Journal of
eISSN: 2373-6410


Case Report Volume 14 Issue 1
1Abdou Moumouni University of Niamey, Department of Neurosurgery, National Hospital of Niamey (Niger)
2Research Department of Sub-Saharan Africa Futures Neurosurgeons Association (SAFNA), Cotonou, Benin Republic
Correspondence: DOSSOU Mèhomè Wilfried , Abdou Moumouni University of Niamey, Department of Neurosurgery, National Hospital of Niamey (Niger)
Received: January 05, 2024 | Published: January 18, 2024
Citation: Assoumane II, Dossou MW, Agada KN, et al. Spontaneous acute subdural hematoma: a case report and literature review. J Neurol Stroke. 2024;14(1):5-7. DOI: 10.15406/jnsk.2024.14.00571
Background: Subdural hematoma is very often associated with head trauma. There are few documented cases of spontaneous acute subdural hematoma without a history of
Case presentation: A 50-year-old man was admitted for a mild-intensity headache in helmet-like, which occurred in the night without any cause waking him up from his sleeping. He denied any drug taken, mainly anticoagulant, non-steroidal anti-inflammatory drugs. The neurological exam was absolutely normal. The head CT Scan performed showed a thick left fronto-temporal spontaneous acute subdural hematoma The blood investigations were normal. Brain angio-CT didn’t show any The patient benefited fromconservative treatment under observation and experienced a progressive regression of the headache throughout the hospitalization stay. He was discharged an eleventh day later.
Conclusion: Spontaneous acute subdural hematoma is a rare entity. It requires painstaking clinical, biological, and imaging and a strict follow-up for its
Keywords: spontaneous, acute, subdural hematoma, Niamey
Subdural hematoma is very often associated with head traumatism.1,2 Spontaneousacute subdural hematoma without a history of traumatism is very rare. There are few documented cases of spontaneous acute subdural hematoma without a history of traumatism.3 Revelation clinical signs are often headaches, the investigations tools are CT scan and MRI and also angiography. Hear authors report a rare case of spontaneous acute subdural hematoma on a youngman manage at Niamey National Hospital in Niger.
A 50-year-old man with a past history of high blood pressure and diabetes diagnosed about 06 years ago was admitted for sustained headache. So the patient was complaining of a helmet-like headache, with a mild intensity, that occurred in the nighttime without any cause waking him up from his sleeping. The patient came to the hospital about 15 hours from the onset. There were other accompanying signs such as vomiting, seizure, and agitation. The patient denied any head trauma recently or priorly. He also denied any drug taken, mainly an anticoagulant, a non-steroidal anti-inflammatory. On physical examination, the patient was alert (Glasgow Coma Scale =15), breathing normally without any assistance (Pulsed oxygen saturation (SaO₂)= 98%; Respiratory rate= 18cycles per minute) but had a non-stable hemodynamic condition (Blood pressure=155/95mmHg); the pulse was 87 cardiac cycles.The neurological exam was absolutely normal (equal and reactive pupils; any neurological deficit).
The head CT Scan performed showed a thick left parieto-temporal hyperdensity witha slight midline shift making think of spontaneous acute subdural hematoma (SASH) (Figure 1). The blood investigations (Prothrombin time and Activated partial thromboplastin time; Complete Blood Count; Ionogram; Blood sugar) were normal. Brain angio-CT didn’t show any abnormality (Figure 2). The diagnosis of spontaneous acute subdural hematoma has been retained despite the unavailability of angiography in our context. The patient benefited from conservative treatment under observation (analgesic (combined stage 1 and 2), saline-based fluid intake, osmotherapy for 48 hours, and anti-hypertensive on cardiological advice). The head CT Scan performed 02 days later was unchanged outside a slight remission of meningeal hemorrhage (Figure 3).
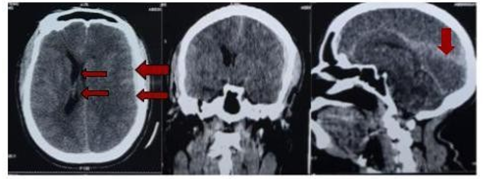
Figure 1 Non injected CT showing left fronto-temporal subdural hematoma with midline deviation and subarachnoid hemorrhage.
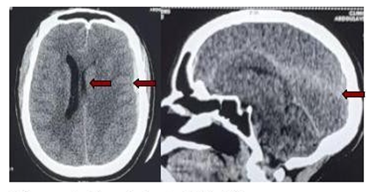
Figure 3 Non injected CT 48h post admission inspection showing persistence left fronto-temporal subdural hematoma with midline deviation and subarachnoid hemorrhage in remission.
The patient experienced a progressive regression of headache throughout the hospitalization stay. He was discharged an eleventh day later. The follow-up at 1 and 3 months show a patient with no complaints and a normal neurological examination.
Epidemiology - Pathophysiology
Acute subdural hematoma very often occurs in a head trauma context and the bleeding is due to a rupture of a vein or artery crossing the subdural space. Spontaneous acutesubdural hematoma (SASH) is a distinct clinical entity with any apparent cause.4 This patient's case meets the definition of SASH, as there is no reported notion of trauma.
Currently, around 200 cases of SASH have been reported in the literature and accountfor 0.7 to 6.7% of all acute subdural hematomas. Young male predominance has beenreported with an age over 40 years.4 Previous reports show a predominance of adolescent males.3 Risk factors for spontaneous acute subdural hematomas include vascular malformations, neoplasia, dural metastases, hypervitaminosis, hematological diseases (coagulopathy), spontaneous intracerebral hypotension, alcoholism, cocaine use, arterial hypertension, bleeding from cerebral artery aneurysms or cortical arteries.3 Among all these, the arterial origin is the most found (60%).4 Around 40% of patients with spontaneous acute subdural hematoma have hypertension and associated alcohol abuse. Arteriosclerosis in hypertensive patients may predispose to rupture of vessels close to the dura. Mortality rates for SASH vary according to etiology, with an average of 37%. The mortality rate varies from 50 to 90%.4 None of the etiologies listed above were reported in this patient.
For most authors, the factor favoring pericerebral subdural bleeding is primary or acquired hypotension (cerebrospinal fluid (CSF) diversion, lumbar puncture, dehydration). The consequence is traction on the cortico-dural veins, leading to a rupture, particularly at thelevel of their attachment to the dura mater (Figure 3).5–8 Spontaneous arterial hemorrhage may be due to the rupture of an arterial branch at the right angle of a cortical artery, which isa potential point of weakness, vulnerable to rupture in the event of increased pressure in the vascular lumen, or the rupture of a cortical artery at the level of adhesion with the dura mater.9 In this patient with no obvious risk factor or notion of trauma, dehydration seems to be themost plausible suggestion, especially the local climatic condition where the temperature can reach or even exceeds 40°C during the dry season.
Hypovolemia of the CSF results in the descent of the encephalon, leading to traction on the meninges and vessels of the skull, which is the cause of the pain and is increased by standing. The existence of constitutive anomalies in the dura mater, making it fragile, increases the risk of dural lesions. Another hypothesis is a mismatch between CSF productionand resorption, leading to hypovolaemia, which is the cause of meningeal damage.10 The two complications to be feared are cerebral venous thrombosis and subdural hematoma. Froma physical point of view, the formation of subdural collections or hematomas is considered to compensate for the loss of intracranial pressure. Consequently, these collections or hematomas are rarely responsible for intracranial hypertension.11,12 There were no obvious signs of intracranial hypertension in this patient.
Clinical appearance
The clinical features of this condition were first described in 1971 by Talalla and McKissock4 Subsequently, Tokoro et al. changed the name to acute subdural hematoma of arterial origin, with the following criteria:4
The clinical picture of spontaneous acute subdural hematoma develops progressively over several hours to days. Usually, consciousness is impaired, sometimes to the point of coma. Headache, vomiting, neurological deficits such as hemiparesis, papilledema, or signsof cerebral involvement may also be present. (4) This patient presented with an isolated headache.
Imaging aspect
The current literature, consisting mainly of surgical case reports, does not offer a consensus etiological diagnostic approach. No diagnostic algorithm for etiological research has been evaluated and validated in this situation, so clinical and paraclinical investigations may vary from one center to another. The examinations most frequently proposed are CT scan, MRI, angiography (to investigate a vascular anomaly), and conventional hemostasis work-up in search of coagulopathy.2 The angio- CT performed on this patient showed no detectable vascular anomaly or hypertensive angiopathy. The blood investigations were normal as well.
Therapeutic aspects
Spontaneous acute subdural hematoma correlates with good outcomes whendiagnosed and treated early in the clinical course.3 Poor prognostic factors, according to Missori et al. are: delayed access to surgery, low Glasgow score, and midline deviation
>13 mm on CT-scan. Early surgery is the most important factor in survival.4
Surgical management of these patients does not appear to be the rule. For some authors, evacuation of subdural hematomas as part of a CSF hypotension syndrome aggravates the latter.12 The patient, in this case, reported benefiting from symptomatic medical treatment. There was no indication of surgical evacuation of the hematoma.
Spontaneous subdural hematoma is a rare entity. It is often associated with vascular malformations, hematological disease, spontaneous intracerebral hypotension, or arterial hypertension. It requires a vascular work-up and an urgent neurosurgical team opinion.
None.
The authors declare no conflicts of interest.

©2024 Assoumane, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.