Journal of
eISSN: 2373-6410


Review Article Volume 7 Issue 2
1Universidade Federal de São Carlos- UFSCar - São Carlos (SP), Brazil
2Department of Medicine, Universidade Federal de São Carlos - UFSCar - São Carlos (SP), Brazil
Correspondence: Estela Barbosa Ribeiro, Gerontologist - Master’s student in Nursery for the Nursery Post-graduation Programme at Universidade Federal de São Carlos - UFSCar - São Carlos (SP), Brazil
Received: June 27, 2017 | Published: July 25, 2017
Citation: Ribeiro EB, Terassi M, Rossetti ES, Vale FAC (2017) Instruments of Active Search and Assessment of Memory Complaint. A Systematic Review. J Neurol Stroke 7(2): 00236. DOI: 10.15406/jnsk.2017.07.00236
Introduction: promote an active search for memory complaint states as a means of predicting neuropsychological symptoms in order to propose an initial adequate intervention.
Objective: identify the instruments that address active search and memory complaint and the context in which they were used.
Metodology: systematic literature review conducted in Pubmed-Medline, Lilacs, Scielo, Web Of Science, Scopus, CAPES thesis database and PsycINFO.
Results: 2227 articles were located; the final sample consisted of 27 articles selected by abstracts and after full reading. The analysis allowed identification of 15 instruments. Of the active memory complaint search instruments, 18,6% corresponded to MAC-Q Questionnaire, 14,8% to MFE, 11,1% to PRMQ, 11,1% to McNair, 7,4% to MAC-S and other questionnaires represented 3,7% each.
Conclusion: the instruments pose as a fundamental tool for memory complaint tracking and have been being utilized in the most diverse research scopes.
Keywords: memory complaint, memory, instrument
The older adults population is increasing at a fast rate around the globe. Aging is accompanied by cognitive skills decrease, memory being one of them. The ability to create, retain and use memory is an essential property in individual’s survival.1 Older adults often complaint about mnemonic impairment, although it doesn’t pose as pathological in some cases.2
According to Yassuda et al. 3 diverse hypothesis have been formulated over the past few years to explain memory performance decrease in older adults population. The most recent refers to the idea that attitudes and beliefs interfere negatively in memory. The set of ideas and feelings about memory is known in the literature as meta-memory.3 Some authors state that memory complaints can foreshadow dementia outcomes in older adults.2 Studies highlight the importance of memory complaint in high schooling older adults for early detection of cognitive impairment, due to its non-identification in brief assessments.2,4,5
Memory loss is a frequent complaint for older adults in medical appointments, being reported for 25% - 50% of these individuals.6 Estimates say the prevalence of memory loss corresponds to 46,3% in adults from 50 to 59 years of age and 63,4% for adults from 80 to 100 years of age,.7 Being a female and having low schooling level have also been associated with highest prevalence of memory loss.7 Memory loss due to aging is associated not only to anatomical-physiological alterations, but to cognitive exercise reduction in the learning process as well.5,8 Older adults who are active in learning processes show favorable intellectual and cognitive performance when compared to non-active older adults.5 Reasoning exercises, new information acquisition and daily reading contribute to keep older adults active.5,9
There are two techniques described in the literature to assess memory loss. Questionnaires with experimental tasks that aim to estimate the recordation probability of previously learned information,10 and self-reported instruments that address the experienced memory issues.11 Researches evidence that subjective memory assessments present difficulties regarding real patient’s performance, making it difficult to measure memory issues via objective assessment tests.12 This assessment hardship is associated to the discretion of the tests, the requisition of specialized professionals and the long periods of evaluations.12
On that aspect, this systematic review aimed to identify the active memory complaint search instruments and the context in which they were used. The reason relies in addressing the importance of acknowledging the active memory search instruments by health professionals, since these instruments can help provide an early diagnosis of dementias in older adults, including Alzheimer’s and depression, thus allowing means to a qualified assistance.
Search strategy
Searching occurred during two months - April and May 2014. Databases utilized were Pubmed-Medline, Lilacs, Scielo, Web of Science, Scopus, CAPES thesis database, and PsycINFO, entering the following descriptors: “subjective memory complaint”, “memory complaint”, “questionnaire”, “scale”, “instrument” e “assessment”. The combinations used in the searching were as follows: “subjective memory complaint AND assessment”, “memory complaint AND assessment”, “subjective memory complaint AND instrument”, “memory complaint AND instrument”, “subjective memory complaint AND questionnaire”, “memory complaint AND questionnaire”, “subjective memory complaint AND scale” and “memory complaint AND scale”. Articles published from 2009 to 2014 were considered.
Identification and screening
The criteria adopted for this review included: (1) English, Portuguese or Spanish language; (2) Articles/papers, dissertations and thesis.
Articles selection was blind and independently conducted by two groups of evaluators, and divided into in two steps: 1. Selection by titles and abstracts; 2. Full article reading. Afterwards the groups gathered to assess possible divergences and find consensus according to PRISMA protocol.
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) protocol - presented in Figure 1 - was proposed by Moher et al.,13 to help authors improve communication of systematic reviews and meta-analyses besides using for critical evaluations of published reviews. The duplicated articles exclusion process utilized the Minilist app*.
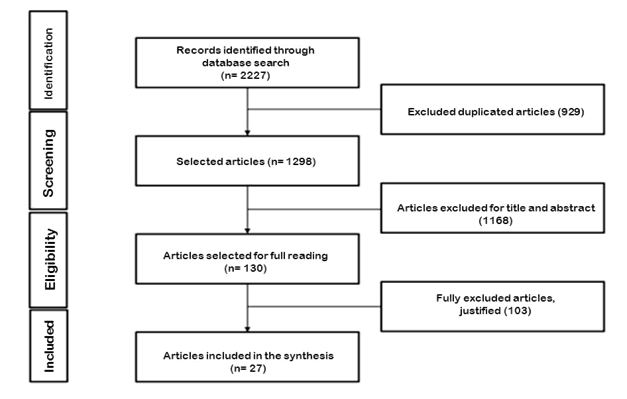
Figure 1 Identification and selection of found articles, according to PRISMA protocol: Source Moher et al.,13
Eligibility criteria
The articles that did not use active search instruments to classify memory complaint were excluded. Three of the found articles utilized questions from validated instruments, but were excluded for not utilizing the instrument as a whole. Two of the found instruments did not assess memory complaint. However, the studies utilized the instruments to characterize their subjects as complainants. Being so, these studies and instruments were considered compatible with the purpose of this paper and gained inclusion in the review.
There were found 2227 articles, of which 929 were excluded for being duplicates. The next step consisted of the exclusion of 1298 articles based on their title or abstract. After these procedures, there were 130 articles left for full reading, of which 103 were excluded for not being pertinent.
The studies selected for the review counted 27, all of them being scientific paper (article) type publications. A total of 15 instruments were found in those articles (Table 1). *App designed to the referred end, by Rafael Campanari (2014). To result analysis end, the articles were grouped by instruments as shown in Table 1. Of the found studies, 22,2% were conducted in Spain, 22,2% in Brazil, 14,9% in the USA, 11,1% in Australia, 11,1% in France, 3,7% in Holland, 3,7% in Canada, 3,7% in Sweden, 3,7% in Switzerland and 3,7% in Germany. The following instruments were identified: Memory Complaint Questionnaire (MAC-Q); Memory Failures in Everyday Memory (MFE); Questionnaire for Subjective Memory Complaints (QSMC) - short version; Memory Complaint Scale (MCS); Prospective and Retrospective Daily Memory Failure Questionnaire (PRMQ); Multifactorial Memory Questionnaire (MMQ); McNair Frequency of Forgetting Questionnaire (McNair); Memory Assessment Clinics-Self-Rating Scale (MAC-S); The Measure of Insight into Cognition - Self-Report (MIC-RS); Corsi Block-Tapping Test (CBT); Hopkins Verbal Learning Test-Revised (HVLT-R); Forgetting Frequency Scale; Evaluation of Balance and Memory Problems (EVATEM); Meta-memory In Adulthood Questionnaire (MIA) and Memory Functioning Questionnaire (MFQ).
Through results analysis it was possible to identify the dominance of the MAC-Q instrument corresponding to 18,6% of the studies, followed by 4,8% of MFE , 11,1% of PRMQ, 11,1% of McNair, 7,4% of MAC-S and 3,7% each of the others. The design of the instruments is presented next.
Memory Complaint Questionnaire (MAC-Q)
Composed of six questions that assess memory complaint in five daily situations, with five different possible answers; scores higher or equal to 25 points are considered indicative of subjective memory compromising, and the maximum punctuation stands for 30 points.14
Memory failures of everyday questionnaire (MFE)
Utilized to assess every day forgetting; it contains 28 items regarding daily life situations and activities with nine possible answers to each item.15
Questionnaire for subjective memory complaints (QSMC) - short version
Brief, reliable and validated questionnaire used to assess memory complaints and to screen for dementia.16
Memory complaint scale (MCS)
Used for memory complaint identification also being useful to differentiate demented from normal older adults. It is composed of seven question, where: No MC (0-2), slight MC (3-6), mild MC (7-10) and accentuated MC (11-14).17
Prospective and retrospective daily memory failure questionnaire (PRMQ)
Composed of 16 questions, it assesses subjective memory. Participants classify how many times each event happened using a five-point scale, ranging from (1) never to (5) very often.18
Multifactorial memory questionnaire (MMQ)
It assesses three dimensions of self-reported memory, including general satisfaction and satisfaction with self-memory capacity (MMQ-contentment), every day memory capacity perception (MMQ-capacity) and the use of every day memory strategies (MMQ-strategy).19
McNair frequency of forgetting questionnaire (McNair)
Participants indicate how often they forget words, people’s names, among other items commonly forgotten punctuating: (0) Never, (1) Sometimes, (2) Frequently, (3) Always. The instrument punctuation score ranges from 0 to 45 points, with higher scores indicating more frequent memory complaints or forgotten items. None of the studies presented a cut point for the frequency of forgotten items, which would be an indication of clinically significant memory deficits.20
Memory assessment clinics-self-rating scale (MAC-S)
Consisted of 45 questions divided into two scales: abilities (21 items), subdivided into numerical recordation, daily tasks, remote personal memory, semantic memory; and occurrence frequency (24 itens), subdivided into semantic memory, attention/concentration, guided memory, general forgetting, facial recognition.21
The measure of insight into cognition - self-report (MIC-RS)
Utilized to assess the report of subjective cognitive complaints in attention, executive functioning and memory. It evaluates difficulty frequency in 12 items, generating a composed score from 0 to 36. The highest punctuation indicates more frequent neuropsychological problems.22
Corsi block-tapping test (CBT)
Assesses attention and memory, particularly attention amplitude and work memory performance. The test consists of a plaque with randomly distributed cubes on it, and is divided into two parts: at first the examiner observes cubes after a predetermined sequence and the assessed subject must reproduce the sequence in the same order; next, the subject must execute the presented sequence without reversing it. The score varies from 0 to 9 points.23
Hopkins verbal learning test - revised (HVLT-R)
Brief learning and verbal memory test with six alternative forms. Ideally used for situations requiring neuropsychological examinations and assessment of abnormal forgetting.24
Forgetting frequency scale
The definitive version of the questionnaire includes four sheets and accompanies two other supplementary sheets: first is the introduction sheet referring to the existence of daily memory lapses experiences including the forgetting frequency scale points one to seven meanings.25
Evaluation of balance and memory problems (EVATEM)
It prospectively evaluates the predictive test values for diagnosis of slight cognitive problems and Alzheimer’s disease in 65+ older adults. If a memory complaint is identified (through a specific questionnaire), the five words test, cognitive disturb examination test and verbal fluency test are applied.26
Meta-memory in adulthood questionnaire (MIA)
It contains 108 questions about individual general memory knowledge, memory processes and tasks divided into seven scales: memory strategies use, knowledge of basic memory processes, anxiety or effort sentiment related to memory performance, awareness of memory changes with age, memory capacity knowledge, and personal control of the ability to recollect.27
Memory functioning questionnaire (MFQ)
Composed of 64 items divided into four scales: general forgetting frequency, severity of forgetting, retrospective functioning and mnemonic use. This instrument does not distinguish prospective memory items.28
Of the instruments found in the selected studies shown in Table 1, only the most important will be addressed here. Studies that classified their subjects as complainants or non-complainants using non-systematic questions from particular instruments, and those which utilized clinical assessments or multidimensional instruments will not be addressed, for they do not refer to a specific instrument, rather to open questions regarding active memory complaint search as in Bartley et al.,29 the study used questions such as the following to assess memory complaint: Do you think you have memory problems? Do you have difficulties remembering conversations?
|
Authors/Year |
Country |
Main objective (MC Related to) |
Age (In Years) |
Type of Study Cut |
|
Memory Complaint Questionnaire (MAC-Q) |
||||
|
Lima-Silva, Yassuda/2009 25 |
Brazil |
Cognitive performance |
56-92 |
Transversal |
|
Morga, John Stevens/2010 30 |
Australia |
Herbal medicine |
≥55 |
Transversal |
|
R Buckley et al./2013 31 |
Australia |
Comparison with AD |
≥60 |
Transversal |
|
Brum et al./2013 20 |
Brazil |
Comparison with MCI |
≥60 |
Transversal |
|
Porto et al./2013 |
Brazil |
Cognitive tests assessment |
> 60 |
Transversal |
|
Memory Failures in Everyday Memory (MFE) |
||||
|
García-Sevilla et al./2014 23 |
Spain |
Effects of training types |
61-81 |
Transversal |
|
Montejo et al./2014 37 |
Spain |
Correlation between humor, episodic memory and health |
65-87 |
Transversal |
|
Montejo et al./2014 38 |
Spain |
Humor e anxiety |
19-60 |
Transversal |
|
Montejo-Carrasco et al./ 2011 |
Spain |
Clinical assessment |
65-89 |
Transversal |
|
Questionnaire for Subjective Memory Complaints (QSMC) - short version |
||||
|
Juncos-Rabadan et al./2012 |
Spain |
Cognitive impairment |
≥ 50 |
Transversal |
|
Memory Complaint Scale (MCS) |
||||
|
Vale et al/2012 17 |
Brazil |
Questionnaire development |
≥ 60 |
Transversal |
|
Prospective and Retrospective Daily Memory Failure Questionnaire (PRMQ) |
||||
|
Eschen et al./2009 35 |
Switzerland |
Initial screening for MCI |
54-91 |
Transversal |
|
Ronnlund et al./2011 34 |
Sweden |
Prevention fundaments |
60-90 |
Transversal |
|
Steinberg et al./ 2013 36 |
USA |
Cognitive performance and psychological factors |
≥ 65 |
Transversal |
|
Multifactorial Memory Questionnaire (MMQ) |
||||
|
Lenehan et al./ 2012 19 |
Australia |
Subtypes of memory complaint |
60-90 |
Transversal |
|
McNair Frequency of Forgetting Questionnaire (McNair) |
||||
|
Brum et al./ 2013 20 |
Brazil |
Comparison with MCI |
≥ 60 |
Transversal |
|
Watfa et al./2010 32 |
France |
Pharmacological treatment and |
60-85 |
Transversal |
|
Kearney-Schwartz et al./2009 33 |
France |
cognitive performance |
60- 85 |
Transversal |
|
Memory Assessment Clinics-Self-Rating Scale(MAC-S) |
||||
|
Adhikari et al./ 2011 39 |
Canada |
Depressive symptoms |
≥ 16 |
Transversal |
|
Ann Pearman/ 2009 40 |
USA |
Personality, depression and health |
19-28 |
|
|
The Measure of Insight into Cognition - Self-Report (MIC-RS) |
||||
|
Gooding et al./ 2012 22 |
USA |
Cognitive rehabilitation for schizophrenics |
± 40 |
Transversal |
|
Block-Tapping Test (CBT) |
||||
|
García-Sevilla et al./2014 23 |
Spain |
Effects of cognitive training |
61 - 81 |
Transversal |
|
Hopkins Verbal Learning Test-Revised (HVLT-R) |
||||
|
Parker et al./2010 |
USA |
Brain function |
≥ 65 |
Transversal |
|
Escala de Frequência de Esquecimentos |
||||
|
Lima-Silva, Yassuda/2009 25 |
Brazil |
Cognitive performance |
56 - 92 |
Transversal |
|
Evaluation of Balance and Memory Problems (EVATEM) |
||||
|
Vannier-Nitenberg et al./2013 26 |
France |
Cognitive tests and falls |
≥ 65 |
Transversal |
|
Meta-memory in Adulthood Questionnaire(MIA) |
||||
|
Visser et al./ 2012 |
Holland |
Instrument development |
± 48 |
Transversal |
|
Memory Functioning Questionnaire (MFQ) |
||||
|
KatjaWerheid et al./ 2010 |
Germany |
Cognitive performance |
± 66 |
Transversal |
Table 1 Studies characteristics and instruments
Morga and Steven,30 & Lima-Silva and Yassuda25 used the Memory Complaint Questionnaire (MAC-Q) in their researches addressing 55+ older adults but no significant results were obtained regarding memory complaint (MC). However, Buckley et al.,31 addressed a population of 1112 60+ older adults, aiming to calculate the transition rates from older adults that were healthy (HOS) to Mild Cognitive Impairment (MCI). Results demonstrated that MC was more severe in MCI patients than in the HOS group. Within the HOS group MC severity was related only to affective variables, whilst in the MCI group it was related only to age. As in Buckley et al.,31 the authors Brum et al.,20 investigated general memory assessment and strategy use among MCI older adults using MAC-Q and McNair Frequency of Forgetting Questionnaire instruments. The MCI participants did not report greater change and forgetting frequencies perception. These findings suggest MCI older adults do not inform precisely or do not perceive their deficits.
McNair questionnaire was also used in Wafta et al.,32 and Kearney-Schwartz et al.,33 studies, both of which addressed hypertensive older adults with MC investigating anti-hypertensive drug action on cognition. As a result, the studies showed that using drugs from the calcium channel blockers class was associated with better cognitive performance, regardless of blood pressure levels, usual cardiovascular risk factors and vessel structure, suggesting a protector effect from this pharmacological class.
Ronnlund et al.,34 examined self-reported daily memory failure predictors using the Prospective and Retrospective Daily Memory Failure Questionnaire (PRMQ) in an older adults population with memory complaints. Results did not evidence relation between the instrument and objective memory. Taken together, these findings are indicative more of a reflection of humor states and personality regarding self-reported memory assessed by PRMQ in an older population than individual differences in memory and cognitive capacity. Eschen et al.,35 and Steinberg et al.,36 assessed PRMQ utility for an initial MCI screening; amongst its findings MCI patients reported greater prospective and retrospective memory deficits. In a healthy older adults sample, the authors described a higher quantity of subjective prospective memory complaints compared to retrospective memory.
Montejo et al.,37 examined the Memory Failures of Everyday (MFE) instrument structure in 19 to 64 year-old participants. Results supported the existence of a structure in the three-factor instrument (do activities, communication monitoring, and recognition) explaining 29,3% of the variance. The first two factors presented high positive correlation between them and a higher association with humor and memory generated complaints. On the other hand, recognition displayed higher positive correlation to age and negative correlation to objective performance memory. García-Sevilla et al.,23 also utilized MFE to assess MC performance in individuals graduated from the memory training programme at Murcia University, Spain. Montejo et al.,38 evaluated the association between MC and health, humor and episodic memory perception. These authors state that a more structured tool like MFE would be strongly correlated to other variables in comparison to non-structured memory complaint open questions (OQ). Based on the findings, MFE appears to be a more precise measure than OQ in detecting MCI predictors.
Vale et al.,17 proposed the Memory Complaints Scale structured questionnaire as an instrument to active memory complaint search in order to investigate its utility to identify dementia in cognitively healthy older adults. Through a random sample extracted from a specialized teaching hospital casuistry, 60+ older adults were selected. The coefficients found for the scale demonstrated to be reliable indicating good internal data consistency and informative properties to the under investigation construction.
Adhikari et al.,39 used the Memory Assessment Clinics Self-Rating Scale (MAC-S) instrument to assess MC in a group of Acute Respiratory Distress Syndrome (ARDS) survivors released from ICU after five years. The instrument assesses subjective evaluations of memory capacity in diverse personal situations. The MAC-S frequency factor is a subjective classification of memory problems occurrence with high test-retest reliability and concurrent validity. As the same, Pearman40 examined the role of several variables in his study with the MAC-S instrument, including personality, depression and health for both objective and subjective memory in young adults from 19 to 28 years old with primary findings being that health problems can affect many areas of healthy functioning including sleep, medicines use and energy, what may directly affect memory functioning. Furthermore, health problems might need constant monitoring changing into the source of anxiety increase and attention dispersion. Therefore, health should be considered an important source of information when memory is assessed and memory problems are reported throughout life.
This review brought evidences that despite the relative variety concerning age and population in the studies here addressed, the findings suggest that realizing an active memory complaint search is a means to predicting neuropsychological symptoms in order to provide initial adequate intervention. Although there is a consensus on properly developed and validated active memory complaint search instruments and their importance as a tool for clinical practice, they should be used carefully, always respecting construction and validation guidelines addressed by the authors and practice guidelines utilized by expert professionals.
Juliana Cerqueira Leite, Mariana Luciano de Almeida, Aryanne Pereira Soares Avalhai, Catia Cristina Thomaz, Keila Francisco Neto de Oliveira, Beatriz Rodrigues de Souza Mel, Zilda Rezende Mota Botan, Daniela Dalpubel, Nathalia Alves de Oliveira, Érica Mestor Souza, Gabriela Dutra Gesualdo and CAPES for financial support.
None.
None.

©2017 Ribeiro, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.