Journal of
eISSN: 2373-6410


Case Report Volume 2 Issue 5
1Department of Neurosurgery, Super-speciality Hospital (SSH), India
2Department of Psychiatric, Super-speciality Hospital (SSH), India
3Department of Neurology, Super-speciality Hospital (SSH), India
Correspondence: Dr. Furqan A Nizami, Lecturer, Department of Neurosurgery, Super-speciality Hospital (SSH), Government Medical College, Jammu (J&K), India, Tel 919797635348
Received: June 15, 2015 | Published: September 4, 2015
Citation: Nizami FA, Banal R, Reshi V, et al. Isolated oculomotor (Third) nerve palsy: a rare presentation in a patient with bilateral chronic subdural hematoma (CSDH). J Neurol Stroke. 2015;2(5):118-120 DOI: 10.15406/jnsk.2015.02.00068
Introduction: Incidence of bilateral chronic subdural hematomas (CSDH) is less than unilateral CSDH. Conversion of unilateral to bilateral hematomas after surgery is also less commonly seen. Isolated oculomotor (third) nerve palsy in a case of recurrent bilateral CSDH is a rare entity.
Case report: We are presenting a case of isolated third nerve palsy in a patient who has been operated for right sided CSDH about three weeks back. He presented with blurring of vision, ptosis and dilated pupil of right eye and when CT scan head followed by MRI brain was done it revealed recurrent bilateral CSDH.
Intervention: Patient was immediately taken up for the burr hole drainage of bilateral CSDH and patient’s neurological deficits improved in post operative period.
Conclusion: Isolated third nerve palsy is rarely seen in a patient with bilateral chronic subdural hematomas (CSDH). Immediate surgery is associated with good neurological outcome.
Keywords:Bilateral chronic subdural hematoma (CSDH), Oculomotor (third) nerve palsy
CSDH is an encapsulated collection of old blood, mostly liquefied and located between the dura mater and arachnoid. It was first described in the literature by Virchow in 1857 as “pachymeningitis haemorrhagica interna”. Later Trotter put forward the theory of traumatic rupture of bridging veins as a cause of what he named “subdural haemorrhagic cyst”. A history of head trauma is not always essential but trauma has been recognized as an important factor in the development of CSDH.1
Unilateral CSDH are common than bilateral collections. In a study by Nayil et al.2 out of 1181 patients included in their study 86% patients had unilateral and 14% had bilateral collections.
The common presentations of CSDH are altered mental state,3-5 hemiparesis,4 headache,6,7 falls,6 seizures,4 and transient neurological deficits.8 The atypical (uncommon) presentations are isolated neurological deficits, extra pyramidal syndromes and rare neurological syndromes.
Patients with CSDH rarely can present with vertigo and nystagmus,9 upward gaze palsy,10 and isolated oculomotor palsy.10,11 Though isolated third nerve palsy is a common presentation of intracranial aneurysms, diabetes mellitus, CML infiltration, and cavernous sinus lesions. Bilateral subdural haematomas presenting with an isolated oculomotor paralysis, however, without any other notable symptoms or signs except for mild headache, are unusual.10 Increased intracranial pressure causing uncal herniation and stretching of cranial nerves was thought to be the mechanism involved.5,10
We are presenting a 72 year old male patient, hypertensive on antihypertensive medication and a known diabetic on oral hypoglycemic agents since last 5 years. He presented with the history of headache which was not responding to the usual analgesics since last one week and drowsiness since last 2 days. Initial CT scan head (Figure 1) revealed a large right sided fronto-parietal chronic subdural hematoma with mass effect, effacement of right lateral ventricle and midline shift of 10 mm towards left side. Patient was taken up for right sided two burr hole drainage, posterior frontal and posterior parietal under local anesthesia and intravenous sedation. His clinical and neurological condition improved in post-operative period.
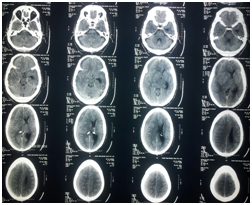
Figure 1 CT scan head showing right sided frontoparietal large CSDH with mass effect and midline shift towards left side.
Three weeks after his first surgery, patient again presented with on and off headache since 3-4 days, visual obscurations and sudden onset ptosis of right eye (Figure 2). On examination right pupil was dilated (6mm) not reacting to light. CT scan head (Figure 3) followed by a MRI Brain (Figure 4) was done which revealed bilateral CSDH. Patient started deteriorating by evening and he was immediately taken up for bilateral burr hole drainage. Patient improved clinically after surgery and his pupil started reacting but ptosis persisted on second post-operative day (Figure 5) but later improved in 2 weeks time (Figure 6).
Chronic subdural hematomas (CSDH’s) are commonly found in elderly patients, as with advancing age the brain undergoes atrophy and leads to approximately 11% increase in the extracerebral space.12 The various predisposing factors for CSDH’s are head injury, alcohol abuse, and coagulopathies.13 A history of head injury is present in 60-80% of patients.14-16 This variation is possibly because of the fact that most head injuries leading to CSDH are trivial; these events are easily forgotten or not actually considered important by patients. In a series by Nayil et al.2 1015/1181 (86%) patients had unilateral collections and 166/1181 (14%) had bilateral collections.
Recurrence is usually seen in multilocular collections. Stanisic et al.12 in a series of 99 patients analyzed the factors that can predict recurrence of the hematomas and found that the laminar separated type of CSDH had a statistically significant correlation with the recurrence of the hematomas. Other factors such as midline shift 5 mm and clot thickness 10mm, and frontal base hematomas, were also associated with high incidence of recurrence. Initial CT scan head of our patient revealed all the three things i.e., multilocular collection, midline shift>5mm and clot thickness>10mm.
One of the most common pathogenic mechanisms of isolated oculomotor (third) nerve palsy is micro-vascular infarction of the nerve, which may be associated with hypertension, atherosclerosis, diabetes mellitus, collagen vascular disease etc.,5,17 Under these circumstances there is usually partial or complete sparing of the pupil.18 In our case, patient did not have papillary sparing. When pupil is dilated and not responding to light reflex, compression of the nerve must be considered, as we know it is the earliest sign of compression.19 The cause of the oculomotor paralysis in our case was presumably pressure of the herniated uncus of the right temporal lobe, a false localising sign, common in raised intracranial pressure due to head injuries and intracranial tumours causing brain shift.5,10
Chronic subdural haematomas may also present this way, usually with other localising signs, impairment of higher mental functions, or a deteriorating sensorium. The fact that only the right third nerve was paralysed led us to believe that the right side subdural haematoma was larger. In fact, the CT and findings at operation showed that both were of similar size. Perhaps slight anatomical variation in the position of the third nerve in relation to the tentorial edges and uncus, and also minor asymmetry of the perimesencephalic cistern explains the lateralization to the right. Rapid recovery of the third nerve after evacuation of the CSDH lends support to our contention that the palsy was due to distortion of the nerve, and not from any other cause.
Isolated oculomotor (third) nerve palsy is rarely seen in a patient with bilateral chronic subdural hematomas (CSDH). Distortion of nerve due to compression seems to be the cause, so immediate surgery is associated with good neurological outcome.
None.
None.

©2015 Nizami, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.