending thoracic aorta lesion |
Narrowing, dilation or aneurysm, luminal irregularity, or any combination determined by angiography: tortuosity alone is unacceptable. |
|
Abdominal aorta lesion |
Narrowing, dilation or aneurysm, luminal irregularity or aneurysm combination. |
|
Coronary artery lesion |
Documented on angiography below the age of 30 years in the absence of risk factors like hyperlipidemia or diabetes mellitus. |
Table 1 Modified diagnostic criteria for Takayasu Arteritis
None.
The authors declare that there are no conflicts of interest.

©2024 Gouveia, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.