Journal of
eISSN: 2373-6410


It is not unusual to face problems like malignant stroke and devastating post operative hemorrhagic infarction (POHI) in clinical practice. These conditions are akin to be perplexing nightmares for neurosurgeon especially when it comes to convince attendants for either surgical intervention or continuing the medical management. Early intervention has a key role in changing outcome in terms of survival but at the cost of a severely disabled or ventilator dependent (difficult to wean off) patient. In this review, we intend to highlight fallacies in management of malignant stroke and POHI focusing on a disregarded indication – “surgeon’s instinct and caregiver’s cultural belief”.
Cerebrovascular accidents are leading cause of mortality and disability throughout the world. Malignant cerebral edema with hemorrhagic stroke constitutes a significant proportion of these patients. Ever since Cushing performed first decompressive craniotomy (DC), the confusion on appropriate management of malignant cerebral edema continues. The present era of evidence based management and quality of life care has manipulated the literature with heterogeneous results and conundrums. Presently, the famous trials talk about functional improvement after DC and advantages of tracking secondary brain injury pathogenesis highlighting the insufferable outcome of various trials. Being a neurosurgeon, I believe that each one of us must have face a situation wherein, either caregiver’s forceful cultural belief or sometimes our own inner conscience push us against all available evidences; and a surprisingly better than expected results are achieved. We never report these cases but the question persistently troubles us is “whether to operate or not?” in a case of malignant cerebral edema.
Malignant cerebral stroke or devastating POHI usually manifests with a severe hemispheric syndrome including hemiparesis, gaze deviation and higher cortical signs followed by headache, papilloedema and decreasing consciousness. The life-threatening edema usually develops between 24 hours to several days propagating to midline shift and death.1 The hemorrhagic infarct in middle cerebral artery distribution complicates the clinical presentation with ocular motor apraxia,2 contralateral dens hemiplegia masquerading as subtle cerebral herniation syndromes. The alarming “line of danger” is very difficult to draw in these patients so point of intervention is rather depending on surgeon’s experience and rather serial radiological investigations. The incidence of surgical demanding POHI is less than 2%3 with overall poor outcome. Early surgical intervention is demanded but at risk of disability. So, question arises, is there any objective parameter below which one can manage these patients with medical options.
At present, role of intracranial pressure monitoring is controversial and radiological parameters have high variability.4 The expanding armamentarium on molecular research, may guide us with objective predictors on monitoring cerebral autoregulation failure and secondary brain injury, in near future. Bert Bosche et al studied the level of extracellular substrate concentrations by microdialysis, intracranial pressure (ICP), and tissue oxygen partial pressure (PtO2) along with neuromonitoring of neuroactive substances like transmitter amino acids (TAAs), lactate, pyruvate, and purines in peri-infarct tissue for early determination of patients at risk for malignant infarction.5 Likewise, Heiss WD et al highlighted the importance of positron emission tomography in early differentiation of malignant edema from benign counterpart.6
The heterogeneity in defining “malignant” progression demands low threshold for surgeon but evidences from metanalysis and randomized trials precludes surgeon in view of poor surgical outcome.1,7 Among the conservative medical options available, only hypothermia shows some beneficial effects in reducing postischemic secondary brain injury and blood brain barrier disruption in animal models.8 Other measures like osmotic therapy with hypertonic saline solutions, mannitol and glycerol did not significantly improve outcome.9 These measures are effective for transient lowering of intracranial pressure. The decompressive craniotomy is always last choice for stroke managing team. There is added risk of infection, reoperation, hydrocephalus, external brain tamponade, sinking skin flap syndrome, paradoxical brain herniation and seizures.10,11
Two problems that often come across are malignant strokes (usually middle cerebral artery stroke) in young patients and need for surgical interventions in POHI. We operated a twelve-year child with systemic lupus nephritis and intracranial hemorrhagic infarct. The child had acute renal failure, pericardial effusion and septic shock with very poor general condition. There was midline shift and frontal-parietal region edema. We operated him in view of younger age and our inner instinct. The parents were willing for perioperative risks. Post operative course was surprisingly better than what one could believe. The patient was discharged in full sensorium and underwent reconstruction cranioplasty in follow up. There is no level I evidence guidelines on management of malignant edema in age less than 18 years. Thereafter, severe comorbidity and poor general status precludes surgical intervention as per conclusions of trials. But the surgical decision based on inner conscience and experience based instinct resulted in unexpected good outcome contrary to what is quoted in famous trials.
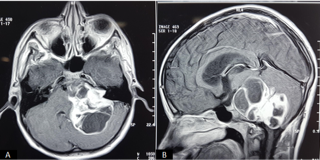
Similarly, another case of left cerebello-pontine angle giant schwanomma was operated. The patient landed in disseminated intravascular coagulation and surgical site POHI (Figure 1). Patient was managed on continuous mechanical ventilation. There was severe electrolyte disturbances and poor neurological brainstem response; so conservative management continued. Thereafter patient developed surgical site wound bulge and we had to decide for second surgery. We had lost all hopes but the caregivers inevitable belief persuaded us to re-operate (CSF diversion) resulting in acceptable outcome (which would not have been achieved if patient was left un-operated). Patient is improved and is command following status in follow up. Judith M et al quoted 1.1% to 4.4% rates of surgery related hematoma.12 He also found that these devastating hematomas occurred within 6 hours. Similarly, Benjamin et al, in his study found 2.1% incidence of hematoma needing surgical evacuation. He also concluded that POHI causes about one third of the post operative morality.13 These type of complications are rarely reported in literature. Third case was operated for giant hemangiopericytoma and developed hemorrhagic infarct in peri-operative region. The patient was re-operated in-spite of poor neurological post operative response and electrolyte imbalance. We discussed the option of medical management but somehow attendants and our team desired “going in”. Patient had good outcome, discharged and still under our follow up.
Several important trials like DESTINY, HAMLET, DECIMAL, etc focused on “time of intervention” and “post surgical (DC) outcomes”. Although initial trials favored early surgical intervention but later on a nebulous picture flooded the literature. The variability in inclusion criteria (age, timing of intervention, follow up time) and statistics used in these trials hinders comprehensive clinical trust. A school of thought objects classifying “favorable outcome” as modified Rankin score of 4 (moderately severe disability).14 The functional outcome of DC is questionable with this dichotomous grouping; 63% of surviving patients in DESTINY II trial refuted their own decision.15 A surgical decision is further shaken with fact that a subset of patients show improvement despite malignant edema or poor general condition or even radiological evidence of midline shift.16,17 Therefore, these trials neither defined “timing of intervention” nor satisfied the “functional outcome” leaving final decision on surgeon’s deliberation.8 Paul Alexander and colleagues, in their meta-analysis of several trials studied effect of DC in extended time range of 96 hours.11 They found increased number of disabled dependent patients but still DC improves on overall mortality specially in subsets of population at younger age group.
Herein comes the “experience based instinct”. Nietzsche and Tanner’s views on the Apollonian and Dionysian theory of “reason and logic” verses “emotion and instinct” explains the medical miracles which many of us has experienced in our clinical practice.18 In a country like India, where cultural beliefs outrage all substantial evidences, sometimes surgeon’s conscious decision depends on “circumstances” and “caregiver’s reinforcement”. Operating for third or fourth time is always unwanted nightmare for surgeon. With existing evidences of poor surgical outcome and inability of patient to bear repeated surgical stress in that poor general condition betrays even the most experienced surgeon.
To conclude, surgeon’s inner instinct and experience along with caregiver’s belief in together, can sometimes dominate the existing evidences. As Darwin has said that “the very essence of instinct is that it is followed independentlyof reason”, and so is decision to operate or not especially in cases of malignant stroke or POHI. The literature guides us with statistical and factual data but every human being demands a different approach.
None.
The author declares no conflicts of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.