Journal of
eISSN: 2373-6410


Case Report Volume 12 Issue 2
Department of Neurology, University Hospital, Belgium
Correspondence: De Reuck J, Ryvisschepark 16, 9052 Zwijnaarde. Belgium, Tel 0032 (0) 474 652076
Received: December 01, 2021 | Published: March 2, 2022
Citation: Reuck JD. Hereditary hemorrhagic telangiectasia: A case report with unusual findings on magnetic resonance imaging of the brain. J Neurol Stroke. 2022;12(2):21-22. DOI: 10.15406/jnsk.2022.12.00492
We present the case of a young woman with hereditary hemorrhagic telangiectasia and unusual findings on magnetic resonance imaging of the brain. Although no cerebral arteriovenous malformaties are observed on the magnetic resonance angiography, two small isolated hemorrhages are observed in the brainstem, an asymptomatic one in a colliculus superior at the level of the mesencephalon and a symptomatic one in the anterior part of the pons. The lesions are most probably the results of embolic strokes.
Keywords: Hereditary hemorrhagic telangiectasia, magnetic resonance imaging with angiography, brainstem hemorrhages
Hereditary hemorrhagic telangiectasia (HHT), previously called Rendu, Osler, Weber syndrome, is an autosomal dominant disease with an estimated prevalence of at least 1/5000, which can frequently be complicated by the presence of clinically significant arteriovenous malformations in the brain, lunges, gastrointestinal tract and liver.1 They result in acute or chronic bleedings and infectious complications from shunting through these malformations.2 HHT as well as the occurrence of brain abscesses can mainly be related to pulmonary arteriovenous malformations.3 Also a case of subdural empyema as complication of pulmonary arteriovenous malformation has been published.4 HHT can clinically mimic a recurrent portosystemic encephalopathy.5 However, in the majority of cases with HHT cerebral infarctions and hemorrhages are the predominant lesions.6,7 We present a case of HHT with unusual locations of small cerebral hemorrhages in the brain on magnetic resonance imaging.
This 22-year old woman was admitted to the neurological department of the Ghent University Hospital because of the occurrence of sudden occipital headache and vomiting. On admission, the neurological examination, including the fund-eyes, was normal. No nuchal rigidity was present. The computed tomography of the brain did not reveal any lesion. Spinal fluid examination revealed clear fluid with a normal composition. Two days after admission the patient developed diplopia due to a lesion of the left nervus trochlearis. These symptoms disappeared after two days and a short corticoid treatment. The general examination did not reveal any significant pathology, in particular at the level of the lungs. Also no telangiectasias were observed on the skin and on the tongue.
The prior history included spontaneous nose bleedings between the age of 14 and 16 years, treated by cauterization. The prior history also included an aseptic meningitis at the age of 18 years and a transient paresis of the right arm and hand, with negative additional investigations when the patient was 21-year of age.
The mother and grandmother had also frequent nosebleeds with the presence of telangiectesia at the levels of the lips, tong, fingers and stomach. These findings were absent in our presented patient. The magnetic resonance (MR) angiography of the brain showed no arteriovenous malformations (Figure 1). On MR imaging a small bleed was observed in the right superior colliculus at the level of the mesencephalon (Figure 2). Also a small bleed was detected in the left anterior paramedian part of the pons (Figure 3).
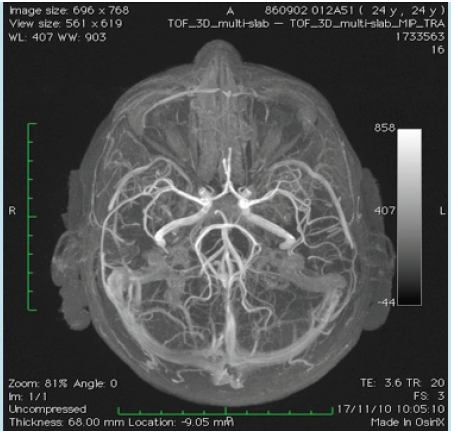
Figure 1 Magnetic resonance imaging with angiography of the circulus of Willis and its afferent arteries. No arteriovenous malformations are detected.
The small bleed in the pons was most probably responsible for the transient diplopia of this patient. On the other hand the small lesion in the mesencephalon was asymptomatic. Asymptomatic strokes occur frequently in HHT.8 The small cerebral lesions are most probable due to embolic strokes, issued from non-detectible pulmonary shunts.9 MRI of the brain with additional spectroscopy allows the distinction between cerebrovascular lesions and brain abscesses.10 The diagnosis of HHT is associated with a significant poor survival rate.11
The author has nothing to declare in relation to this article. No funding was received for the publication of this article.
None.
The authors declare no conflicts of interest.

©2022 Reuck. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.