Journal of
eISSN: 2373-6410


Case Report Volume 12 Issue 5
1Psychiatrist, Health region of the province of Herrera, Panama
2Psychiatrist, National Institute of Mental Health (INSAM), Panama
Correspondence: Jesus E Amador L, Psychiatrist, Health region of the province of Herrera, Panama
Received: September 23, 2022 | Published: October 7, 2022
Citation: Amador LJE, D’orcy E. Porencephalic cyst due to encephalomacia with neuropsychiatric symptoms and epilepsy: a case report. J Neurol Stroke. 2022;12(5):165-167 DOI: 10.15406/jnsk.2022.12.00519
Porencephaly is a rare pathology and is commonly due to an encephalomalacia lesion. Both have two types: congenital or acquired, causing neurological symptoms and/or disorders such as epilepsy, intellectual disability, cognitive difficulties or impairment, and depressive-type neuropsychiatric symptoms, irritability, behavioral changes, and psychosis. Symptoms will depend on the size and location.
Objective: Expose clinical data; and diagnostic and therapeutic methodology.
Case: We present a 44-year-old female patient; with a personal medical history of epilepsy and neurodevelopmental disorder, who has a history of aggression and frequent seizures. Neuroimaging was performed, finding an injury due to encephalomalacia and, by neurological evaluation, it has an impression of porencephaly. Through laboratory tests, electrophysiological studies (electroencephalogram), neuroimaging and clinical evaluation. It is decided to present the clinical characteristics found in the patient who required management with antiepileptic, mood stabilizer and psychological - occupational therapies with gradual improvement of her admission symptoms.
Keywords: porencephaly, neuropsychiatry, encephalomalacia, epilepsy
Porencephaly is a brain disease characterized by single or multiple cysts or cavities filled with brain fluid in the brain parenchyma. It is rare and is classified into two types: congenital and acquired. If it is acquired, it is characterized by cerebral infarction, trauma, hemorrhage, infection of the cerebral parenchyma and idiopathic causes.1 Causing a cystic degeneration and encephalomalacia leading to a porencephalic cystic formation. They commonly occur from a focal encephalomalacia due to a localized brain insult during early gestation.2
Encephalomalacia is the loss of brain tissue after cerebral infarction and ischemia, infection, head trauma, or other injuries.3 These injuries most are seen in infants and children; but rare in adults. Most of the symptoms will depend on the size and location4 with neurological disorders and/or seizure disorders.3,5 With manifestations commonly hemiparesis and epilepsy,4 signs and symptoms of porcencephaly usually appear in the first year of life which are spasticity and epilepsy2 and other symptoms have been observed such as: cognitive deficits with variation from mild learning disability to severe mental disability,4 language difficulties, motor deficits2 and some psychiatric symptoms such as psychosis4,6 and in a clinical case with an outburst of anger.1
In adults with encephalomalacia there are rare cases reported with psychiatric morbidities in the progressive form of mental decline, borderline dementia, depressive-like symptoms, delusion and oedipism.3 There is no specific treatment, these varies from surgery and drugs;1,7 however, several studies emphasize symptomatic management, aimed at the stage of development in which it is diagnosed; general physiotherapy, speech therapy and long-term positive behavioral support tend to be the pillars7 and psychological therapies8 as well as the benefit of behavioral and cognitive therapies, body - mind and educational interventions as in patients with epilepsy to improve quality of life.9
In this clinical case we present a 44-year-old patient with aggressive symptoms, irritability and epilepsy possibly associated with porencephalic cysts due to encephalomalacia. In Panama, so far there is no record of these pathologies have been found, for which this case report is presented for the medical literature.
This is a 44-year-old female patient with a pathological personal history of epilepsy, intellectual disability and sequelae of poliomyelitis. With a history of aggression and frequent seizures. From the home of Mother Teresa of Calcutta located in Panama City. She is admitted on 10-27-14 in the National Institute of Mental Health of Panama(INSAM). With stable vital signs and without alterations in laboratory tests and ECG. There are no perinatal history data. We only have what was investigated by social work, recorded in her file and the data that the patient tells us. Born in the province of Chiriquí, she has indigenous descent (Ngäbe-Buglé).
Schooling: first grade in elementary school.
First seizure episode at 3 years of age, tonic-clonic with spontaneous remission during childhood. Recurrence of seizures at 16 years of age, coincides with menarche. It is recorded in the file that she was treated by a neurologist and used treatment with various anticonvulsants (carbamazepine, phenytoin, phenobarbital). About the possible polio, she relates ´´since she was 3 years old with symptoms: heaviness, slowness and weakness of the left side of the body and it leaves sequelae. She received outpatient treatment. She does not remember the rest.
She has a history of neurodevelopmental delay, with slurred speech at 2 years of age.
Neuroimaging
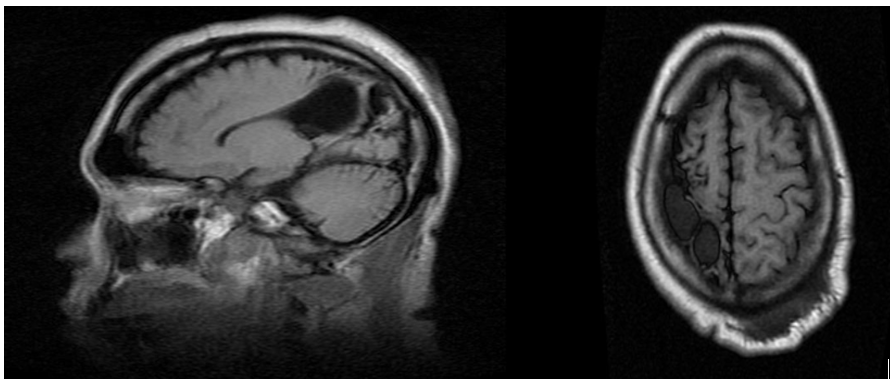
Figure 2 Sagittal and Axial slice.
Lesion that affects the right parietal region, causing an increase in the subarachnoid space, retraction of the wall of the lateral ventricle, and asymmetry of both lateral ventricles due to dilation of the right posterior portion. The preserved intracranial vascular structures where a cystic encephalomalic area is observed that affects the right parietal region, there is a decrease in the entire cerebral hemisphere of that side.
Electrophysiological studies
Cognitive screening and evaluation by clinical psychology
PFEIFFER test
3 errors suspect mild cognitive impairment; but by correction for schooling without suspicion of cognitive impairment.
Test G.V.L. BENDER
Other skills retained
• Some preserved intellectual functions (memory, psychomotricity, language). • Basic language. • Adequate gender identification. • Left dominant hemisphere.
Upon admission to INSAM, She undergoes the following mental exam:
good arrangement, with gait alteration secondary to a sequel to poliomyelitis, a state of awake consciousness, self- and allopsychically oriented, she is attentive to the interviewer, concrete thinking and no alterations in sensoperception are observed.
The patient had a history of being aggressive according to admission history and of several generalized tonic-clonic seizures per month with predominance of relaxation of the sphincters, with a decrease in the seizure threshold associated with minimal stress and it was necessary to transfer her to a crisis intervention unit to stabilize and due to the particular delicate situation of the patient, it was decided to transfer her to a room with better security. Readjustments of the antiepileptic sodium valproic acid (VA) IV every 8 hours and levetiracetam (LVT) IV every 12 hours x 72 hours are made, then when her epilepsy improves, she is switched to oral LVT 1000 mg BID and AV C /6h x 72 hours and then LVT same indication and readjustment of VA to 500 mg orally BID with a good evaluation of the patient, it is decided to omit phenobarbital gradually and it is omitted due to the improvement observed and due to the adverse effects of slowness and sedation. Only with two anticonvulsants were left. Evaluation by neurosurgery was requested where conservative management was decided and re-evaluation by neurology in neuroimaging, the impression of porencephaly is given.
Since 2018, the patient began her participation in the CRPS (psychosocial rehabilitation center) where they emphasize different cognitive and self-esteem areas where she was able to write her full name, reading and writing by association, responsibility, social and spiritual integration and the self esteem. Helping the patient feel better about herself and reducing her stress, which has helped regulate her seizure threshold. Together with a multidisciplinary and interdisciplinary management, the patient has been helped to improve with pharmacological and non-pharmacological treatment (psychological and occupational therapy).
Mental examination after improvement
It is observed with good arrangement and personal cleanliness, cooperative, facies with better adequate facial expressions, awake, alert, oriented in person, place and knows the day, the month; but she does not remember the year, with already known gait disturbance, she observes herself with adequate will, attentive to the interviewer.
language: oral, Spanish, with difficulty in pronouncing certain words, tends to bradilalia. Thinking evaluation her tends to bradypsychia, concrete, denies delusional ideas and denies suicidal ideas at the time.
mood and affect: with adequate affective resonance
Sensoperception: denies sensoperceptual alterations.
critical judgment: the patient is aware of her reality.
Neurological exam
Nystagmus of right predominance stands out, decreased motor strength in the already known left hemibody.
Possible neuropsychiatric symptoms such as the aggression observed in the patient when comparing it with the clinical case of Chaudhury et al, and Dionisie V. et al, were possibly due to presenting lesions in the frontal lobe;1,4 while ours was the parietal lobe but there is no relationship. It is possible to be impressed that perhaps the symptom of aggression was due to the cerebral dysrhythmia in the frontotemporal region. A possible similarity of cognitive difficulty and social dysfunction can be shared, as it was in the case of Pan F et al.6 where the lesion was in the parietal lobe. In addition to intellectual disability, mild difficulty in language and motor deficit as mentioned by Tapadia, S. et al in their case report.2
No other neuropsychiatric symptoms were found in the patient, such as: psychosis and depressive-like symptoms.3,4 What is observed in common is the expected epilepsy , as mentioned by Çetintas E et al, Das J, Tapadia S, et al and Dionisie V, et al.2–5 Especially in the study by Tapadia S et al, where the patient presented a generalized tonic-clonic seizure as our patient.2
Comparing the case of Sisa, M., et al of frontotemporal porcencephaly with a history of poliomyelitis, we are of the same opinion that the history could not be demonstrated due to the absence of studies that confirmed the presence of the virus and to be a possible etiology in our patient.7 We have the impression that the intellectual disability did not progress to overt cognitive impairment because of therapeutic support to improve the patient's quality of life plus the decrease the patient's seizures. The psychological therapies and occupational therapy of the INSAM´s Psychosocial Rehabilitation Center (CRPS) are made up of a multidisciplinary team made up of a psychologist, nurse, occupational therapist and social worker.10 With workshops such as: orchid therapy and medicinal plants for the development of manual skills, art therapy to stimulate people and social integration, self-esteem and fine arts10 compared to what is recommended: by Tencer, J., Agarwal, S. Child Neurology Foundation. physiotherapy, occupational therapy, special instruction and speech therapy,8 Michaelis R, et al., behavioral and cognitive treatment, mind-body therapies and educational interventions9 being important pillars of similar treatment mentioned by Sisa M et al.7
Despite the neuropsychiatric evidence of these types of injuries, more case studies and/or systematic review are recommended in order to reach a consensus. In our patient, symptoms of intellectual disability, motor deficit, slight difficulty in the articulation of words, epilepsy and possible symptoms of irritability or aggression were possibly evidenced, which improved with pharmacological and psychological treatment - occupational therapy to prevent cognitive deterioration that may occur in these cases.
Diagnostic impressions (ICD – 11)
Diagnostic impressions (ICD – 10)
Dr. Elvia D'orcy, psychiatrist. INSAM, Panama
Dr. Fernando Gracia, Neurologist. Saint Tomas Hospital (HST), Panama
Dr. David Sanjur, Doctor in clinical psychology, Panama
Dr. Emelyn Sanchez, Neuropsychologist. Neuropsychology Clinic, Panama
Dr. Mao Rodriguez and the medical team of INSAM, Panama
The staff of the CRPS team of INSAM, Panama.
Dr. Edgar Rodriguez, psychiatrist, Panama

©2022 Amador, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.