Journal of
eISSN: 2373-6410


Case Report Volume 6 Issue 3
1Department of Neurology, Atma Jaya Catholic University of Indonesia, Indonesia
2Department of Microbiology, Atma Jaya Catholic University of Indonesia, Indonesia
Correspondence: Rr Josephine Retno Widayanti, Department of Neurology, Faculty of Medicine, Atma Jaya Catholic University of Indonesia, Jakarta, Indonesia
Received: January 27, 2017 | Published: March 11, 2017
Citation: Widayanti RJR, Tjoa E, Tasia Y, Jati MDN, Vania A (2017) Meningoencephalitis Caused by Epstein-barr Virus in Adult with Lung. J Neurol Stroke 6(3): 00202. DOI: 10.15406/jnsk.2017.06.00202
Epstein-Barr virus (EBV) infections usually cause mild symptoms and resolves spontaneously, however the virus may cause severe complications such as neurological diseases, malignant diseases and myocarditis. Determining a diagnosis requires molecular, serological and imaging procedures. The therapeutic modalities for EBV-related severe organ damage including central nervous system manifestations are still uncertain. We report a 31-year-old man with lung tuberculosis with EBV meningoencephalitis presenting with prolonged fever and altered consciousness. Cranial imaging was consistent with meningoencephalitis characteristics. The diagnosis was made by EBV-DNA amplification in cerebrospinal fluid samples. In this case report, we aim to describe a meningoencephalitis caused by EBV in adult with underlying other organ infection.
Epstein-Barr virus (EBV) infections occur worldwide. By adulthood more than 90% of individuals have been infected and have antibodies to the virus.1,2 Central nervous system (CNS) involvement in primary EBV infection in adults is rare, with less than 8% of cases found. EBV was found as a causative agent in 2 to 5% of viral encephalitis and meningitis cases.3
Involvement of EBV in CNS includes encephalitis, meningitis, cerebellitis, myelitis, plexitis and acute disseminated encephalomyelitis.2,4˗6 This case report aims to describe a patient with lung tuberculosis showing symptoms and signs of meningoencephalitis caused by EBV.
A 31-year-old man was admitted to the emergency room with a history of unconsciousness since the day before admission. He previously had 6 days of fluctuating fever and headache. The patient had some behavioral changes since six days before admission such as deliriousness, incoherence and anxiousness. There were involuntary movements in both his hands. He was diagnosed with miliary type lung tuberculosis (TB) 3 months ago. He was given a regimen of antituberculosis drugs which he consumed for only two months before stopping for one month.
On admission, he was sopor (Glasgow Coma Scale E2M5V2) and his vital signs recorded were blood pressure 110/70 mmHg, heart rate 70x/minute, respiratory rate 32x/minute, and temperature 37oC. There was crackles in right lung examination. In the neurologic examination there was nuchal rigidity, positive Kernig sign, hemiparesis in right extremities, and positive Babinski sign.
Initial investigations including hematologic, liver function, renal function and random plasma glucose did not show any abnormalities, except for a decrease in serum sodium 123 mmol/L. Anti-HIV test was negative, with normal CD4 count, CD 8 count and CD4:CD8 ratio. Serology test for syphilis were normal. Blood culture was negative for bacteria.
The chest X-ray revealed no abnormality at this admission. Contrast-enhanced CT scan conducted on admission was consistent with meningoencephalitis characteristics and hydrocephalus sign was noted. He was diagnosed with TB meningoencephalitis and lung tuberculosis with history incompliance to TB therapy. He was treated with ceftriaxone, the same antituberculosis drug regimen and dexamethasone therapy with tapering dose per week. During observation his vital signs and condition was stable, there was fever only in the first three days of admission.
On the second week of therapy there was no any clinical improvement, thus MRI examination and lumbar puncture were performed. MRI description showed characteristics of meningoencephalitis. CSF examination were normal; leucocyte count 4/µL with predominance of mononuclear cells, red blood cell count 54 cells, protein 51 mg/dL, glucose 54mg/dL and serum glucose 76 mg/dL. Acid-fast stain test and India-ink test were negative. CSF culture for bacteria were no growth. The CSF Polymerase Chain Reaction (PCR) were negative for Herpes Simplex Virus (HSV) 1, HSV II, Varicella Zoster Virus, Cytomegalovirus, Human Herpes Virus (HHV) VI, HHV VII, HHV VIII, enterovirus and TB, but positive result for EBV.
At the third week, the patient had high fever (41,5oC), dyspnea and rhonchi in lung examination. We administered levofloxacin and meropenem, but he died after two days of treatment because of pneumonia and severe sepsis (Figure 1 & 2).
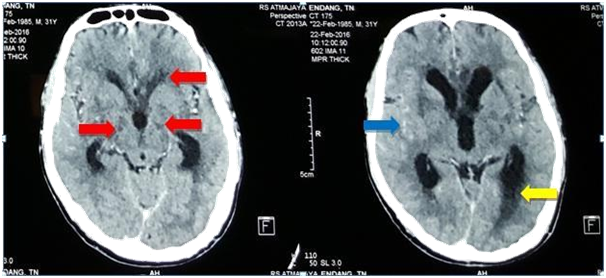
Figure 1 Contrast-enhanced brain CT showed multiple hypodense lesions (red arrows), narrowing of cortical sulci with contrast enhancement (blue arrow), and dilatation of ventricle system (yellow arrow).
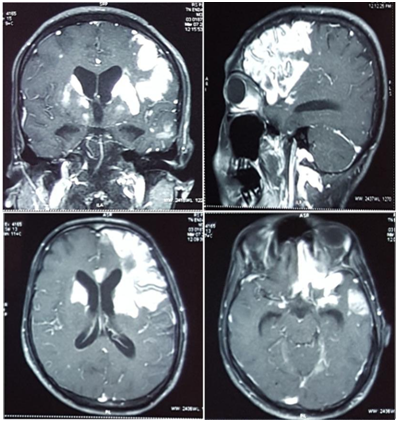
Figure 2 Brain MRI examination showed contrast enhancement in grey and white matter of frontal and left temporal lobe, bilateral uncus, bilateral caudate nucleus, left corpus callosum and bilateral ganglia basalis. There were also contrast-enhancement multiple small lesions in the pons, right and left cerebellum, bilateral cortical and subcortical frontal lobe, bilateral temporal, bilateral parietal, bilateral occipital and white matter of right lateral of periventricular.
Meningoencephaltis is an inflammation of the meningens and parenchyma of the brain.7 This condition is usually caused by bacteria or viruses. HSV-1, VZV, EBV, HIV are often cause of enchepalitis.8 In developing countries-like Indonesia, children acquired the infection in the first years of life. In elderly with decreased immune response, EBV infections are caused by reactivation. Reactivation of latent EBV is clinically important in immunocompromised conditions.9
EBV replicates in B lymphocytes and epithelial cell oropharynx and parotid duct. Infection is most likely spread through saliva, its incubation period is about four to eight weeks. Viruses reach CNS through neuronal or hematogenous paths.9 Pathological finding can be seen in acute condition of viral encephalitis, there are infiltration of mononuclear inflammatory cells in the meningens surrounding the wall of vessels.8 Clinical presentation of EBV meningoencephalitis includes fever, headaches, altered consciousness, meningeal signs, fever, seizure and bizarre behavior.5,10,11 These symptoms was seen in our patient.
Establishing a diagnosis of EBV infection is difficult and requires molecular, serological and imaging techniques. PCR amplification is the gold standard for EBV infection in the CNS. In PCR, both the quantity of EBV and the degree of inflammation (measured by pleocytosis) are measured.4,5 In our case we did not see pleocytosis in the CSF examination, with leucocyte cell count 4/µL. Studies found majority of EBV in CSF of immunocompromised patients.4 We did not do quantitative measurement of EBV and EBV panel test due to resources limitations.
EBV has a tropism is in the deep nuclei, neuroimaging using MRI T2-weighted may show multiple foci hyper-intensity in the cortex, brainstem, thalamus and basal ganglia.6,10 This is consistent with our patient in which we found contrast-enhancement multiple small lesions in several areas of the brain.
The management of neurologic EBV disease depends upon the pathogenesis of the illness and there is no clear consensus for the treatment.4 Some reports suggested that the use of antivirus for severe EBV infection which might be beneficial.10 In our case, we did not give antiviral therapy, but we gave corticosteroid as the adjunct therapy in accordance with the guideline from Infectious Diseases Society of America. Although acyclovir has been used in some cases of CNS disease, it probably provides little or no benefit and is not recommended. Corticosteroids were reported to be helpful in several anecdotal reports of neurologic complications of infection with EBV and have been used in patients with increased intracranial pressure; these data suggest that they may be beneficial in selected patients, but their potential benefits must be weighed against potential risk of perpetuating viral infection or of delaying the diagnosis of or partially treating AIDS-related CNS lymphoma.12
In conclusion, EBV meningoencephalitis is rare. It can be seen in immunocompetent or immunocompromised patients. This case highlights EBV as the causative agent of CNS infection in an adult with underlying other organ infection, lung tuberculosis in this case.
None.
None.
None.

©2017 Widayanti, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.