Journal of
eISSN: 2373-6410


Research Article Volume 9 Issue 2
1Department of Neurosurgery, Royal medical services, Jordan
2Department of Endocrinology, Royal medical services, Jordan
3Department of Radiology, Royal medical services, Jordan
4Department of Histopathology, Royal medical services, Jordan
5Department of Interventional radiology department, Royal medical services, Jordan
6Department of consultant pediatric nephrology, Royal medical services, Jordan
7Consultant neurosurgeon, Royal medical services, Jordan
Correspondence: Rami Alqroom, MD, FACS, Consultant Neurosurgeon-Spine surgeon at Royal Medical Services- King Hussein Medical Center, Jordan
Received: March 13, 2019 | Published: April 11, 2019
Citation: Alqroom R, Suzan E, Qamar M, et al. Posterior fossa-”Sin City”: tumors debriefed and cardinal epidemiological features illation. J Neurol Stroke. 2019;9(2):91-94. DOI: 10.15406/jnsk.2019.09.00354
Objectives: Posterior fossa tumors are the most frequent neuro-oncological pathology in children. The current review, as a supplement to other published works, aimed to use a retrospectively collected data registry of surgically treated cases of posterior fossa lesions to primarily delineate the relative frequencies of tumors patterns in our setup. Special emphasis was given to analyzing the cardinal epidemiological features.
Methods & Patients: This retrospective review was conducted under approval by the institutional ethical committee. The institutional patient database of 201 patients who underwent surgical intervention by the Department of Neurosurgery in a single referral center (King Hussein Medical Center) over a 15years period from January 2002 to January 2017 was scrutinized.
Results: The study population after applying the exclusion criteria was 201 patients with a male: female ratio of 1:1.1. Most (61.7%) of the posterior fossa tumors involved children <14 years with 23.9% in children <5 years. The most common clinical presentation was the significant increase in intracranial pressure. Cranial nerve involvement was observed in 2.6% of the cases. The general surgery-related complication rate in our study was 41.29 %, affecting 83 patients. The overall surgical-related mortality rate was 6.47% in 13 patients.
Conclusions: Posterior fossa tumors, known for high morbidity- and mortality-related complications. Female children were more affected with tumours. Clinical demonstration is insidious with a significant increased intracranial pressure. Evolution in treatment options offers great improvement in survival with very low recurrence rates.
Keywords: posterior fossa tumor, hydrocephalus, endoscopic third ventriculostomy, medulloblastoma, mutism
Posterior fossa tumors are the most frequent neuro-oncological pathology in children and are one of the most cataclysmic forms of human illness. It has been reported that >60% of the posterior fossa tumors occur in children.1‒4 The close vicinity of these lesions to the nearby brainstem and fourth ventricle explains the common presentation of these patients who show a significant increase in intracranial pressure, obstructive hydrocephalus, and cranial nerve involvement in about 80% of the cases leading to herniation and death.5–8 Innovative evolutions in radiological modalities and treatment options have promised about a great improvement in survival in these patients over the past few decades.1,9‒11 Large multi-institutional reports exemplifying the epidemiology of posterior fossa tumour surgery, especially in developing countries, are lacking.12 The current review, as supplementary to other published works, aimed to use a retrospectively collected data registry containing surgically treated posterior fossa lesion cases in order to delineate the primarily relative frequencies of tumour patterns in our setup over a period of 15years. Special emphasis was devoted to cardinal epidemiological feature and major concurrent issue analyses.
This retrospective review was conducted under approval from the institutional ethical committee. The institutional patient database containing 201 patients who underwent surgical intervention by the Department of Neurosurgery in a single referral center (King Hussein Medical Center) over a 15year period from January 2002 to January 2017 was scrutinized. Clinical records, in addition to computed tomography (CT) and magnetic resonance imaging (MRI) reports, operative notes, follow‑up records and histopathological reports were obtained and analyzed for all patients. Patients with ages ranging from 1 to 58years were included in the study. Patients with posterior fossa metastasis were included, and 67 patients with insufficient data were excluded.
The study population after applying the exclusion criteria included 201 patients; 104 study subjects were females, and 97 were males yielding a male: female of 1:1.1. Age analysis of patients showed that 61.7% of posterior fossa tumors involved children <14years with 23.9% in those <5years. The most common clinical presentation of posterior fossa tumors is the significant increase in intracranial pressure. Headaches and vomiting were the most common presenting symptoms with symptom duration of ranging between one and 16months (16months in extreme cases). Cranial nerve involvement was observed in 2.6% of these cases. All of the patients had CT and MRI-based radiological studies (Figure 1). Symptomatic hydrocephalus was evident in 183 cases as the primary presentation, a pre-operative ventriculo-peritoneal shunt was inserted in 47 cases while 136 cases underwent endoscopic third ventriculostomies (ETV), and 21 post-tumor resection cases needed shunt procedures. All patients underwent surgical intervention using a posterior craniectomy with tumor excision. Several histopathological patterns were recognized and documented:
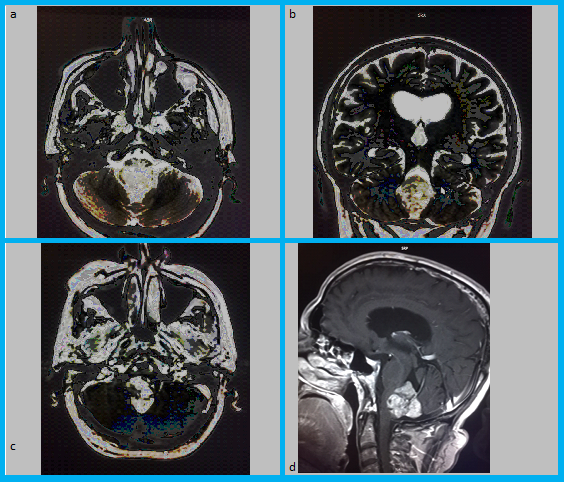
Figure 1 A & B) T2WI axial and coronal demonstrate a lesion with lobulated margins filling the middle and inferior aspects of the fourth ventricle, lesion appears heterogeneously hyper to iso intense in T2WI with multiple small cystic components, extending into the foramina of Magendie and Luschka. C& D) Axial and sagittal T1WI post contrast shows heterogeneous marked enhancement. (EPENDYMOMA)
Adjuvant therapy was applied according to standard guidelines. The general complication rate in our study was 41.29 %, affecting 83 patients (Figure 3). Overall, 28 patients had a second operation/resection during the follow-up within 1 to 68 months. Seven of these patients also underwent a third resection after during a 1, 6, and 11-year follow-up. Decisions for repeat surgeries were based on clinical condition severity and/or progression based on radiological images (MRI-based indications of an increase in tumour residual). The overall mortality rate related to surgery was 6.47% occurring in 13 patients.
Research is currently dedicated to eliciting more extensive information about posterior fossa lesions since this area shows dissimilar mass lesions presents divergent clinical and pathological manifestations. The clinical representation depends on the tumour site and aggressiveness, biological behavior, and growth rate. Clinical manifestations vary from non-definite symptoms such as headache and vomiting to more intense and serious presentations such as lower cranial nerves palsies and ataxia due to direct nerve involvement or nerve compression.1,3,13 In our study, the most common clinical presentation of posterior fossa tumours was a significant increase in intracranial pressure. Headache and vomiting were the most common presenting symptoms followed by cerebellar symptoms.
The value of radiological imaging used for defining the diagnosis based on medical history and physical exam is of the utmost importance. All patients underwent CT and MRI and other specific relevant studies if needed (Figure 4). In our study, these radiological studies were sufficient and appropriate for considering and planning surgical management in all cases.
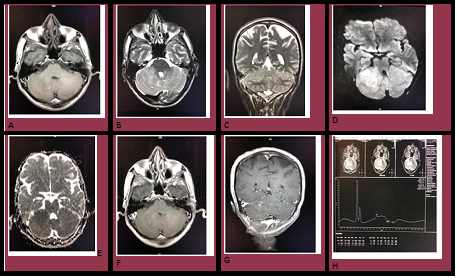
Figure 4 Radiological study showing the different sequences to confirm the diagnosis, A) Axial T1WI: subtle irregular hypo-intensity in the right cerebellar hemisphere. B&C) Axial and coronal T2WI: demonstrate poorly demarcated intra axial subtle heterogeneous hyper intense lesion in the right cerebellum, causing mass effect on the right side of the lateral ventricle, with extension into the right middle cerebellar peduncle, no internal cystic nor hemorrhagic components are seen, No significant surrounding edema, D&E) Diffusion study: high DWI signal with low ADC signal indicating restricted diffusion, F&G)Axial and coronal T1 post contrast: the lesion exhibits faint spotted enhancement, H) Multivoxel Spectroscopy study: there is choline peak with high cho/cr value, low NAA, consistent with high grade lesion.
Due to the limited space in the posterior compartment, all lesions were addressed utilizing surgical intervention, which consisted of a posterior craniectomy with tumour excision executed on urgent basis. Addressing the associated hydrocephalus in these cases is the major issue. In our review, symptomatic hydrocephalus was evident in 183 cases as the primary presentation. A pre-operative ventriculo-peritoneal shunt was inserted in 47 cases while 136 cases underwent ETV, and 21 post-tumour resection cases needed shunt procedures.1,2,5,7
A wide variety of histological subtypes were seen, each requiring tumour-specific treatment approaches. The most recent histopathological classification (2016) confers a combination of both histological and genetic conclusions.14‒16 In our study, heterogeneity of pathological patterns due to the diversity of cells of origin was identified (Figure 2). In our management armamentarium, adjuvant therapy is a cornerstone for achieving better results and longer survival rates. We followed the standard guidelines specified for each tumor. As a result of long-term follow-up, the collective complication rate in our study was 41.29%, affecting 83 patients. The cardinal complications encountered were post-operative hydrocephalus, cerebellar mutism, cerebrospinal fluid leak, and wound infection (Figure 3). All cases were treated expectantly.
Posterior fossa tumours are considered a challenge as all patients experience the same type of signs and symptoms. The nature and severity of the deficits show a discrepancy between patients with both patient and treatment dynamics affecting the ultimate outcomes.
Posterior fossa tumours are one of the most overwhelming neuro-oncology diseases and are well-known for their high morbidity- and mortality-related complications due their vicinity to vital neurological structures and the delicate population involved. Female children were more affected than males. Clinical demonstration is insidious with a significant increase in intracranial pressure and cerebellar symptoms. Innovative evolutions in radiological modalities and treatment options have promised a great improvement in survival with very low recurrence rates due to a feasible gross total excision.
This study has several limitations. First, a quantitative analysis could not be established due to great heterogeneity in the included studies, different patient populations of different ages, and multiple tumour subtypes.
We are planning more detailed appraisals for each encountered histological pattern and clinical manifestation. The diagnostic approach for brain tumors is changing significantly.
None.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Authors disclose no external funding sources.

©2019 Alqroom, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.