Journal of
eISSN: 2373-6410


Case Series Volume 14 Issue 4
1Department of Neurosurgery Federico Lleras Acosta Hospital, Ibagué, Colombia
2Hospital Federico Lleras Acosta, Ibagué, Colombia
3Department of Research Colombian Clinical Research Group in Neurocritical Care, Bogotá, Colombia
Correspondence: Juan Sebastián Reyes Bello, General Physician, N Fundación Universitaria Sanitas, Bogotá D.C, Colombia
Received: July 10, 2024 | Published: July 31, 2024
Citation: Lugo CMR, Alba NAM, Tafur JJE, et al. Percutaneous management of thoracolumbar fractures: a case series. J Neurol Stroke. 2024;14(4):92-97. DOI: 10.15406/jnsk.2024.14.00590
Background: Minimally invasive surgery (MIS) has emerged as a significant advancement in spinal surgery, offering an alternative to conventional open surgery for thoracolumbar fractures. This approach may reduce bleeding risk, infection, and postoperative recovery time.
Aim: This study aims to describe a case series of traumatic thoracolumbar fractures managed using minimally invasive spinal surgery techniques.
Materials and Methods: In this case series an analysis included 11 patients who had experienced thoracolumbar fractures and underwent percutaneous minimally invasive surgery between 2017 and 2022 treated at Federico Lleras Acosta Hospital in Colombia. Fractures were classified using the AO spine classification. Clinical and radiological evaluations were performed with to assess surgical outcomes.
Results: The case series encompassed a variety of fracture types and severities. Patients experienced improvements in pain, neurological deficits, and deformities postoperatively. The visual analog scale (VAS) pain score displayed a marked decline in the surgical cohort as opposed to the conservatively managed patients. Hemorrhage exhibited a remarkable decrease within the minimally invasive cohort, and patients exhibited faster recovery and reduced hospital stays. Radiological assessments showed proper alignment, stabilization, and improved bone healing.
Conclusions: Opting for minimally invasive procedures to address thoracolumbar fractures presents various benefits when contrasted with open surgery. These advantages encompass diminished hemorrhage, expedited recuperation periods, and enhanced pain management. The approach effectively addresses various fracture types, allowing for proper alignment and stabilization. This study substantiates the effectiveness of employing minimally invasive methods for the treatment of thoracolumbar fractures. It highlights the potential for improved patient outcomes regarding pain relief, functional recovery, and reduced morbidity.
Keywords: percutaneous surgery, thoracolumbar fracture, ao spine, minimal invasive surgery
CRP, c reactive protein; CK, creatine kinase; MIS, minimally invasive surgery; TL, thoracolumbar spine; VAS, visual analogue scale
The vertebral column is a bony structure that constitutes one of the main support axes of the body, which also fulfills multiple dynamic and protective functions. It comprises vertebrae divided into seven cervical, twelve thoracic, and five lumbar segments. Its resistance capacity is given by how the vertebrae are organized, being of different sizes depending on the area where there must be greater resistance. This is how the lumbar vertebrae are much larger than the cervical ones since this is the region that needs to bear the most significant amount of force, Ganon et al.1 Spinal cord trauma and precisely vertebral fractures occur when a force exceeds the resistance of the vertebrae. The leading cause is polytrauma,2 with the thoracolumbar vertebrae the most frequently affected in almost 50%, about 6% present spinal lesions, and approximately 50% some motor déficit.3
When evaluating the severity and extent of the fracture, it is necessary to establish the best type of treatment for traumatic pathology of the thoracolumbar spine, which is why there are classifications such as vertebral AO, ASIA4 that determine or not the need for a surgical approach. Two approaches have been defined for treating these fractures: open or conventional surgery, and today, the minimally invasive method is on the rise.5 Here, a discussion begins regarding the best approach to be carried out on a patient. It is for this need that multiple authors have carried out comparative and descriptive studies of both techniques, as is the case of the study provided by Guiroy et al.3 or of Kreinest in the assessment of postoperative complications and perioperative data following either open or percutaneous dorsal instrumentation for traumatic fractures in the thoracic and lumbar spine.6 These results have established that minimally invasive spinal procedures represent a valuable and profitable resource today given that allow the stabilization of the spine using percutaneously inserted transpedicular screws with a significant reduction in postoperative complications such as bleeding, pain, and risk of infection, likewise, shortens recovery time by reducing trauma against soft tissues compared to open surgery.7
This retrospective case analysis involving individuals with thoracolumbar fractures received approval from the institutional committee at Hospital Federico Lleras Acosta in Ibagué, Colombia. Patients provided informed consent for the review of their medical records and the publication of anonymous information.
Description of cases
Case 1
A 23-year-old woman with a documented history of multiple traumatic events, hemodynamically stable on physical examination with axial low back pain, pain on palpation of the spinous process, and pain in the rib cage without neurological deficit. Admission images showed fractures of the 6th and 8th thoracic vertebrae, type A2 in the AO spine classification, mild kyphotic deformity taken early to bilateral percutaneous fixation, and fracture reduction with adequate pain modulation after the surgical procedure. The hospital discharged the patient two days after the surgery, with no signs of early complications. Subsequent outpatient visits revealed the patient's favorable progress (Figure 1).
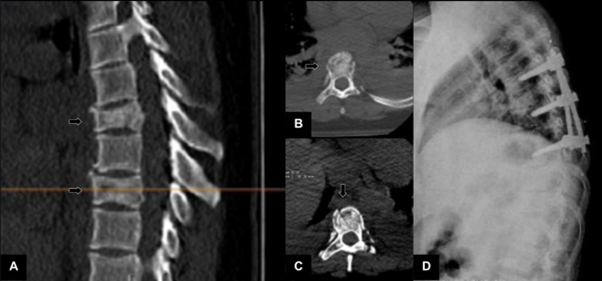
Figure 1 (A-C) Simple thoracic spine tomography showing upper and lower plate fractures of T6 and T8 vertebrae with slight kyphosis deformity. (D) In the postoperative control image on the right, the proper position of the pedicle screws and fixation material is evident.
Cases 2 and 3
A 16-year-old woman with a medical background of pelvic trauma due to a fall from a height. At evaluation, the hemodynamically stable patient had severe lumbopelvic pain and distal paresis of the right lower limb. Neuroimaging showed an A4-type fracture in 4 Lumbar vertebrae with invasion and bone fragments toward the canal. She was considered a candidate patient for L4 corpectomy and decompression + transpedicular fixation by percutaneous technique. The procedure was performed without complications. The hospital was discharged six postoperative days, achieving adequate evolution (Figure 2). In the second postoperative check-up 30 days after medical discharge, there was evidence of improvement in paresis of the left lower limb, the patient walking with progressive improvement of her previous neurological deficit. Case 3 corresponds to a male patient with a fall of 10 meters in height and subsequent trauma to the lumbar spine and lower right limb. The patient presented pain on palpation and mobilization of the lumbar region on physical examination without evidencing a neurological deficit. Images were taken showing a type A4 fracture of the L1 vertebra (Figure 3). He underwent vertebrectomy and percutaneous fixation, achieving adequate alignment and deformity correction.
Cases 4 and 5
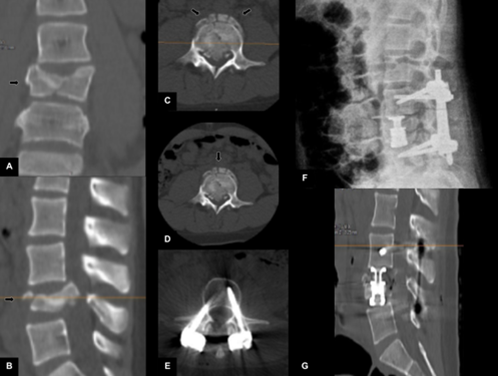
Figure 2 (A-D) Simple lumbar spine tomography showing L4 burst fracture with kyphosis deformity and severe spinal canal invasion. (E-G) Postoperative control images show an intercorporal cylinder in l4 with adequate alignment, canal decompression, and transpedicular screws with good positioning.
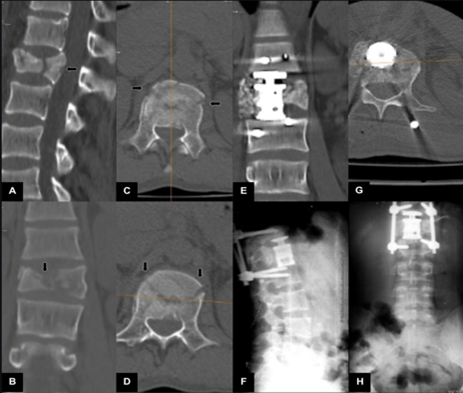
Figure 3 (A-D) Simple lumbar spine tomography showing burst fracture with involvement of the posterior wall of the body of L1. (E-H) Postoperative control images show an interbody cylinder in L1 with proper alignment, canal decompression, and transpedicular screws with appropriate positioning.
These are two male patients with a history of falling from a height; the first is a 31-year-old patient with a medical background of falling from a height of 2 meters while standing in association with right tibia and fibula open fractures. On evaluation, the patient was algic, in regular admission conditions, and had dense paraparesis in the lower limbs. A dorso-lumbar spine tomography showed an L1 fracture with a fragment migrated towards the canal and kyphotic deformity. He is taken to percutaneous fixation, achieving adequate decompression and deformity alignment Figure 4).
The second patient, 20 years old, fell from a height of 7 meters when sliding from a tree, receiving trauma in the lumbar region with impossibility for spinal flexion and lower limb motor deficit. On admission, the neurological examination found a patient with 2/5 dense paraparesis in the lower limbs + abolished bulbocavernosus reflex. MRI and spinal tomography showed a type B2 lesion of L2 with a posterior translation that occupied 90% of the spinal canal. Patient Who underwent L2 corpectomy by percutaneous technique achieving adequate decompression and deformity alignment. Patients in whom partial improvement of previous neurological deficit was evidenced during postoperative controls (Figure 4).
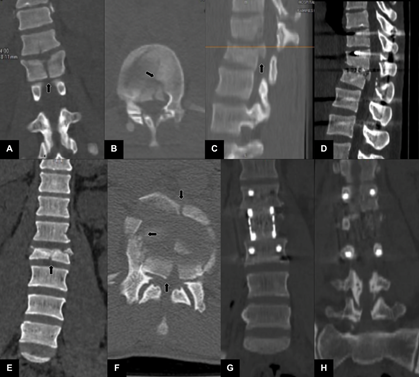
Figure 4 (A-C) Simple lumbar spine tomography showing L4 burst fracture with kyphosis deformity and severe spinal canal invasion. (D) Postoperative control images show an intercorporal cylinder in l4 with adequate alignment, canal decompression, and transpedicular screws with good positioning. (E-F) Simple lumbar spine tomography showing L2 burst fracture with obliteration and damage to the spinal canal. (G-H) Postoperative control images show an interbody cylinder in L2 with proper alignment, canal decompression, and transpedicular screws with appropriate positioning.
Case 6
A 43-year-old man experienced a fall while riding a horse, resulting in subsequent chest trauma, hemodynamically stable on admission with intense pain in the rib cage and on palpation of the thoracic spine. During his hospital stay, the patient underwent closed thoracostomies due to a history of hemo-pneumothorax. After stabilization, he was consulted with the neurosurgery service, showing multiple type A1 and A1 fractures of the T11, T12, and L2 vertebrae (Figure 5). The patient is presented to the neurosurgery board, considering that due to distant fractures, he was a candidate for long percutaneous arthrodesis. The patient underwent an uneventful procedure with adequate recovery and pain modulation in postoperative controls.
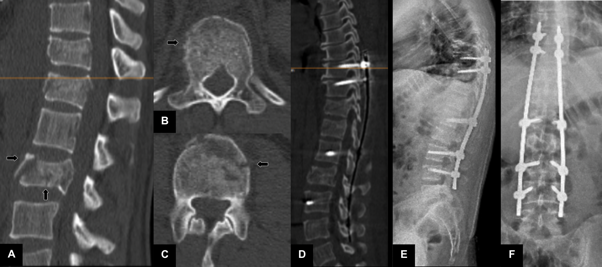
Figure 5 (A-C) Simple lumbar spine tomography showed a burst fracture of L2 and invasion of the spinal canal. (D-F) Postoperative control images show an interbody cylinder in L2 with proper alignment, canal decompression, and transpedicular screws with appropriate positioning.
Case 7
A female patient, 11 years old, was brought to the emergency room of the Federico Lleras Acosta Hospital due to a fall from 8 meters in height, causing trauma to the lumbar region and left heel. On physical examination, the patient had pain, with pain on palpation of the thoracic spine without evident neurological deficit. Column images were taken, evidencing an unstable L2 type A2B2 fracture with a bone fragment in retropulsion towards the medullary canal (Figure 6). She was presented at a meeting of the neurosurgery service, considering the patient to be a candidate for arthrodesis with a temporary internal fixator. The patient is reassessed one year after her postoperative period, evidencing adequate consolidation of the fracture, for which she was considered a candidate for removal of the temporary internal fixator without complications.

Figure 6 (A-D) Simple lumbar spine tomography showing type A3 compression fracture of the L2 vertebral body. (E-G) On the right, postoperative control images with adequate positioning of the osteosynthesis material and adequate fracture consolidation at 10 months postoperatively.
Cases 8 and 9
The first patient, a 20-year-old, had a past occurrence of experiencing a fall from an elevated position and complained of discomfort in the lower back. On physical examination, there was pain in the lower back, without neurological deficit and adequate sphincter control. A lumbar spine MRI was performed due to suspicion of ligament injury, evidencing an l1 type b1 fracture. It was considered to take the patient for percutaneous arthrodesis with subsequent back pain improvement and return to daily activities without complications (Fig. 7). The second patient, 58 years old, with a history of direct trauma to the lumbar region due to a 3-meter fall, was hemodynamically stable during evaluation without neurological compromise, in whom neuroimaging was performed, evidencing a burst fracture of L2 type A4, Unstable, with 46% invasion of the spinal canal, led to percutaneous fixation and decompression maneuvers by percutaneous technique, achieving adequate alignment and decompression (Figure 7).
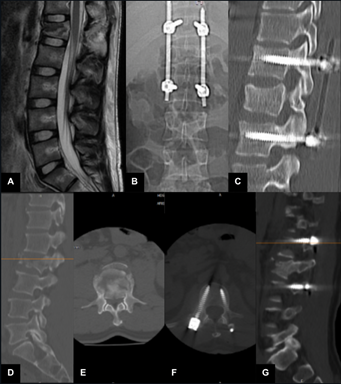
Figure 7 (A) On the left, an MRI of the lumbar spine shows an L1 fracture with ligament compromise is evident. (B, C) Postoperative control images are displayed on the right, showing adequate fixation, positioning of osteosynthesis material, and fracture fusion one year after the surgical procedure. (D, E) L2 compression fracture with spinal canal invasion. (F,G) In the images on the right, proper positioning of osteosynthesis material can be seen by percutaneous technique and fusion.
Case 10
A 24-year-old patient with a medical background of polytrauma due to a traffic accident with low back pain and lumbosacral deformity on physical examination was admitted to the institution two years and months after the event. Neuroimaging showed severe subluxation of L4-L5 with facet diastasis and laterolisthesis with coronal deformity. She was considered a candidate patient for fracture reduction by minimally invasive lateral technique, achieving adequate deformity alignment (Figure 8).
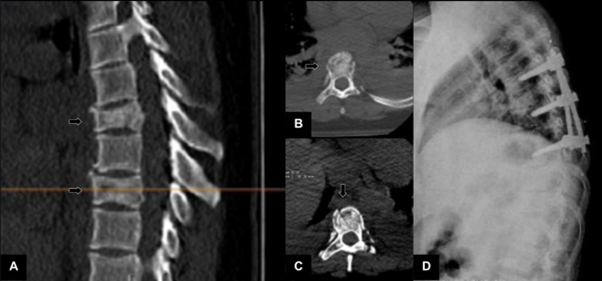
Figure 8 (A, B) On the left, an MRI of the lumbar spine shows evidence of his thesis of L4 L5, CT scan of the lumbar spine showed laterolisthesis and severe coronal deformity of L4 L5. (C, D) Images on the right with osteosynthesis material by percutaneous technique and XLIF box achieving adequate alignment of the deformity and reduction of the fracture. (E-H) Preoperative (I-K) and postoperative images of T11 and T12 dislocation fracture reduction with adequate positioning of osteosynthesis material.
The thoracolumbar spine (TL) extends from the 1st thoracic vertebra and the 5th-6th lumbar spinal segment, and it frequently experiences traumatic spine fractures resulting from high-energy injuries like motor vehicle accidents and falls from elevated positions. The TL region acts as a crucial bridge between the rigid thoracic spine, connected to the breastbone, ribs, and the more flexible lumbar region. This pivotal role is fundamental in spinal biomechanics.8,9 In Colombia, as revealed by a retrospective descriptive study conducted within the city of Cali, 210 cases of thoracolumbar fractures were taken; the most affected sex was male, with a ratio of 2:1, and the age group between 20-45 was the most affected. In 54% of cases, trauma predominantly resulted from falling from elevated positions, with 29% attributed to traffic accidents.10 Such injuries can lead to enduring physical consequences and notable psychological, economic, and social implications.11
A primary and severe consequence of traumatic fractures in the thoracolumbar spine is a spinal cord injury, with an occurrence of 26.5%, with T10-L2 being the most affected segment. These injuries may lead to severe long-term consequences, such as paralysis, discomfort, disfigurement, and impaired functionality.8 Timely treatment of this type of injury can help prevent and recover from neurological damage and avoid post-traumatic deformity.9
For this type of thoracolumbar fracture, there is the classification of the Arbeitsgemeinsschaft für Osteosynthesefrageb Foundation or by its acronym, AO Foundation, founded in Vienna.4 It has created a morphological classification system of the fracture, neurological status, and modifiers. Fractures caused by compression forces produce burst injuries or type A; those caused by distraction forces will cause a transverse ligament disruption or type B; and finally, those caused by axial torsion forces produce rotational deformities or type C.12 There are three categories within each type, and each category includes three subgroups with specific details, being then nine primary groups that will progress in severity and greater risk of neurological injury, the incidence of neurological deficit for type A is 14%; for type B, 32%, and type C, 55% (Figure 9).12
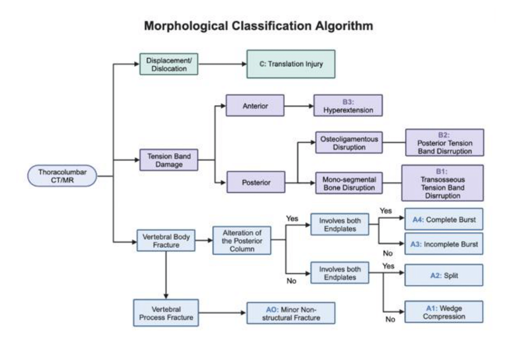
Figure 9 Morphological Classification Algorithm Adapted from Vaccaro, A. R., Oner, C., Kepler, C. K., Dvorak, M., Schnake, K., Bellabarba, C., … Vialle, L. (2013). AO Spine Thoracolumbar Spine Injury Classification System. Spine, 38(23), 2028–2037. Modifications were made to enhance clarity and emphasize specific injury types.
Among the main surgical techniques to stabilize TL vertebral fractures is the traditional open surgery; through a posterior approach over the midline, intervention is related to a more significant loss of blood, longer operative times, and a greater risk of infection of the operative site.9 On the other hand, as a beneficial alternative, minimally invasive spine surgery (MIS) has been described;
its primary goal is to safeguard the integrity of soft tissues while adhering to the principles of both pressure reduction and stabilization.9 This has been under development for over ten years in order to mitigate the trauma linked to the conventional open approach, which can result in a substantial reduction of blood supply and nerve function.13 MIS also allows internal reinforcement during fracture healing since it allows preservation of the innervation, blood supply, and muscle insertion.14
Evaluating the benefits of surgical versus conservative management, Landi et al. inquired about pain perception according to the pain analogue scale (VAS), the percutaneously treated patients exhibited significantly reduced VAS scores, which tended towards 0.3 months post-operation. In contrast, patients treated conventionally had VAS scores averaging 1.5 at their one-year follow-up, likely due to early mobilization within 24 hours post-operation with no need for rigid orthosis, thereby preventing muscle weakening and atrophy. In addition, prompt function and mobility recovery allow the patient to restore adequate muscle contraction from the early postoperative time.15 Percutaneous surgery patients returned to daily life, worked sooner than expected, were more conscious of the success of the treatment, and recovered more quickly from painful symptoms.15
These results are related to the study developed by Ntilikina et al., in which they implemented a standardized MRI protocol one year after implant removal, measuring the cross-sectional areas and signal intensity provided by the paravertebral muscles, they found that the use of percutaneous instruments is more effective in reducing muscle atrophy than open surgery, they also identified in the image that there was a decrease in the amount of fat build-up in the muscles around the vertebral area with percutaneous approach.16
Some history
The first report on pedicle screws was made by Roy Camille in 1963.17 Subsequently, in 1977, Margaret came up with the technique of placing them percutaneously, mainly for short-term spinal fixation, and then taking them out. It was around this time that Assaker R. et al. made the first report on percutaneous trauma to the thorachis with a mention of pedicle screw.17
However, not all patients are candidates for management with this type of technique since there are relative contraindications for percutaneous insertion of pedicle screws, among which pedicle fractures, fracture of the adjacent body, patients with significant kyphosis as well as people with neurological issues that caused bone fragments to move back and forth in the spinal canal were identified.14,17
Surgical technique description of minimally invasive surgery for treatment of thoracolumbar fractures
This technique involves the placement of percutaneous pedicle screws through a 1-2 cm para-median incision; the adequate insertion site of the screws is confirmed using intraoperative anteroposterior and lateral images. Subsequently, a trocar is inserted, followed by a guide wire, and finally, dilators in ascending size; in this way, the dilators divide the paraspinal muscles without detours, avoiding dissection.9 Open approaches are associated with a high level of morbidity due to the extensive removal of soft tissues, which results in muscle ischemia and nerve injury, which causes pain and subsequent muscle atrophy that leads to a torpid rehabilitation of patients.9
Advantages of percutaneous technique
Saravi and colleagues reported a substantial reduction in intraoperative blood loss, early fivefold less, within the minimally invasive stabilization group when juxtaposed with the open surgery group. Moreover, they ascertained better hemodynamics measurements during the minimally invasive procedure, supporting the notion that this approach safeguards cutaneous tissue integrity more effectively than open surgery.8 Likewise, Kevin Phan included 12 comparative studies demonstrating a significantly shorter duration of surgery, less intraoperative hemorrhage, reduced incisions, lower infection rates, reduced hospitalization duration, and prompt functional rehabilitation of patients.17,18 Furthermore, it facilitates internal bracing throughout the process of fracture healing, ensuring that the injury receives sufficient blood flow and safeguards the correct attachment of muscles.14
Complication rates in this study between 2007 and 2014 concerning the open surgical approach were 14.8%, significantly reduced to 5.3% with a percutaneous surgical procedure.6 The MIS technique improves outcomes regarding pulmonary or thromboembolic complications, short operation time, and little blood loss. It benefits geriatric patients and patients in the context of a polytraumatic event.19 Schmidt OI et al. report that compression of the soft tissue during open approach can cause a lot of histological impairment and microscopic damage due to the pressure of the retractors; therefore, minimally invasive percutaneous stabilization will decrease secondary iatrogenic mild tissue trauma19 in correlation with inflammation indicators such as C reactive protein (CRP) and Creatine Kinase (CK), their values would be lower in blood in the MIS technique compared to open surgery at 24 and 48 h after the operation, indicating less trauma and therefore shorter hospital stay.20 In addition, with an effective recovery of the height of the affected vertebral body (Figure 10).21 Percutaneous fixation causes less damage to the muscles adjacent to the spine compared to open fixation with pedicle screws. It has positive effects on the postoperative performance of the trunk muscles, as demonstrated in their study by Kim et al.22 MIS not only provides a secure, dependable, and efficient approach for thoracic fracture treatment but also offers benefits such as minimizing trauma and expediting the patient's post-treatment recovery.23
The adoption and use of minimally invasive approaches in spinal injuries is expanding rapidly. These techniques feature briefer surgery times, reduced hemorrhage during surgery, diminutive incisions, decreased infection incidents, swift postoperative pain alleviation, and abbreviated hospitalization periods, all while delivering comparable structural stability. Over time, these methods achieve effective kyphosis correction, ensure ongoing spinal fixation, and support successful fusion.
An essential consideration in the context of MIS is experience, which involves a learning curve resulting from decreased tissue exposure and limited visual and tactile anatomical references, which presents a challenge of expertise for the surgeon. Nonetheless, the effectiveness of MIS remains a topic of debate, given the limited research tracking variables over an extended period.
None.
Not applicable.
Ethics approval and consent to participate. Ethical committee clearance was taken before including this case for study.
The authors declare that there are no financial and non-financial competing interests associated with this case. report.
Conceptualization: Maryelena Rodriguez Lopez, Juan José Erazo Tafur, Claudia Marcela Restrepo Lugo; Formal analysis and investigation: Maryelena Rodriguez Lopez, Juan José Erazo Tafur, Juan Sebastián Reyes Bello, Claudia Marcela Restrepo Lugo; Writing - original draft preparation: Juan Sebastián Reyes Bello, Maryelena Rodriguez Lopez, Juan José Erazo Tafur; Writing - review, and editing: Claudia Marcela Restrepo Lugo, Luis Rafael Moscote Salazar, Nelson Alberto Morales Alba; Supervision: Restrepo Lugo Claudia Marcela, Nelson Alberto Morales Alba, Luis Rafael Moscote Salazar.
All authors contributed to the study's conception and design. The first draft of the manuscript was written by Claudia Marcela Restrepo Lugo, Juan Sebastián Reyes Bello, Juan José Erazo Tafur, and Maryelena Rodriguez Lopez, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.

©2024 Lugo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.