Journal of
eISSN: 2373-6410


Research Article Volume 3 Issue 1
1Anesthesiology Department, Faculty of Medicine, University of São Paulo, Brazil
2Neuromodulation Laboratory, Harvard Medical School, USA
3Anesthesiology Department, Faculty of Medicine, University of São Paulo, Brazil
Correspondence: LiviaStoccoSanchesValentin, Faculty of Medicine, University of São Paulo, Rua Dr. Enéas de Carvalho Aguiar, 44 543-9 Cerqueira Cesar, Zip Code: 2661-5, São Paulo, SP, Brazil, Tel 551199959215, Fax 55129503298
Received: September 11, 2015 | Published: October 5, 2015
Citation: Valentin LSS, Fregni F, Carmona MJC. Effects of the transcranial direct current stimulation on prevention of postoperative cognitive dysfunction after cardiac surgery: prospective, randomized, double-blind study. J Neurol Stroke. 2015;3(1):1-6. DOI: 10.15406/jnsk.2015.03.00078
Introduction: Postoperative cognitive dysfunction (POCD) is a contrary event observed between 20 to 83%, especially in elderly and after cardiac surgery. Prevention and rehabilitation on cases of POCD may improve the quality of life. The neuromodulator effect of the noninvasive cerebral stimulation has been used in the treatment of brain injuries, depression, and also in the cognitive rehabilitation. The hypothesis is that the use of the transcranial direct current stimulation (tDCS) technique can decrease the occurrence of POCD and cognitively rehabilitate patients submitted to cardiac surgeries. The objective of this study will be to evaluate the tDCS effect over the occurrence of POCD in patients on cardiac surgeries.
Methods: After approval the institutional ethics committee, will be included in the study 138 adult submitted a cardiac surgery. After assigned the consent form patients will be randomly allocated in two groups.
tDCS GROUP: Submitted to 2 daily sessions of cerebral stimulation, starting from the first day after surgery during 4 consecutive days, with each session having 20 minutes. Will be applied a direct current stimulus of 2mA in the right anode and in the left cathode on the prefrontal right region.
SHAM GROUP: The same equipment used in tDCS as simulated stimulus similar to the active one. Will also be summited to neuropsychological tests to evaluate memory, attention, and executive functions as well as data relative of surgery, cognitive evolution and quality of life in the postoperative period. The neuropsychological test will be describes according groups and the moments of application, with mean and standard deviation (SD) and compared to results of normative tables with Z-score (±1,96). The data will be expressed in means, medians, confidence intervals (CI-95%) and SD and analyzed by Generalized Estimating Equation (GEE), to comparison of the results between the two groups. P<0,05 will be considered significant.
Keywords:Postoperative Cognitive Dysfunction, transcranial Direct Current Stimulation, Cardiac Surgery
POCD, Postoperative Cognitive Dysfunction; tDCS, transcranial Direct Current Stimulation; FAPESP, Support Foundation Researched state of São Paulo; InCor, Heart Institution; HC-FMUSP, Hospital das Clínicas and the Medicine School of University of São Paulo; SD, Standard Deviation; GEE, Generalized Estimating Equation; VLT, Verbal Learning Test; TMT, Trail Making Test
The postoperative cognitive dysfunction (POCD) is defined as a degradation of the intellectual function, causing injuries to memory, concentration capacity and daily activities. It’s considered a contrary event observed in elderly patients submitted to a cardiac surgery,1 being rare among youngster patients and others who submit to noncardiac surgeries.2 Even though some researches show that local anesthesia can cause cognitive dysfunction, it is known that general anesthesia and its depth can lead to a higher percentage of POCD.3
The majority of POCD cases are reported by the patients or by their relatives, and they refer to mnemonics, attentional and behavioral alterations, making the diagnosis imprecise. The POCD diagnosis requires neuropsychological evaluation, pre and postoperative. This evaluation must include information about the medicines taken before the surgery and some neuropsychological tests specifics to emotional and cognitive functions.4
Factors related to POCD or use of opioids after the surgery, lack of physical activities, postoperative fatigue, postoperative pain, depression and quality of life. Some medicines can worse POCD, as the pre and postoperative use of benzodiazepines, sedatives, ant depressives and antiparkinsons.5
The occurrence of POCD is elevated by 40% in patients over 65 years old, submitted to medium and large surgeries, and in cardiac surgeries this percentage can be over 80%.6 The risk factors aren’t completely defined yet, just as the importance of each of these factors in the development of this neurological complication that many times predisposes comorbidities increasing the mortality of the surgical patient.7 Psychiatric or neurological disorders, just as some surgical and anesthetic event, also can cognitively compromise some patients in the postoperative period.8
The under diagnoses of this surgical complication occur mainly because of the lack of cognitive functions routine exams on the preoperative period, to the lack of specificity of simple evaluation tests or the difficulty in applying more precise tests.9 The use of patronized and validated tests for the neuropsychological functions makes easy the preoperative cognitive examination and the postoperative comparison.10
Currently, therapeutic and psychoeducational means and even medicines are occasionally used to treat diseases that compromise cognitive functions that lead to injuries in the executive, attentional, motivational and emotional operations, as Attention Deficit Hyperactivity Disorder (ADHD).11 Among these therapeutic, but yet little defused, however, promisors we found the Transcranial Direct Current Stimulation (tDCS), a technique capable of stimulating the human brain with a few advantages, being painless and noninvasive.12
This technique consists in a simpler and less costly neuromodulation technique, being able to induct changes on the excitability of the motor cortex for up to one hour after the stimulation.13 Such changes depend on the polarity of the applied electric current and on the stimulus duration. The polarity of the anodic current is responsible for increasing the cortical excitability, while the cathodic polarity is responsible for contrary effects, suppressing the cortical excitability.14 Processes of lasting cerebral elasticity depend on the changes that occur directly in the synaptic forces and results in anatomical changes; tDCS’s role is to alter these synaptic forces.15
The effect of the tDCS has been observed on neuropsychiatric disorders, and is showing improvements in motor, behavioral and emotional areas.16,17 Neuroplasticity is a physiological property of the Central Nervous System (CNS) that allows to the brain to adapt to different stimulus and it’s intrinsically linked to learning processes.18 This plasticity capacitates the individual who has some neurological or psychiatric commitment to neurologically rearrange some functional capacities, showing previously lost abilities like, for example, the cognitive and motor rehabilitation on people who suffered a Cerebrovascular Accident (CVA) or Stroke.19,20
Knowing about the neuroplasticity, the benefits of the tDCS and the possible cognitive commitment after cardiac surgeries, this study hypothesizes that the stimulations of the tDCS might decrease the occurrence of POCD in patients submitted to cardiac surgeries. The First Outcome will be assessed if tDCS sessions can decrease the occurrence of POCD in patients submitted to cardiac surgery and the second outcome will be if the tDCS technique can rehabilitate the patients with POCD after submitted to cardiac surgery.
The study was approved by the Scientific Commission of InCor and by the Ethics Commission for Projects Analysis of Hospital das Clínicas and the Medicine School of University of São Paulo, Brazil. Was registered on Clinicaltrials.org, and the research data will be stored in the RedCap-HC-FMUSP system and will be asked to help to Support Foundation Researched state of São Paulo (FAPESP) for the research. The collection of data will be held in the Heart Institution (InCor) in the Hospital das Clínicas of the Medicine School of University of São Paulo (HC-FMUSP) and all patients will receive a detailed written and oral explanation about the study and the research, which will be invited to participate.
Patient selection criteria
Patients will be evaluated by Mini Mental State Examination (MMSE) and those who doesn’t reach the minimum demanded score (>18 points and >23 points) by this tracking test, according to the subject’s education degree, score will be eliminated.
The MMSE evaluates reasoning, space-time orientation, memory and scholarship. The cutoff for this instrument is considered for two types of education- up to 4 years of regular academic study and up to 4 years of education. With an 18 points cutoff for the less schooled, those who only concluded up to the 5th grade, which correspond to Brazilian formal education as Fundamental Education I, and with a 23 points cutoff for those with higher education degree, starting from the 6th grade, as correspondent to the Brazilian system as Fundamental Education II.21
Inclusion criteria
Exclusion Criteria
Free and clarified consent term
After elective surgical indication and evaluation of the inclusion and exclusion criteria, patients will be invited to participate in research. Clarifications about the general study objectives will be offered to patients that will sign the Consent Form in two-way.
Will be include 138 adult patients submitted to cardiac surgery randomly allocated in two groups:
Will also be applied neuropsychological tests to evaluate memory, attention, and executive functions as well as another tests to assess specifics contents useful to describe the sample and research’ results. The tests applied will be on specific data set (Figure 1).
Sociodemographic Datawill be analyzed including education, marital status, occupation, and current medication. Signs and symptoms of depression will be assess preoperatively using the Beck Depression Inventory (BDI), for screening on global cognitive will be use Telephone Interview for Cognitive Status (TICS), will be use the Verbal Learning Test (VLT) for long-term memory and the Recognition Memory Test (TEM-R) for visual memory, the Symbol Digit Modified Test (SDMT) will be use to assess short-term memory, visual search skill and attention, STROOP Test will be assess the selective attention, inhibitory ability and mental flexibility that are constructs of executive function and the Trail Making Test (TMT) for the assessment of selective and alternating attention.
Beck Depression Inventory (BDI), which consists of 21 questions that explore depressive symptoms on a scale of 0 to 4, where zero represents no symptoms and four is the maximum symptomatology. A total of 14 points will be consider indicative of the presence of moderate depressive symptoms.22
Patient Questionnaire health (PHQ-9), this questionnaire about the health of the patient is an instrument with 9 questions. Each question has 4 possible responses: 0 (no day), 1 (several days), 2 (more than half days), and 3 (nearly every day). The PHQ-9 can be interpreted in three ways: 10 in the form of algorithm, identifying individuals with a major depressive episode and tracking probable cases of major depressive disorder; 20 as a continuous measure, with scores between 0 and 27 points, being able to assess levels of depressive symptoms through the cut- points 5, 10, 15 and 20 points=mild depression, moderate, severe and serious; 30 as continuous measurements with scores between 0 and 27 points, classifying the individuals dichotomous through the use of a single cutting point (typically ≥10).23
The Confusion Assessment Method (CAM-ICU) is a test to evaluate delirium; patients are evaluating qualitatively by the researcher from a number of simple questions to the presence or absence of postoperative delirium. This review will be done on the patient to wake up from anesthesia in the first hours after surgery and on the third day postoperative.24
The Telephone Interview for Cognitive Status (TICS) will be use as a standardized test to assess neuropsychological functioning when assessing cognitive skills. This test can be used when screening personally is impractical or when patients are unable to attend the clinic. This test consists of a structured interview with 11 items that assess the skills of spatial and temporal orientation, mental control, memory, general information, language and calculations.25
Memory will be assessed using the Verbal Learning Test (VLT) this test consists of a list of words. A list of 15 words is presented and must be stored and recalled in three successive attempts (VLT/ A-B-C), with delayed recall after 25 minutes (VLT-Delay). Rate is the number of words recalled and the number of errors for each presentation. The VLT evaluates the modalities of memory immediate, consolidated and long-term. This instrument will be held in two stages: pre-operative at the time of 1st evaluation before surgery and postoperatively in the second and final assessment between day 10 and 15 postoperatively.26
The Recognition Memory Test (TEM-R) consists of storing pictures and words to further identify remembered stimuli. For the stimulus responses can be presented to the subject in graphic form (figures) or written (words). This instrument will be held in two stages: pre-operative at the time of 1st evaluation before surgery and postoperatively in the second and final assessment between day 10 and 15 postoperatively.
The Symbol Digit Modified Test (SDMT) will be applied for the evaluation of short-term memory, visual search skill and attention. This is a graphical task where the individual has to fill in symbols exemplified in the spaces below the corresponding number within 180 seconds. The result is measured as the number of symbols drawn and the number of errors.27
Attention will be assessed by STROOP Test, which consists in presenting three paper sheets to the subject. The first one, the patient should verbalize the names of colors printed in black ink. In the second, verbalization is made of color are filled rectangles, the same provision of the words of the previous slide. The third blade consists in verbalize colors printed over the written word. Evaluates selective attention, inhibitory ability and mental flexibility that are constructs of executive function. Scores obtained include the number of words (Word task), number of bar colors (Color), and number of color words (Color–Word) completed within a set time, or as noted above, the amount of time required to complete each of the tasks. We will consider the number of errors as well.28
Attention will also be evaluated using the Trail Making Test (TMT) for the assessment of selective and alternating attention. In part A of the test, the subject must draw lines connecting consecutively numbered circles. In part B, the subject must draw lines connecting circles alternately with letters and numbers in a sequence. The result is measured as time and trial errors. The Attention function will be examined with Trail Making Test (TMT). This test consists of two parts. In Part A, the subject must draw lines connecting consecutively numbered circles. In Part B, the subject must draw lines alternately connecting circles with letters and numbers in a sequence. The test involves the addition of alternate and selective attention, visual screening and complex manual dexterity (Part A) and executive processes (Part B). Among the executive procedures, the inhibitory ability and cognitive alternating seem to be those most required in completing the task. They are valued the time spent and the number of errors in each of. These instruments will be held in two stages: pre-operative at the time of 1st evaluation before surgery and postoperatively in the second and final assessment between day 10 and 15 postoperatively.29
Data collection
The database will be inserted on the Redcap platform. The intraoperative data will be obtained at the end of the surgery. Will be collected data about the type of surgical procedure, the CPB (Cardiopulmonary Bypass) duration, if used, number of transfused blood products and water balance. Postoperative data will be obtained during the admission in the surgical ICU or in the infirmary. Trained nurses will collect clinical data as the time of mechanical ventilation, presence of infection daily. Will be daily collected routine postoperative laboratory exams until the hospital discharge. Patients will be followed during the whole admission period in the ICU and in the infirmary in order to obtain data about the possible occurrence of delirium, postoperative complications, evident cognitive dysfunctions and mortality. After the discharge/transference from the ICU will be followed to the 30th postoperative day for the identification of morbidity or mortality in this period. The first outcome will be consider over TICS’ results used to evaluate the evolution of global cognition postoperatively and will be apply in every phase’s pre and postoperatively. For the diagnosis of POCD, a composite cognitive index will be establish defined by the occurrence of cognitive impairment in TICS and at least 1 of 8 possible deficits of the others neuropsychologist tests. Changes in neuropsychological tests will be compared with the results of tables of normative subjects matched for age, gender and formal education.
Interim analysis
Preliminary statistics analysis of the clinical results will not be planned and won’t be defined objective criteria for a standstill of the study. However, is established that in cases of complications or unexpected improvements during the execution of the study, researchers will make an isolated evaluation about the time e frequency of the occurred events and will analyze the necessity or the possibility of an interruption or completion of the study.
Randomizing will be held by using the Internet website randomizer.org. It will be held in groups of 30 patients, with an internal analysis forecast after each group randomization is over. The randomized groups will be kept in opaque envelopes and will be opened in the beginning of the patient study. There will be “blinding” for the patients and the researchers that will analyze the outcome.
The volunteers will be evaluated in a model with the intention to treat (ITT) of recovering the cognitive functions evaluated by scores on the test based on normative tables, this is the primary outcome. The secondary outcome will be improvements on the response of these cognitive tests, the admission of these patients will last 30 days in the intensive treatment unity and in the hospital. There will also be evaluated data relative to the surgery, the cognitive evolution and the quality of life in the postoperative period.
Regulation and methodology for the analysis of the neuropsychological tests results
The application of neuropsychological evaluations must be as base for the definition of the diagnosis of POCD. The battery of tests used in this study, which gauges for superior cognitive memory, executive, attention and language functions, with the intention of detecting possible and subtle neuropsychological dysfunctions.
The patients will be evaluated by an expanded battery of neuropsychological tests (BNT) for the evaluation of the cognitive functions, besides measuring emotional aspects related to depression and quality of life. All neuropsychological tests will be individually administered verbally or graphically, timed and corrected and compared with results in scale according to age, gender and education patronized sample in general population, having as reference the neuropsychological scales. In relation to the time of execution of the task, is expected that the individual doesn’t exceed a time of three minutes.
Memory: Memory will be immediately evaluated after the evocation of the language and after twenty minutes.
Executive function: the evaluation of the executive function for the search for strategies, drape and organization of stored content, just as the language, will occur for the clinical observation of the patient’s speech, the eloquence, fluency, thought course and the performance during the fulfillment of the tests.
Attention: The tone and maintenance of attention will be evaluated during the BNT application and by standard instruments.
Criteria for POCD diagnosis
The POCD diagnosis will be defined based in two criteria: Two scores of standard deviation already defined by z-score of each test (normative table) and/or starting from previous result of tests performed by the patients before the surgery. The expected scores are found in normative tables on majoritypart of the tests used and defined by education and age.
Neuropsychological evaluation data
The neuropsychological tests will be performed on pre-operative at the time of 1st evaluation before surgery and postoperatively in the first and final assessment between day 8 and 10 postoperatively after stimulation with tDCS. The patient will be asked to attend for evaluation 30th, 90th, and 180thdays after from surgical event to be assessed again with a neuropsychological battery and clinical evaluation according to the program of the hospital the agenda of the InCor.
Anesthetic surgical evaluation
Will be evaluated data related to:
tDCS stimulus protocol
The tDCS protocol will involve the application of two sponge electrodes on the scalp. The positive electrode is placed on the dorsolateral prefrontal underlying cortex left area (F3 region in the international system 10/20 for electroencephalogram), and the negative electrode will be placed on the supraorbital overlying right area. An electric direct current of 1-2mA will be applied between the two electrodes for about 20 minutes, with the tDCS sessions being promoted daily during 4 days in the postoperative period (twice a day) comprising 8 postoperative sessions. For the tDCS sessions (stimulus or simulated) the patient will be comfortably kept in the ICU, or ward, bed, with his/her back inclined in 45º. Will be installed two sponge electrodes of 25-35 cm2 (nonmetallic) surfaces, moistened in NaCl solution, on the scalp, one serving as anode (positive pole) and the other as cathode (negative or reference pole). An electric direct current of 2mA (produced by a generator with constant current, fed by a regular battery) is applied between these two electrodes for 20 minutes. (Figure 2).
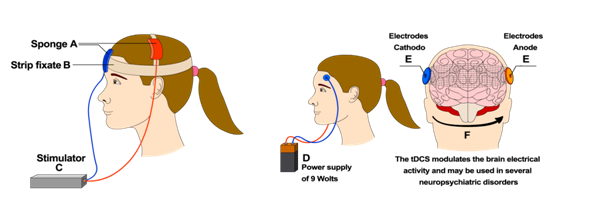
Figure 2 Use of Transcranial Direct Current Stimulation technique (tDCS). tDCS: Transcranial Direct Current Stimulation; PO: Postoperative.
Sample calculations and statistical analysis
Based on a POCD occurrence of 40% in elderly patients and having a decrease of 20% of POCD on the group that receive the tDCS, with a maximum error of 5%, with a confidence interval and a desired statistic power of 90%, estimate that 138 patients will be needed to compose the sample of this study. The results of the neuropsychological tests will be described according to the groups and moments of evaluation, by standard and pattern deviation, and compared between the groups using the Generalized Estimating Equation (GEE). (GraphPad Prism Version 6.0f).
The changes on results of the neuropsychological for the postoperative time tests will be compared to the results of the normative tables, according to sociodemographic data of age and education using as reference the cognitive dysfunction z-core (±1, 96). A Mixed-Model of Linear Multiple Regression will be calculated for the analysis of missing data during the study phases. Will be considered significant values inferior top<0, 05.
Risk and benefit evaluation
By the letter analysis, it’s evident the necessity of searching new therapeutic alternatives for the Postoperative Cognitive Dysfunction. The use of tDCS is authorized for the treatment of depression and psychiatric disorders as Schizophrenia and Obsessive-compulsive Disorder. But there are no studies about the use of this tool on patients with POCD. All patients will receive the usual treatment used in the institution for treating postoperative recovery with medicines. The tDCS technique is considered safe and without medicine could be better than another conventional treatments. Might occur a slight discomfort during the stimulation, if the discomfort is considered unbearable, the procedure will be interrupted and the patient will be kept in the study in the principle of intention to treat (ITT).
On the other words, the use of Transcranial direct current stimulation on prevention of postoperative cognitive dysfunction after cardiac surgery is a good subject to be researched, especially with the documented reports of tDCS to increase cognitive performance (even in healthy adults) on a variety of tasks and its ability to achieve persistent cortical changes even after the stimulation is ended. Other research could be also beneficial to realize a comparison with the effect of other neuromodulation techniques, for instance neurofeedback, rTMS in patients with postoperative cognitive dysfunction (POCD) not only in cardiac surgery but, in general surgery undergoing deep anesthesia or a specific population as in a sample of elderly patients or illiterate.
Since this is a study, which shall have its beginning in October of this year the result will be publicly available following the collection, analysis and interpretation of data recorded in this survey. However, we can conclude that this study will be able elucidated much concerning the tDCS technique and its application onto patients with POCD especially after cardiac surgery.
This study has the register in ClinicalTrials.gov Identifier: NCT02549560.
The authors followed the International Committee or Journal of Medical Journals Editors (ICMJE) form for disclosure of potential conflicts of interest. All listed authors concur with the submission of the manuscript; all authors have approved the final version. The authors have no financial or personal conflicts of interest.

©2015 Valentin, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.