Journal of
eISSN: 2373-6410


Case Report Volume 6 Issue 6
1Department of Pathology, Necmettin Erbakan University Meram Faculty of Medicine, Turkey
2Department of Neurosurgery, Necmettin Erbakan University Meram Faculty of Medicine, Turkey
Correspondence: Siddika Findik, Assistant Professor, Department of Pathology Necmettin Erbakan University Meram Faculty of Medicine, 428 Akyokus/Meram, Konya, Turkey, Tel +90 332 2236289, Fax +90 332 223 6182
Received: February 21, 2017 | Published: May 26, 2017
Citation: Findik S, Esen HH, Erdi F, Oltulu P (2017) Primary Pilocytic Astrocytoma with Malign Transformation. J Neurol Stroke 6(6): 00222. DOI: 10.15406/jnsk.2017.06.00222
Pilocytic astrocytoma is a slow-growing brain tumor that occurs more often in children with a benign course and long clinical history compared to diffuse astrocytomas. Pilocytic astrocytomas may rarely show malignant transformation and radiotherapy plays a key role in the treatment of malignant transformation. In this study, we present a pilocytic astrocytoma case with no radiotherapy history and showing malignant characteristics histologically on a 3 year old girl.
Keywords: pilocytic astrocytoma, malign transformation, histopathology
According to World Health Organization (WHO), pilocytic astrocytomas (PA) are Grade-I astrocytic tumors. It is the most common brain tumor in children and occurs in the cerebellum localization with a rate of 67%. According to radiological examinations, they are seen as well-circumscribed mass with cystic components.1 The treatment is surgical excision and chemotherapy (CT) and radiotherapy (RT) treatment can be applied in the presence of residual tumor or recurrence.2,3 After total resection, the 10 year and 20 year surveys are 95.8% and 82%, respectively. The survey rates show that pilocytic astrocytoma is a brain tumor with a benign course clinically. However, PAs may show malignant transformation.4˗6 RT plays a key role for malignant changes.6 However, it is suggested that RT is not an effective factor by itself in malignant transformation.3,5 In the present study, we present a PA case showing malignant transformation in a 3-year-old girl caused by 4th ventricle with no previous RT history.
A 3-year-old girl admitted to the Pediatric Clinic of Necmettin Erbakan University Meram Medical Faculty with headaches and vomiting complaints. She was hospitalized for further evaluation and treatment. In the magnetic resonance (MR) imaging, a 5x3.5 cm mass lesion with a heterogeneous character, cystic and solid components extending to foramen magendie on the left was found in the 4thventricle accompanied by obstructive type hydrocephalus symptoms (Figure 1). The tumoral mass was removed by surgery and sent to the Pathology Department with the pre-diagnosis of ependymoma. According to the macroscopic examination, the removed mass was a soft material with off-white color and 6x5x2 cm dimensions and some parts of the tumor were bleeding. The tumoral structure composed of compact and looser areas with ovoid nuclei and hair-like extensions was observed. Eosinophilic granular bodies and rosenthal fibers were present in the tumor. However, significant cellular pleomorphism, cellularity and vascularity increase was observed in some areas in addition to 3 atypical mitosis in 10 high power fields. In addition, there were necrosis areas. In the immunohistochemical studies; tumor cells were GFAP and S-100 positive and EMA, chromogranin and synaptophysin were negative. Ki-67 index was less than 1% in the conventional areas, and 50% in the areas with significant cellularity (Figure 2). The patient was diagnosed with malignant transformation based on these findings. No residual tumor was detected in the post-operative MRI. The case was transferred to pediatric oncology to receive chemotherapy in addition to surgical treatment.

Figure 1 Preoperative magnetic resonance imaging (MRI) scans A-D) Cystic and solid components of tumour extending to foramen magendie on the left was found in the 4th ventricle.
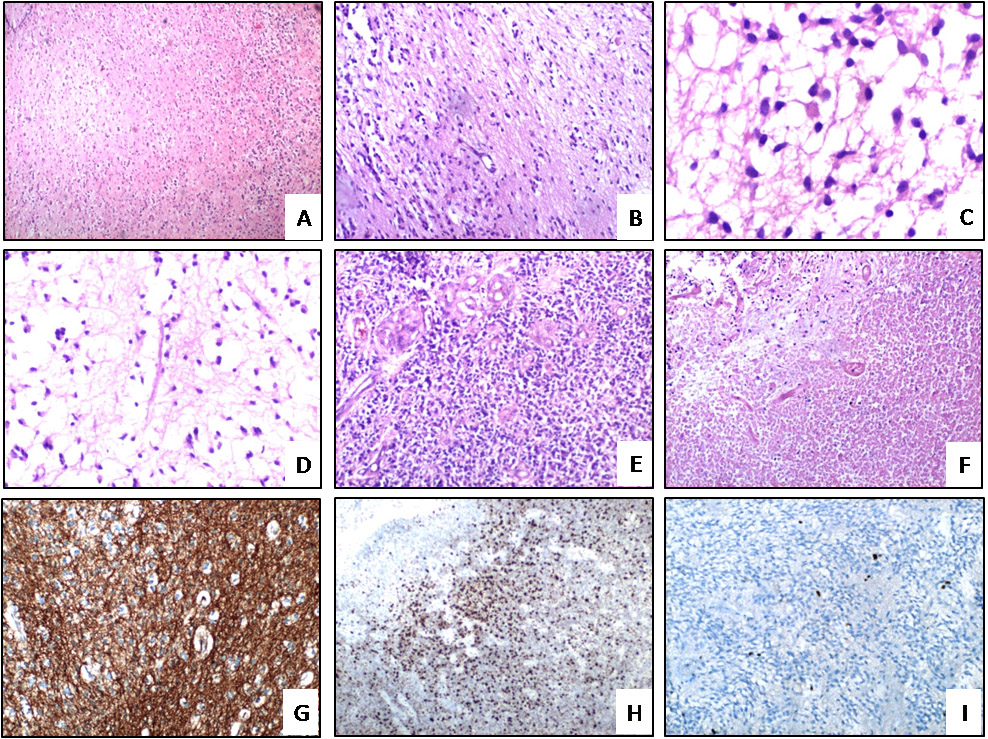
Figure 2 Representative pathological images of the tumoral lesion. A) Tumoral lesion (H&E x40). B) Compact and looser areas in a tumoral lesion (H&E x100). C) Eosinophilic granular bodies (H&E x400). D) Rosenthal fibers (H&E x200). E) Vascular proliferation in a tumoral lesion (H&E x100). F) The necrosis area (H&E 100). G) Positive immunostaining for GFAP (x100). H) In some regions the lesion shows 50% Ki-67 positivity (x40). I) The lesion shows 1% Ki-67 positivity in some areas (x40).
According to WHO, pilocytic astrocytomas are Grade-I astrocytic tumors. They are usually seen in people under 20 years of age. The incidence peaks in the 8-13 age range. These tumors are seen in cerebellum, optic nerve, optic chiasm, hypothalamus, 3rdventricular zone, spinal cord and temporal lobes, respectively.7
Histologically; they are characterized by biphasic tumor pattern developed by compact and loose microcystic areas of pilocytic cells. Hyalinization is seen in rosenthal fibers, eosinophilic granular bodies and vessels in the tumor. Mitosis is very rare. Ki-67 index is about 1%. Presence of cellular pleomorphism, nuclear chromasia, vascular proliferation, meningeal spread and necrosis is not symptoms of anaplasia. The main finding of anaplasia is the increase in the number of mitosis.7 In our case, there was an increase in cellularity and vascularity as well as pleomorphism and necrosis in some areas in addition to conventional areas. 3 atypical mitosis in 10 BBA and Ki-67 index about 50% in these areas were interpreted as malignant transformation. There was no RT history in our case. In PAs, the underlying mechanisms in the malignant transformation are not known yet. In the literature, it is reported that all 52 malignant transformation cases had a history of RT.6 Therefore, RT is suggested to play a key role in malignant transformation in PAs. In another publication, anaplastic features were identified in 34 of 2200 PA cases; however, clinical, therapeutic and clinical follow-up data were insufficient in these cases. 4 of these 34 cases had RT history and it is suggested that RT is not the only criteria in the malignant transformation. In the same study, it is indicated that necrosis free anaplastic PA shows similar prognostic characteristics with Grade-II astrocytomas and PA cases containing necrosis show similar prognostic characteristics with Grade-III astrocytomas.8 In another study, it is suggested that cellularity, necrosis, nuclear pleomorphism and intratumoral hemorrhage seen in glioblastoma multiforme are not evidence of poor prognosis or malignancy in PA.1,9 There was significant increase in the number of mitosis and Ki-67 index in our case. In another study, a 1-year old case diagnosed with a mass in the posterior fossa has shown no progression during the 6-year clinical and radiological follow ups and was not monitored after 7years of age. However, the patient was diagnosed with PA with malignant characteristics at 21years of age. Therefore, it is suggested that the primary tumor in the case can be PA and it can show malignant transformation spontaneously in the past 20 years with no treatment. Malignant transformation is suggested to be developed during the natural clinical course of tumor.10 In our case, the lack of RT history shows that unexplained factors play a role in malignant transformation and the underlying mechanisms should be clarified. In this field, further clinical studies and researches are required. The present work was performed after taking informed consent from the patient and a sincere effort has been made to uphold patient confidentiality.
None.
None.
None.

©2017 Findik, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.