Journal of
eISSN: 2373-6410


Case Report Volume 3 Issue 3
1GHS Stroke Center, Greenville Memorial Hospital, USA
2Department of Emergency Medicine, Greenville Memorial Hospital, USA
3Pediatric Neurology, GHS University Medical Grp PED NEU, USA
Correspondence: Rodney Leacock, GHS Stroke Center, 71 Grove Road, Greenville, South Carolina, USA 2965, Tel 864-455-8848
Received: August 18, 2015 | Published: November 16, 2015
Citation: Leacock R, Sternberg S, Polley K, et al. A teenager with an acute stroke while at school. J Neurol Stroke. 2015;3(3):1-6. DOI: 10.15406/jnsk.2015.03.00093
Acute stroke in children is an uncommon occurrence. We present a 16 year old adolescent boy who developed acute left hemiparesis while at school and 911/EMS was called and received iv tpa and made an excellent recovery. We discuss potential challenges to stroke recognition and treatment in children.
Keywords:Acute stroke, Teenager, Children, Thrombolysis
EMS: Emergency Medical Services; iv tpa: intravenous tissue plasminogen activator; tpa: tissue plasminogen activator; GMH: Greenville Memorial Hospital; NIHSS: National Institute of Health Stroke Scale; CT: Computerized Tomography; CTA: Computerized Tomography Angiogram; CTP: Computerized Tomography Perfusion; MRI: Magnetic Resonance Imaging; PSC: Primary Stroke Center
Acute stroke in children is an uncommon occurrence. The reported frequency is 2.3 to 13 per 100,000.1 Children recognized and treated with iv tpa for acute ischemic stroke is a rare occurrence. We discuss the case of a 16 year old boy who developed acute left hemiparesis and received intravenous administration of tpa.
Recombinant tissue plasminogen activator was proven to be effective for acute ischemic stroke treatment in 1995.2 and approved by the FDA for use in eligible patients more than 18 years old since 1996. The Brain Attack Coalition described the formation of primary stroke centers in 2000.3 which was followed by the proposal for the formation of comprehensive stroke centers in 2005.4 and the proposal for the formation of acute stroke ready hospitals in 2013.5 There are even several guidelines which address acute ischemic stroke therapy, of which the most current is from 2013.6 With regard to stroke in infants and children the only guideline is from 2008.7 The formation of the primary pediatric stroke center has only recently described.8
A 16 year old adolescent male developed acute left hemiparesis while in the school training facility during a workout. The training staff suspected that he was having a stroke and 911/EMS was called. This led to a stroke alert at Greenville Memorial Hospital (GMH). Upon arrival to the Pediatric Emergency Department (Peds ED) he was greeted by the Pediatric Emergency Medical Team. Emergency stabilization was performed. An NIHSS scale was performed by Adult Stroke Team responders.
The patient was able to recall the duration of symptoms beginning about 2 hours prior, complained of a headache and was drowsy in the Peds ED bay. The initial NIHSS was 15. Direction was provided by the Adult Stroke Team responders to obtain emergent CT head and CT angiography. Additional responders included Pediatric Neurology who basically deferred to the Stroke Team for guidance and direction in the first 24 – 48 hours.
In the CT scanner, the patient experienced nausea and vomiting was given Zofran and maintained his airway. The non-contrast head CT did not show hemorrhage and the NIHSS remained 15. We proceeded with the CTP and CTA head and neck. Cerebral ischemia was suggested by the CTP, but there were limitations with both the CTP and CTA. Initial height and weight were 190 cm and 141 kg with blood pressure 145/55 and heart rate 66.
It was concluded that the patient was having an acute ischemic stroke and thrombolysis was considered. The patient’s father was contacted and explained the diagnosis and treatment options. The benefits and risks were explained to the father questions were answered and the father verbally consented to iv rt-PA administration. The CTA head did not show a large vessel occlusion and the CTA neck was of poor quality.
Our patient had hypertension, dyslipidemia, and migraine headaches. His mother had congenital heart surgery as child. There was a paternal grandmother history of stroke.
The tpa was started at 4:22 pm which was about two hours and fifty two minutes from the onset of symptoms and was stopped at 5:20 pm. During thrombolysis administration, the patient was monitored in Adult Trauma Bay. He experienced a severe headache and the repeat emergent CT head was negative for hemorrhagic transformation. The patient was admitted to the NeuroTrauma Intensive Care Unit (NTICU) for continued post thrombolysis monitoring. By 8 am the following morning, on examination, he had mild drowsiness, mild visual impairment, mild dysarthria, left facial paresis, mild left hemiparesis with only a slight drift of the upper and lower extremities, and the NIHSS was 7. The MRI brain (Figure 1) showed a right basal ganglia infarction. Thrombolysis with tpa limited the extent of infarction as it was suspected to involve a significant portion of the right middle cerebral artery pre-treatment. Two hours after the tpa was completed, he actually improved to an NIHSS of 2 but fluctuated through the night and the following morning his NIHSS was a 7. A repeat non-contrast CT head (Figure 2) was obtained at 9:18 am without hemorrhagic or significant infarction changes.
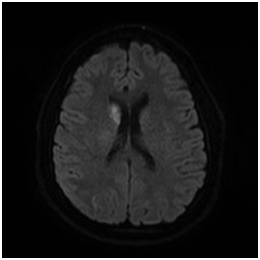
Figure 1 MRI-DWI showing acute right head of the caudate infarction at 9:32 pm about 5 hours post tpa initiation.
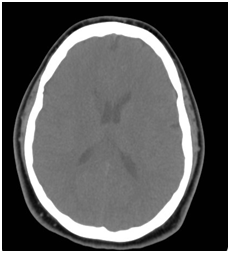
Figure 2 Non contrast CT head obtained at 9:18 am the following morning about 17 hours post tpa initiation.
After the NTICU course he was transferred to the Pediatric Service and followed by Pediatric Neurology. The patient regained ambulatory function. A carotid duplex was performed and less than 50% stenosis was found bilaterally. The 2D echocardiogram was interpreted as normal and without atrial septal defect. Seven days later, he was discharge to rehabilitation and his NIHSS score was 2 and the mRS=1. At a follow up office visit 3 weeks later his NIHSS was 0. No hypercoagulable disorder was found. An elevated lipoprotein A level was found and he was maintained on niacin, aspirin and topiramate.
This is our first administration of iv tpa for acute ischemic stroke in the pediatric population at GMH. GMH has been certified as a PSC by the Joint Commission since 2009. Our center averages about 700 adult ischemic stroke patients per year. Through ongoing participation in Get With The Guidelines-Stroke (9) [], our thrombolysis administration rate with tpa for acute ischemic stroke in adults is 28 percent and greater than 85 percent receive it in less than 60 minutes. Our pediatric stroke data is limited.
We have learned to be able to recognize acute stroke in the pediatric population can be very challenging indeed. Our patient was a 16 y.o.male who resembled an adult in many ways by height and weight. He was a football player and was under the supervision of experienced coaching and training staff who responded emergently. The EMS personnel brought the patient to GMH PedsED. There was discussion amongst all providers at GMH. In summary, the patient received the appropriate treatment and care.
Barriers to stroke recognition were his age, duration of symptoms, and uncertainty with diagnosis. Treatment delays were relying on available technology, patient stabilization, obtaining consent for treatment. Staff concerns and anxiety were raised about giving tpa to a teenage child. Intravenous thrombolytic use has not been established in pediatric patients.10 Where to monitor the child during and after tpa administration were concerns. Fortunately reassurance was provided to all of the staff who raised questions about the process and the plan.
Reported thrombolysis rates in children are very small from 0.7-2%.1,11,12 The challenges associated with site recruitment and patient screenings were described. Only 1 patient was enrolled out of 93 screened and 46% did have an ischemic stroke.1 Exclusion criteria reported included moyamoya arteriopathy, anticoagulation, malignancy, recent strokes, delayed recognition and treatment times, and stroke severity NIHSS < 6.1
In 2009, Amlie-Lefond et al.12 reported 15 out of 687 children enrolled in the International Pediatric Stroke Study (IPSS) received tpa 9 intravenously and 6 intra-arterially. Asymptomatic intracranial hemorrhages were reported in four patients. Two patients died and 12 of 13 had remaining neurological deficits. This is the largest reported experience with tpa administration and children.
More recently, Ladner et al.13 reviewed 124 stroke alerts over a 42 month period from April 2011 after the formation the pediatric acute stroke team and protocols. There were 30 strokes and 21 were ischemic of which two received mechanical endovascular therapy and one received endovascular fibrinolysis. The overall benefits were up to 40% of children had a stroke or a neurological emergency. Access to MRI was readily available the majority of times.
Amlie-Lefond et al.12 reported barriers to treatment with tpa included longer delays in making a specific diagnosis of stroke as stroke mimics are more common in children. The reason our patient received expedited care because he was in a setting around trained personnel who suspected he was having a stroke and called 911/EMS.We made every effort to adhere to current published adult guidelines for tpa administration.6 with regards to time and dosage unlike in Amlie-Lefond et al.12 where 7 of 15 did not receive treatment according to the published guidelines.14 Fonarow et al.15 showed with shorter door to needle times of tpa administration in less than 60 minutes that better outcomes were achieved from a national database of 1030 Get With The Guidelines-Stroke Hospitals. It has also been shown that less than 30 percent of patients are treated within 60 minutes. Pre-notification by 911/EMSfacilitated patient preparation for the ED and Stroke Team responders. The patient outcome was directly attributable to this. EMS, hospital prenotification is associated with shorter evaluation and treatment times .15 and a greater rate of tpa administration.16
Ways to improve the recognition of stroke in children is through the identification of predisposing risk factors like hypertension, diabetes, dyslipidemias, and obesity. Syndromes with a genetic predisposition for stroke include sickle cell disease, metabolic disorders like MELAS, hypercoagulable disorders, moyamoya disease or connective tissue disorders. Equally important is to raise community awareness through family education, teacher education, school education, and recreational and sporting event education. The most likely location for a child to have stroke other than home is at school. Although mechanisms like dissection were not identified, it is possible with football, weight training, wrestling, cheerleading or soccer.
To summarize, children can have a stroke and it is important to raise awareness about stroke recognition, treatment options, rehabilitation, secondary prevention, patient selection and eligibility, collaboration amongst participating specialties like EMS, emergency medicine, adult and pediatric neurology, radiology, and adapting stroke systems of care to include children and even potentially becoming a primary pediatric stroke center based on the criteria established by the TIPS study.1,8 The initial steps should include the formation of a pediatric acute stroke response team and protocols, and preferable access to MRI for emergency brain imaging .1,8,13
Despite the above mentioned barriers it is possible to achieve a good outcome using iv tpa for acute stroke in children. Individual case reports remain a significant source for outcomes in pediatric stroke care. A 15 year old boy with left hemiparesis, NIHSS was 7, was given tpa 1 hour and 43 minutes from symptom onset, and his symptoms resolved after 33 minutes.17 Another 16 year old boy presented to the ED 1 hour after onset of symptoms, with speech impairment and right hemiparesis, NIHSS was 13, and was given iv tpa 2 hours and 40 minutes after symptom onset. 8 hours later, he had near complete resolution of symptoms with normal speech and near normal strength.18 Tpa was administered 4 hours from symptom onset to a 16 year old girl who presented with basilar artery occlusion from a lupus anticoagulant and the NIHSS was 8. At 6 hours from symptom onset her NIHSS improved 2.19 To consider a child with a stroke for thrombolysis with tpa requires a more thorough assessment of history and examination, identify stroke mimics, access to advanced imaging including MRI, CTP and CTA, collaboration amongst a team of experts in stroke care, and well defined stroke protocols.7,8,12,13,17-19
Access to endovascular therapies for acute ischemic stroke offer a more precise and directed therapeutic option which are more readily available at larger institutions.13
None.
None.

©2015 Leacock, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.