Journal of
eISSN: 2373-6410


Literature Review Volume 13 Issue 2
Department of Spine Surgery of the High Specialty Regional Hospital of Puebla, Institute of Security and Social Services for State Workers, ISSSTE, Mexico
Correspondence: José Francisco Sánchez Sánchez, Av. 14 sur 4336, Jardines de San Manuel, 72570 Puebla, Puebla, Mexico, Tel (+52) 222 531 9080
Received: April 05, 2023 | Published: April 27, 2023
Citation: Sánchez-Sánchez JF, Robles-Ortíz RE, Rodríguez-Messina AF, et al. Posterior spinal implant failure and its clinical significance: analysis of two cases and literature review. J Neurol Stroke. 2023;13(2):42-44. DOI: 10.15406/jnsk.2023.13.00542
Background: The goal of spine arthrodesis is vertebral fusion and stabilization, however there are multiple factors which don’t allow it; among the most known are implant failure and pseudarthrosis. The question is, should a revision surgery must be performed in all implant failures?
Case description: We present 2 cases of screw fatigue or failure which were treated differently based on the symptoms of the patients, even when they had clear radiologic images of implant failure.
Conclusion: The set of signs and symptoms are the pillar for the decision in the definitive treatment, even though the literature mentions bone-implant fusions in less than a year, instrumentation does not always fulfill its objective due to surgical and non-surgical factors; however, we must individualize each case with the aim of maintaining spinal stabilization, preserving neurological function and relieve pain.
Keywords: implant failure, broken screw, fatigue screw, spinal fusion. spinal instrumentation, pseudoarthrosis
Transpedicular screw fixation is the reference technique in the management of lumbar spine conditions, especially in those requiring improved stability and correction of spinal deformities such as spondylolisthesis and scoliosis.1,2 Among the major postoperative complications of spinal instrumentation are screw breakage, broken rods, and screw/rod dislodgement.3,4 In most cases these complications do not require surgical reintervention unless the patients present important pain or neurological symptoms. Furthermore, this situation can be distressing for many patients and revision surgery may be indicated with the aim of improving symptoms.3.4
Matsuzaki et al.3 reported an implant failure rate of 21%; with the evolution of current devices, the failure rate has decreased by 10%. The etiology of implant failure might be due to several factors such as screw location, bone quality, degree of bony fusion, disc height preservation, segmental kyphosis, and pedicle screw design deficiency.5,6 We present two cases, in which the definitive management decision was based on the symptoms of the patients; when reviewing literature, we noticed that some of the series based their treatment by observing implant failure in imaging studies (X-rays and CT); we think that the symptoms should be considered as the most important criteria to avoid unnecessary revision surgeries.
Case 1
61-year-old female, with type 2 diabetes mellitus, spinal surgery in 2017 in which a discectomy and transpedicular instrumentation of L4-L5 was performed. Presented herself into the ER with a history of low back pain and related left leg symptoms which increased with lumbar flexion and extension of 8 months of evolution. Physical examination showed limp gait, left paravertebral muscular contracture, hyperesthesia, and nerve root irritation. Implant fatigue was evident (Figure 1 & 2). A standard posterior approach to lumbar spine was performed, the rods were removed, identifying the fatigue of the right L5 transpedicular screw, the polyaxial head was then removed with a plier to expose the broken screw head. Then, the rest of the screws were removed with torx screwdriver. Subsequently the interbody cages L3-S1 were inserted with TLIF technique in addition to transpedicular instrumentation (L3-L4-S1 right; L3-S1 left) (Figure 3). After surgery, the patient showed an immediate improvement, decreased pain and absence of leg symptoms. She started to walk 8 hours after the surgery, and she was discharged 20 hours later without complications.
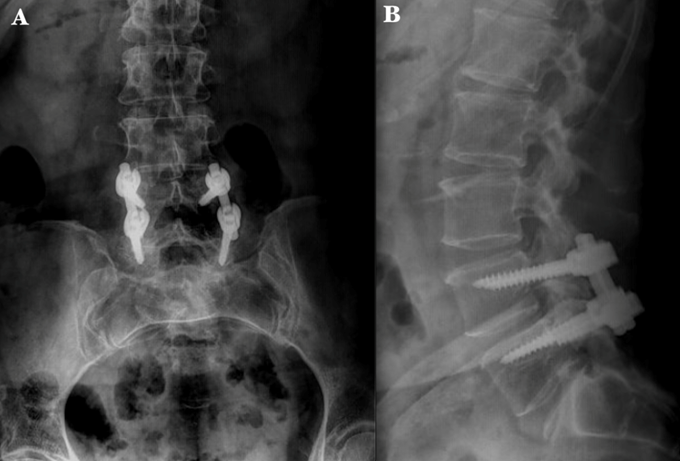
Figure 1 Preoperative X-ray radiographs of the lumbosacral spine. A) Anteroposterior image shows transpedicular instrumentation at the L4-L5 level. B) Lateral image shows the interface area of the transpedicular screw and fatigue of the right L-5 screw..
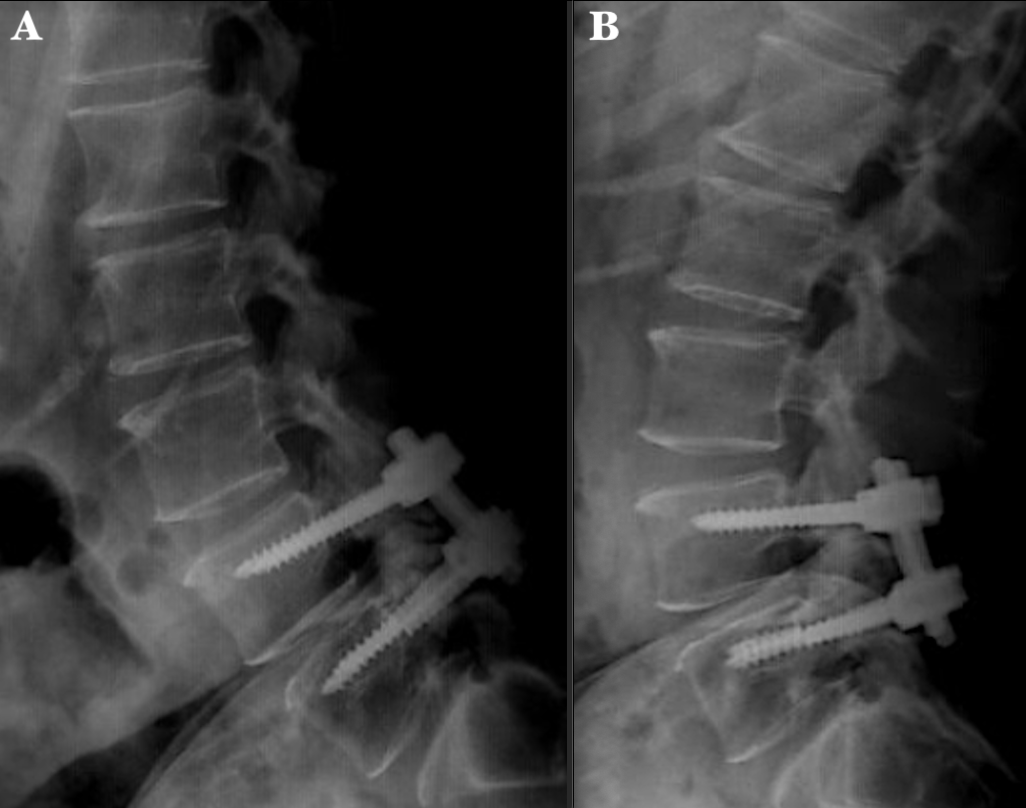
Figure 2 Preoperative dynamic X-ray of the lumbosacral spine. A) Lateral flexion image shows L4-L5 spinal instability. B) Lateral extension image shows a decrease in the foraminal space at the L4-L5 and L5-S1 levels, with displacement of the right L5 screw due to fatigue..
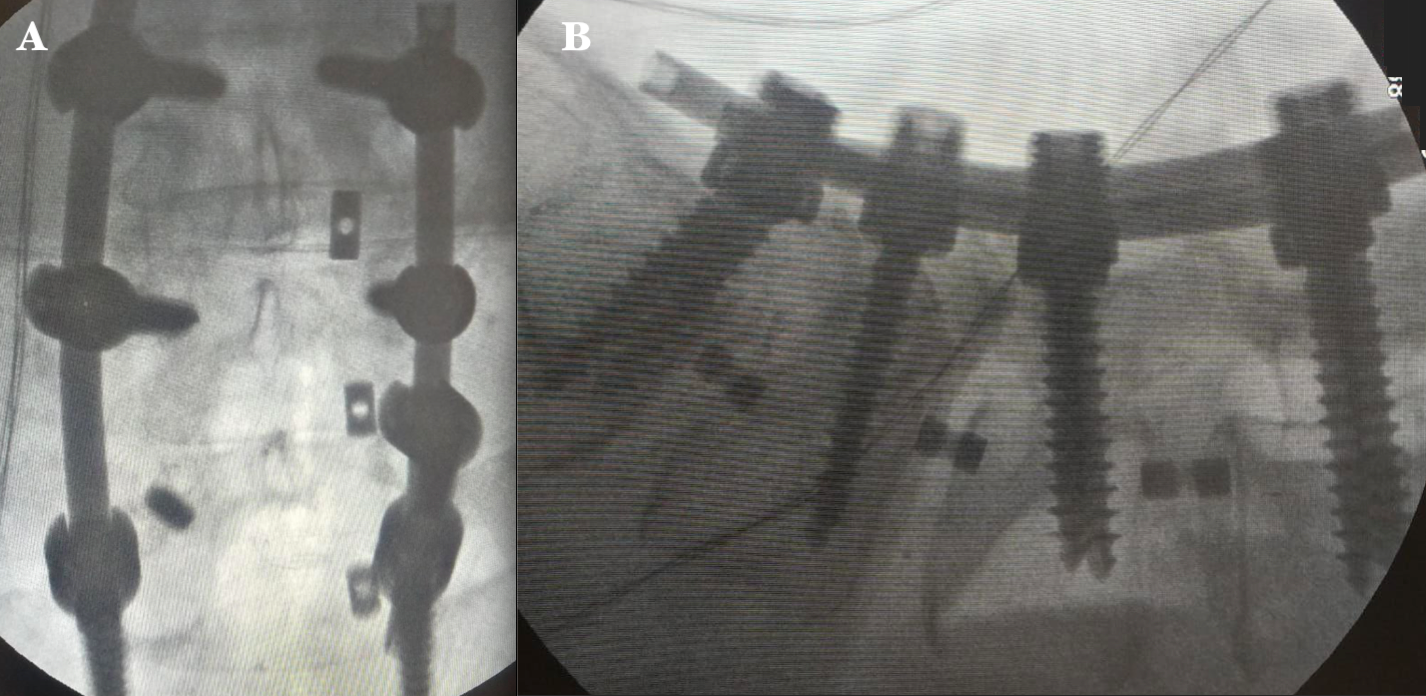
Figure 3 Intraoperative fluoroscopic images A) Anteroposterior image shows the left L3-S1, L3-L4, and right S1 transpedicular instrumentation and the distal portion of the broken L5 screw. B) Lateral image shows proper placement of transpedicular screws and interbody cages at L3-S1levels. .
Case 2
60-year-old male with a history of spondylolisthesis who underwent trough L4-S1 decompression and posterior lumbar instrumentation in 2019. Fourth years postoperative follow - up physical examination revealed a midline surgical scar without abnormalities, mild pain on palpation of the lumbar paravertebral muscles and normal neurologic assessment. Control X-rays were taken showing fatigue of level S1 screws; however, the patient was asymptomatic, therefore, conservative treatment and surveillance were decided, without the need of revision surgery (Figure 4).

Figure 4 X-ray radiographs of the lumbosacral spine. (A) Anteroposterior and (B) lateral radiographs show both S1 screws breakage apparently at the middle level of the length of the threads (6.0x50 mm polyaxial pedicle screws). Interphase is observed at right L4 and L5 screws with no evidence of pull-out..
The aim of spinal fixation is to restore and stabilize the spine when it is affected in one of its 3 columns according to Denis. This condition is mainly caused by instability secondary to degenerative disease, tumor or trauma disease.7 Currently there are several techniques to stabilize an unstable spine; among the most known there is the combined fixation of segmental pedicle screws and rods,8 obtaining good results; however, over the time, the spine might generate new pathologies that require implant replacement surgeries, extension of instrumentation or revision surgeries. Unfortunately, despite having better quality of implants, there are still failures of the secondary system due to breakage or migration of the rods and fatigue or breakage of the secondary screw due to the relationship between fusion-quality of the bone-implant.
Implant failure can be classified according to the time of onset dividing it into early and late failures; early implant failures are those that are clinically, or imaging evidenced in a period < 3 months post-surgery, caused by poor bone quality secondary to neoplastic (tumors, multiple myeloma) or metabolic (osteoporosis) pathologies; meanwhile, late failures are those that occur > 3 months post-surgery secondary to mechanical and fusion-implant causes.9 Implant failure occurs most frequently within the first 6 months post-surgery (90% of cases), caused by several factors, among the most common are pseudoarthrosis or failure of fusion and design of devices; some multicenter studies showed that up to 6.8% of patients suffered this type of complication referring to rod breakage as the most frequent presentation.8,10,11 The incidence of pseudoarthrosis is observed in 3-83% (average 24%), mostly found in the transition sites, and mainly affecting the thoracolumbar region;11–14 this process demonstrates a continuous tension on the implants, leading to fracture or loosening of the instrumentation.10 The series of Hofler et al.15 and How et al.16 reported a 1.4% to 6.3% risk of developing pseudoarthrosis that required revision surgery depending on the main disease (long instrumentation, spinal deformity respectively). This complication stems from two causes: surgical and non-surgical. The most important surgical causes for developing pseudoarthrosis are inadequate screws fixation and long instrumentations (>6 levels);9,15,16 meanwhile, the non-surgical causes involve age >55, smoking, prolonged use and high doses of steroids and rheumatological diseases leading inadequate bone formation.15,16
Another important factor of implant failure is the design of the devices, however, let us remember that it is a vicious circle in which pseudoarthrosis affects fusion and devices increase the risk of pseudoarthrosis. The bone-implant fusion process can be generated on an interval of 3 to 12 months (average 8 months), therefore, the support system should be maintained with a lower degree of stress-tension during that period, until its consolidation.11,13,17 The design of devices or implants is important for stabilization and avoidance of fatigue.13,17 The incidence of screw breakage or fatigue is 1% to 11.2%.6,12 In previous studies it was considered that the rupture of the screw was mainly proximal to the head of the screw, however current studies of biomedical engineering show that the rupture is mostly observed in the distal portion of the screw head (between the portion without support and the pedicle).13,17 Among other factors independent of the material and design of the implants, the position and orientation of the screws were assessed; incompletely inserted screws have an increased risk of fatigue;13,17 La Barbera et al. demonstrated an increment in tension up to 40-50% on the screw and 11% on the rod in those systems without a screw length support of 2.3mm compared to those where the screws were fully inserted.17 Due to the incomplete insertion of the screw, a decrease in resistance of 20 N has been observed for each exposed thread increasing the risk of fatigue.13 The concentration of force and distribution of tension is found at the ends of the instrumentation, being the caudal screws the most affected.12,13 Implant fatigue is also exerted secondary to high-energy impacts and repetitive aggression or hyperflexion movements, decreasing the useful life of the implant and therefore the probability of fusion.13 These complications can affect the daily activities of the patients due to the loss of correction of the deformities and neurological alterations that can compromise the integrity of the nerve and its function; pain being the main cause of consultation;7,8 therefore, these cases presenting the after mentioned characteristics are candidates for revision surgery. On the other hand, the absence of neurological symptoms and pain are important characteristics for the treatment decision, being surveillance and medical management the ideal treatment in these cases.10
There are currently many techniques for the removal of the affected implants, if the broken screw fragment is inside the pedicle, it can be extracted by drilling the screw;7 if there isn’t enough space in perpendicular position for the insertion of a new screw, it can be treated by drilling at the inferomedial point of the pedicle for a new placement (of a longer screw with a larger diameter, without exceeding a 70% of the treated pedicle diameter to avoid its rupture), treating it below the broken fragment (above L5 levels)7,12,14,18 or a making a vertebral spinal fusion bridge of the affected level; in some cases where S1 screw fatigue is found, a similar technique can be performed with the removal of the screw after its drilling until the broken surface of the screw is discovered and can be removed with a screwdriver and reposition another one into an anteromedial or tricortical direction towards the sacral promontory. If the screw cannot be removed in this segment, 1) place an anteromedial screw directed to the broken screw (this will depend on the direction of the first screw) 2) Avoid the S1 pedicle and insert the screw in the sacral alar or 3) placement of iliac screws.6,14,18
It is important to assess the amount of bone resection that will be caused to remove the screw, since the pedicle can be weakened and cause an inadequate grip of the implant with the possibility of developing screw fatigue again. Some factors that must be considered to avoid the failure of a double screw placement on the pedicle is the orientation of the broken screw and the diameter.6,18
In case 1, the patient presented progressive pain with VAS 8/10, so we decided to perform the revision surgery considering to bridge the right L5 level, and perform a transforaminal lumbar interbody fusion (TLIF) with posterior fixation (level L3-L4-S1 right and L3-S1 left); it immediately improved stability and pain that occurred with flexion and extension. On the other hand, our case 2 patient has maintained pain control with medication and physiotherapy only, it was demonstrated a definitive radiological failure of the implant, without the need for revision surgery; due to the time passed between the placement of the instrumentation and the follow up, our patient had already presented bone fusion, allowing us to maintain him with a conservative treatment.
The literature has mentioned high rates of failure in spinal implants between the first 6 months, therefore, we must consider telling our patients the importance of care and postsurgical recommendations to avoid early ruptures, and allow allowing a complete fusion after the year of instrumentation. Also, a physical preparation must be considered to strengthen the paraspinal muscles (erector spinae and multifidus muscles) at least 3 months before surgery and individualize the definitive treatment based on the symptoms of the patients; we have to take in consideration that a revision surgery increases morbidity as well as transoperative and postoperative risks. Clinical evaluation is the basis of the treatment, and as pain being the most frequent cause of consultation of the Spinal Surgery Department, we should provide greater benefits in those cases which reintervention is offered, with the aim of maintaining spinal stability, sagittal balance, neurological improvement, and pain relief.
The authors declare no conflicts of interest.

©2023 Sánchez-Sánchez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.