Journal of
eISSN: 2373-6410


Case Report Volume 10 Issue 5
1Department of Internal Medicine, Serviço de Saúde da Região Autónoma da Madeira, Portugal
2Department of Infectious Diseases, Serviço de Saúde da Região Autónoma da Madeira, Portugal
Correspondence: Rafael Ferreira Nascimento, Department of Internal Medicine, Serviço de Saúde da Região Autónoma da Madeira, Portugal
Received: September 17, 2020 | Published: October 30, 2020
Citation: Nascimento RF, André DR, Gouveia F, et al. Beware of cryptococcomas when treating Cryptococcal meningitis. J Neurol Stroke. 2020;10(5):183-184. DOI: 10.15406/jnsk.2020.10.00435
Introduction: The authors describe a rare presentation of central nervous system cryptococcosis in an immunocompromised patient.
Case description: An HIV-positive patient, with poor adherence to the treatment, presented with a seventeen days history of severe headache. On the neurological exam there was only evidence of neck stiffness, he had a CD4 count of 23 cells/μl and plasma HIV RNA viral loads of 364,000 copies/ml. Lumbar puncture revealed positive for cryptococcal antigen virus and so treatment with amphotericin B was started. During his admission the patient developed an expressive aphasia with visual hallucinations and the brain MRI revealed cerebral cryptococcomas. After 98 days of treatment general and neurological examination was normal and the patient was discharged home.
Conclusion: This case highlights a rare and severe complication of Cryptococcus neoformans infection in immunocompromised patients.
Cryptococcomas are a rare complication of infection by Cryptococcus genus of invasive fungi. The two Cryptococcus species implicated in cryptococcoma are Cryptococcus gattii and Cryptococcus neoforman.1,2 Cryptococcomas should be suspected in a patient with cryptococcal meningitis who shows clinical deterioration despite adequate treatment. The presentation of cryptococcoma differs largely on which organ is affected, central nervous system commitment usually presents with raised intracranial pressure and hydrocephaly. This article describes a rare presentation of central nervous system criptococcomas in an immunocompromised patient.
A 40-year-old-male presented for a routine check of his HIV-1 that had been treated with combination antiretroviral therapy since 2008. He was a patient with poor adherence to the treatment and with poor disease control. His current medication was tenofovir and a combination of lopinavi/ritonavir and abacavir/lamivudine which the patient abandoned nine months before.
The patient complained of a 17-day history of severe headache associated with nausea and vomiting. The headache was localized to the frontal region and was described as dull and without relief despite paracetamol administration. General examination was normal but on the neurological examination there was evidence of neck stiffness with negative Brudzinski´s and Kernig´s signs. Blood tests revealed normocytic normochromic anemia with Hb 11.2 g/dL (13-18), sodium 129 mmol/L (136-145), chloride 92 mmol/L (98-107), c-reactive protein 10.6 mg/dL (<0.5), CD4 count of 23 cells/μl (700-1100) and plasma HIV RNA viral loads of 364,000 copies/ml (< 20). Contrast enhanced CT-scan of the brain was normal. A lumbar puncture was performed which showed a raised opening pressure, with a cerebral spinal fluid (CSF) cell count of 52 cells/mm3 (Mononuclear cells), the protein level was 191 mg/dl (15-45), and glucose was 20.6 mg/dL (40-70). CSF results revealed no bacteria, but few encapsulated yeasts identified as Cryptococcus neoformans and CSF real-time PCR returned positive for cryptococcal antigen virus and negative for JC virus, Toxoplasma gondii and syphilis. Culture for mycobacteria was negative. CSF culture was positive for Cryptococcus neoformans confirming cryptococcal meningitis and so the patient started intravenous amphotericin B (ampB) 0.7 mg/kg/day for two weeks with transition to oral fluconazole 800 mg/day. Serial lumbar puncture was performed throughout his hospital stay in order to control symptoms of increased intracranial pressure (ICP).
The headaches persisted and on the 31th day of hospital admission the patient developed an expressive aphasia with visual hallucinations with no signs of facial palsy, suspecting cerebral cryptococcoma a brain MRI scan was performed showing fronto-temporal pachymeningeal gadolinium enchancement in relation to pachymeningitis and intra-parenchyma small nodules in the midbrain and lenticular nucleus in favor of cryptococcomas (Figure 1).
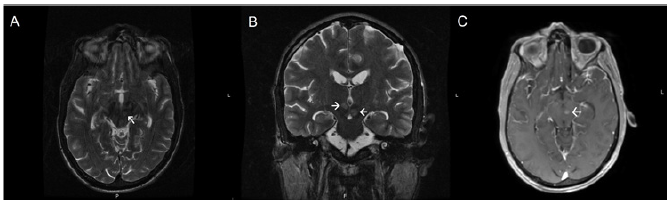
Figure 1 Brain MRI showing in the midbrain and lenticular nucleus cryptococcomas. T2-weighted axial (A) and coronal (B) magnetic resonance imaging showing increased signal hypertensity on T2. (C) Post contrast study showing enhancement of the lesions.
Induction therapy with ampB 4 mg/Kg/day was prolonged to 6 weeks maintaining fluclonazole (800 mg/day), after 98 days general and neurological examination was normal and the patient was discharged home. The patient did the treatment for a total of 18 months and during that time antiretroviral therapy was restarted without any major side effect.
Cryptococcus is the most common fungus causing central nervous system infection (CNS) with the most common presentation being meningoencephalitis and it occurs mainly in immunocompromised patients 3. The treatment of cryptococcal meningitis involved several lumbar punctures whenever symptoms of ICP were present, through reducing the opening pressure to ≤20 cm of cerebral spinal fluid ICP symptoms were effectively controlled.
In rare cases Cryptococcus neoformans can manifest has a granulatomatous CNS lesion that may cause a mass effect lesion known has cryptococcoma. We suspected our patient had cryptococcoma when he didn´t improve after 31 days of therapy and developed an expressive aphasia with visual hallucinations. When the diagnosis of cryptococcoma was confirmed, induction therapy was restarted with ampB 4 mg/kg/day plus fluclonazole 800 mg/day for at least six weeks in accordance with the Infectious Diseases Society of America.4 Unfortunately, in this particular case we had no access to flucytosine and so the induction therapy was done only with ampB, regardless the clinical evolution was favorable.
Intraparenchymal cryptococcomas usually present with low signal intensity on T1-weighted MRI and high intensity on T2-weighted images,5 surgery is reserved for large accessible lesions with mass effect. Cryptococcoma is a rare presentation of Cryptococcal infections that despite proper surgical and clinical treatment has a high mortality rate.5
Despite being rare, physicians should be aware of the possibility of cryptococcomas in a patient with cryptococcus meningitis who doesn´t improve despite adequate treatment.
None.
The authors declare no conflicts of interest.

©2020 Nascimento, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.