Journal of
eISSN: 2373-6410


Case Report Volume 10 Issue 1
Department of Internal Medicine, Serviço de Saúde da Região Autónoma da Madeira, Portugal
Correspondence: Rafael Ferreira Nascimento, Department of Internal Medicine, Serviço de Saúde da Região Autónoma da Madeira, Portugal, Tel +351912153471
Received: January 28, 2020 | Published: February 26, 2020
Citation: Nascimento RF, Gouveia F, Freitas JM, et al. Case on venous sinus thrombosis: the unexpected should be expected! J Neurol Stroke. 2020;10(1):58-59. DOI: 10.15406/jnsk.2020.10.00411
Introduction: The authors present a venous sinus thrombosis that started in a woman 10 days after labour.
Case Report: A 34-year old woman, who had gone into labor 10 days before her admission, presented to the emergency department with paresthesia on the right side of the body and dysarthria which started that day. The neurological exam showed predominant right brachial paresis associated with a diminished sensitivity in the right arm and leg. The CT-Scan revealed a venous thrombosis that reached the straight, superior and transverse sinus, with a greater extension on the right side involving multiple tributary veins. The admission in the cerebral vascular diseases unit was followed by heparin perfusion. Ten days after the onset of the episode the patient was submitted to another CT-Scan that showed resolution of the thrombosis. Goldman campimetry was considered normal. The patient was discharged from the unit and started an etiologic search, which pointed to the pregnancy as the main reason for the event. The echocardiogram and cervical duplex ultrasound were normal. Currently, the patient does not show any sequels and maintains follow-up in the cerebrovascular disease consult.
Conclusion: The authors highlight the role of the physician in the diagnosis of a rare entity in a woman, 10 days after labour, without any relevant past medical history.
Cerebral venous thrombosis (CVT) is a rare cause of cerebral vascular disease, corresponding to 0,5% of all cases of cerebral vascular disease.1 The annual incidence is estimated in 5 cases by one million of population, showing a higher frequency in women.2 In CVT clinical presentation, imagiology and prognosis are variable,3 showing a mortality rate of 10% in recent studies.4
This article presents a CVT in an otherwise healthy woman ten days after labor. During pregnancy platelets, factors levels (VII, VIII, IX, X and XII) and fibrinogen are elevated, fibrinolytic activity is reduced, since this hypercoagulable state persists several weeks postpartum pregnant women are at a greater risk to develop CVT.5,6
The authors present a case of a young woman who developed a CVT shortly after labor alerting to the fact that rare and unlikely diseases may occur when the physician least expect.
The authors present a 34-year old woman who went to labor 10 days before her admission in the emergency department. She presented with headache, paresthesia on the right side of the body and dysarthria which started that day. The neurological exam showed right brachial predominant paresis IV/V associated to a diminish sensibility in the right arm, without impairment of the right leg, coordination or muscular tone. Beside an increased C-Reactive Protein of 74.48 mg/L blood work did not show any other significant result.
Patient was submitted to a head computed tomography (Head-CT) scan which revealed a venous thrombosis that reached the straight, superior and transverse venous sinuses, with a greater extension on the right side involving multiple tributary veins, without any other lesions (Figure 1).
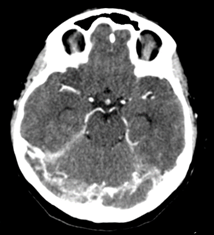
Figure 1 Head-CT showing a venous thrombosis of the straight, superior and transverse venous sinuses.
The admission in the cerebral vascular diseases unit was followed by administration of low molecular weight heparin. Ten days after the onset of the episode the patient was submitted to another Head-CT that showed resolution of the thrombosis (Figure 2). Goldman campimetry was considered normal. The patient was discharged from the unit and started an etiologic search. In a consult regimen the proceeded with the etiological investigation pointing out that the echocardiogram and eco-Doppler were normal. Further analysis excluded auto-immune causes as well as genetic causes namely mutation of Leiden V Factor gene and Prothrombin G20210A gene.
Till this day the patient does not show any sequel and maintains a regular follow-up in the cerebrovascular disease consult.
In this case we have a young woman who presented with neurological focal deficits, which is one of the four main presenting syndromes of CVT, the other three are isolated intracranial hypertension, seizures and decrease level of consciousness.7,8 These syndromes can occur isolated or in association depending on the extension and location of thrombosis.8 The patient also presented with headache which is the most common symptom in CVT affecting 90% of patients in acute phase and 64% in a subacute phase.8,9
The symptoms seen in CVT are due to the obstruction of the venous sinuses and impaired drainage of cerebrospinal fluid leading to intracranial hypertension,10 having this into account, Goldman campimetry helps to assess visual impairment caused by intracranial hypertension secondary to a thrombus. In this particular case Goldman campimetry was normal probably due to the fact that the thrombotic event was not big enough to cause an increase in the intracranial pressure and subsequently visual symptoms.
The first line treatment for CVT includes administration of anticoagulants such as heparin and warfarin11 to try limiting de progression of the thrombotic event, in this case the patient was treated specifically with low molecular weight heparin 60 mg without any complications. Some patients may not respond to the anticoagulation and develop refractory intracranial hypertension.2
Even though the blood work did not show any cause that could explain a predisposing factor to CVT, it should not be forgotten that pregnancy and postpartum are themselves risk factors because of the hypercoagulable state that exists associated to these two conditions, furthermore the postpartum period conventionally defined as the 6 weeks after delivery is associated with increases by a factor of 3 to 9 in the risk of stroke and by a factor of 9 to 22 in the risk of venous thromboembolism when compared to a nonpregnant state.12
Nowadays the patient maintains a regular follow-up in the cerebrovascular disease consult, though some studies show that recurrence of a new CVT episode is rare and happens in about 2.8% of cases.13
The authors highlight the role of the physician on the diagnostic of a rare entity in a woman, 10 days after labor, without any relevant background.
None.
The author declares no conflicts of interest.
None.

©2020 Nascimento, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.