Journal of
eISSN: 2373-6410


Case Report Volume 9 Issue 6
Department of Neurosurgery, Centro Hospitalar Universitário de Coimbra, Portugal
Correspondence: João Páscoa Pinheiro, MD, Centro Hospitalar Universitário de Coimbra, Neurosurgery department, R. Prof. Mota Pinto 3075, Coimbra, Portugal, Tel +351915484428,
Received: November 22, 2019 | Published: December 31, 2019
Citation: Pinheiro JP, Carneiro D, Santiago J, et al. Dural sinus thrombosis: The unusual complication of traumatic brain injury - a case report. J Neurol Stroke. 2019;9(6):342-344. DOI: 10.15406/jnsk.2019.09.00401
Background: Dural sinus thrombosis is a rare cerebrovascular disease characterized by a complete or partial obstruction of the blood flow inside a dural sinus, promoted by an intraluminal thrombus. Traumatic brain injury is an uncommon cause, with an ill-defined prevalence.
Case presentation: A 40-year-old woman, who had taken oral contraceptives for 20 years, was brought to the emergency department after a traumatic brain injury. She was discharged after an unremarkable neurological examination and normal evolution of intracranial lesions. Twenty- five days later, she returned to the hospital with signs of intracranial hypertension. A computed tomography cerebral venogram revealed a left dural sinus thrombosis. The patient started anticoagulation therapy immediately.
Conclusion: Physicians caring for survivors of traumatic brain injury should consider CT venogram to rule out dural sinus thrombosis in patients with prothrombotic conditions and skull fractures over a dural sinus.
Keywords: case report, dural sinus, oral contraceptives, thrombosis, traumatic brain injury
DST, dural sinus thrombosis; CT, computed tomography; CVT, cerebral venous thrombosis; TBI, traumatic brain injury; GCS, glasgow coma scale; ICP, intracranial pressure; SDH, subdural hematoma; TF, tissue factor
Dural sinus thrombosis (DST) is a rare subtype of cerebral venous thrombosis (CVT), accounting for only 1% of all ischemic cerebrovascular diseases. It is more frequent in children and young women and has an incidence of 3 cases per million. The first report was made in 1825, by the French physician Ribes, during the autopsy of a patient with a neoplastic disease of the central nervous system. Nowadays, with the development of new imaging techniques such as computed tomography (CT) venography, DST is more easily detected. Despite these technological advances, DST continues to be an underdiagnosed disease with considerable mortality and morbidity rates. Traumatic brain injury (TBI) is an unusual cause of DST with a virtually unknown incidence.1
A 40-year-old woman suffered a left parieto-temporal TBI after a fall. The event was preceded by a transient loss of consciousness followed by spontaneous recovery. She complained of nausea and a light tension-type holocranial headache. The pain was relieved with analgesic and antiemetic drugs. She had a Glasgow Coma Scale (GCS) of 15 and an unremarkable remaining physical and neurological examination. The electrocardiogram and echocardiogram were both unremarkable. The cranial CT scan showed a left linear fracture of the petrous temporal bone (Figure1A), a 3-millimetre left subdural hematoma (SDH) and pneumocephaly (Figure 1B). Her past medical history was relevant: she had taken the same brand of oral contraceptives for the previous 20 years.
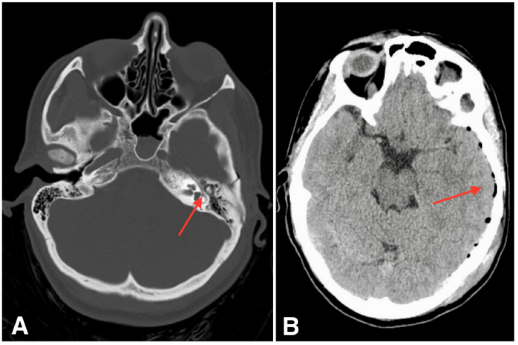
Figure 1A CT scan showing left linear fracture of the petrous temporal bone.
Figure 1B CT scan showing left temporal pneumocephaly and milimetric SDH.
The intracranial haemorrhagic lesions were monitored with two cranial CT scans while the patient was hospitalised. The second one, performed on the 4th day after the trauma, revealed partial reabsorption of the pneumocephaly and total resolution of the SDH (Figure 2). At the time of hospital discharge the patient was neurologically stable and capable of returning to her normal daily activities. She was advised to suspend oral contraceptive therapy.
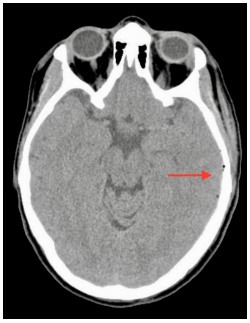
Figure 2CT Scan preformed 4 days after TBI showing partial reabsorption of pneumocephaly and complete resolution of the SDH.
The patient returned to the emergency department with complaints of a sudden strong left parieto-temporal headache, confusion and blurred vision 25 days after the traumatic event. A cranial CT scan showed complete resolution of the SDH and pneumocephaly (Figure 3). Even though the intracranial lesions had had a natural evolution, the patient was still symptomatic and now presented with an altered state of consciousness (GCS 13 - E3M6V4). Thus, a CT venogram was performed, which identified an absence of contrast enhancement on the left distal third of transverse (Figure 4A) and sigmoid (Figure 4B) sinus and on the left internal jugular vein, compatible with DST (Figure 4C & 4D). The patient immediately started anticoagulation therapy with enoxaparin 80 mg twice a day for 4 days and warfarin for 1 year. Recently, at the 14-month follow-up, a complete dissolution of the thrombus and dural sinus recanalization were identified in the CT venogram. Genetic or acquired thrombophilia, vasculitis, and neoplastic disease were excluded.
We presented the case of an otherwise healthy 40-year-old woman with a left temporal TBI, intracranial pneumocephaly and a delayed presentation of DST. DST is a rare cerebrovascular disease, with mortality rates ranging from 5-30%. This wide range is explained by its underdiagnosis and nonspecific signs or symptoms. The most common clinical manifestation is headache (80%), followed by partial seizures (40%), papilledema (30%), altered state of consciousness (20%) and diplopia (12%).2
DST diagnosis is achieved when clinical suspicion leads to the performance of a CT venogram, the most important diagnostic exam. TBI is a rare cause, so several other factors must be taken into account, since they increase the risk of DST: genetic and acquired thrombophilia, prothrombotic drugs such as oral contraceptives, central nervous system infections, neoplastic diseases, systemic vasculitis, neurosurgical interventions, lumbar puncture and pregnancy. The relationship between TBI and DST was first described by Bagley in 1934. The incidence of DST after penetrating trauma is 4%. However, its prevalence after closed head injury and linear skull fractures is not well established.3
The pathophysiology of post-traumatic DST is explained by components of the Virchow’s Triad: haemodynamic changes, endothelial lesion and hypercoagulability. According to Ohm’s Law applied to fluid dynamics, the blood flow inside a vessel is inversely proportional to the vessel’s resistance and directly proportional to the perfusion pressure. Therefore, extrinsic compression on the dural sinus (caused by extra-axial haemorrhages, depressed skull fractures or bone fragments from linear fractures) is responsible for haemodynamic changes inside the sinus, contributing to intra-luminal clot formation. On the other hand, an endothelial lesion promotes platelet activation and adhesion to the subendothelial collagen via Von Willebrand factor. Consequently, the expression of the transmembrane protein tissue factor (TF) increases. TF is responsible for factor VII activation, the main trigger for the extrinsic pathway of the coagulation cascade.4
An increase in intracranial pressure (ICP) and jugular venous pressure is strongly associated with DST. Blood flow obstruction inside the sinus impairs cerebrospinal fluid absorption and promotes rupture of the blood-brain barrier, which in turn leads to vasogenic oedema. Cerebral perfusion pressure (CPP) is inversely proportional to ICP. Thus, an increase in the latter reduces CPP and consequently the cerebral blood flow, which results in ischaemia and cytotoxic oedema. Occasionally, a decompressive craniectomy may be necessary to relieve the ICP promoted by brain swelling. Otherwise, the therapeutic approach for DST is similar to that for CVT, with low-molecular-weight heparin as a bridge to a vitamin K antagonist. Endovascular thrombolysis could also be used as a treatment strategy.5 In this case, the patient starts anticoagulation therapy 20 days after the traumatic event, so the risk of intracerebral re-haemorrhage is extremely low.
The prevalence of DST associated with linear skull fractures is not well established, so identification of patients who will benefit from a CT venogram is crucial. Authors suggest that a CT venogram should be performed within the first 24 hours if the fracture is over the path of a dural sinus, if there is an altered mental status relative to a previous observation and in patients with prothrombotic conditions, such as oral contraceptive therapy. In asymptomatic patients with risk factors for DST, a subsequent radiological control is suggested within the first and second week after trauma.
In this case, we observed a late development of DST in a neurologically stable patient with a linear fracture over the transverse-sigmoid transition, who was taking oral contraceptives. Although the patient had taken oral contraceptives for a long time, the most likely cause of DST was the fracture over the transverse-sigmoid transition. Oral contraceptive therapy is a risk factor for DST and could increase the predisposition for this condition. The length of oral contraceptive therapy is not related to an increased risk of developing DST. The authors therefore consider that the haemodynamic changes caused by the traumatic event are the most probable cause for the DST. In the authors' opinion, it is imperative to understand whether prothrombotic drugs, such as oral contraceptives or chemotherapeutic drugs, increase the risk of DST in patients with a linear fracture in the region of a dural sinus without neurological impairment. Case-control studies should be planned in order to evaluate the risk-benefit of drug suspension in this specific group of patients.
Despite its unknown prevalence, DST is a described complication of TBI. Even with a complete and correct physical examination, it is challenging for physicians to have a high index of suspicion for DST. The incidence of head trauma is rising, so DST should be included in the guidelines for TBI management. Being a life-threatening condition, the identification of patients with a high risk of developing DST and those who will benefit from having a CT venogram is essential. Prompt diagnosis and early anticoagulation therapy could avoid secondary brain injury and the need for a life-saving intervention.
None.
None.
Consent for publication
Informed consent was obtained from the patient for publication of this case report and any accompanying images.
Author contributions
These authors contributed equally to this work.
Funding
None.

©2019 Pinheiro, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.