Journal of
eISSN: 2373-6410


Case Report Volume 5 Issue 1
CentraCare Neurosciences, St. Cloud, USA
Correspondence: Muhammad Shah Miran, MD, CentraCare Neurosciences, 1406 6th Avenue North, St. Cloud, MN, USA, Tel 320-255-5791, Fax 320-255-5882
Received: June 14, 2016 | Published: August 12, 2016
Citation: Defillo A, Miran MS, Peterson M, Roering L, Shea K,et al (2016) Microangiopathic Occlusion of a Perforating Prepontine Long Circumferential Artery Presenting with Lower Motor Neuron Facial Weakness: Clinical and Radiological Correlation. J Neurol Stroke 5(1): 00166. DOI: 10.15406/jnsk.2016.05.00166
Case Description: A 79-year old male patient with myelodysplastic syndrome associated with severe neutropenia, thrombocytopenia, anemia, hypertension, and hyperlipidemia was admitted for pneumonia secondary to influenza A. Two weeks later he presented with new symptoms of acute dysarthria, and left facial weakness involving his upper and lower face; the following day he developed left arm weakness. Admission computed tomography (CT) and MRI scans revealed an acute ischemic stroke (AIS) in the right posterior frontal cortex. The initial MRI was reported negative for pontine lesions. Anatomically, the cortical infarct could not explain his left lower motor neuron cranial nerve VII (LMN CN VII) facial weakness distribution because in a cortical lesion the upper half of the face would be expected spared due to contralateral cortical innervation. Upon review of the MRI, the initial hyperintensity seen on Fluid-Attenuated Inversion Recovery (FLAIR) was overlooked and later identified as an acute stroke in the vicinity of the perforating prepontine long circumferential artery affecting the CN VII nucleus.
Conclusion: In the absence of earache, active infection, and/or inflammation, a sudden onset facial palsy, lower motor neuron distribution, must point to a pontine microangiopathic infarct until proven otherwise. Under these circumstances, maintaining a high level of suspicion is of paramount importance.
Keywords:Pontine tegmentum acute ischemic stroke, Perforating prepontine long circumferential artery, Lower motor neuron facial palsy, Diffuse Weighted Imaging MRI, Earache
AIS, Acute Ischemic Stroke; MRI, Magnetic Resonance Imaging; LMN CN VII, Lower Motor Neuron Cranial Nerve VII; CT, Computed Tomography; DWI, Diffusion Weighted Imaging; MDS, Myelodysplastic Syndrome; FLAIR, Fluid-Attenuated Inversion Recovery; HVS, Hyperintense Vessels Signal; T1WI, T1-Weighted Images
Pontine infarcts account for 7% of all ischemic strokes.1,2 Within this group, the microangiopathic variant affecting the pontine tegmental location, specifically the area involving the infranuclear portion of the VII cranial nerve, is very atypical. Our primary goal is to describe a perforating prepontine long circumferential artery occlusion affecting the CN VII nucleus. To our knowledge, there are only a handful of cases previously accounted.2-5
The secondary goal of this report is to compare the similar clinical characteristics, including signs, symptoms and radiological findings among these cases. Of note, these lesions appear to be radiologically misdiagnosed, despite showing as punctuate ≤5mm in size enhancing lesions on MRI diffusion weighted imaging (DWI).2-4 Additionally, it seems male gender, hypertension, and hyperlipidemia are all associated risk factors.2,4,5
A 79-year old male patient with myelodysplastic syndrome (MDS), hypertension, and hyperlipidemia was admitted for pneumonia secondary to influenza A and sepsis. Patient had MDS-associated neutropenia (23.5%), thrombocytopenia (Platelets: 18000/UL), and anemia (Hemoglobin: 6.4g/dl). His chest x-ray suggested pneumonia, and he tested positive for the influenza A virus. Broad spectrum antibiotic therapy along with Tamiflu and Voriconazole was initiated. Over the course of several days his clinical symptoms improved. Two weeks later, he presented with acute onset LMN CN VII facial palsy (Figure 1). On the following day he developed left arm weakness.

Figure 1 Photograph of the patient depicting a left peripheral-type CN VII facial paralysis. Of notice is involvement of the upper and lower face, ptosis, facial asymmetry and decreased nasolabial fold.
CT and MRI scans revealed an AIS in the right posterior frontal cortex (Figure 2C, 2D & 2E). Originally a left tegmental enhanced lesion was overlooked as a non-specific focus of signal prolongation which was interpreted as small vessel disease (Figure 2A & 2B). There was no other acute infarct identified on MRI, as well as the MRA was non-contributory.
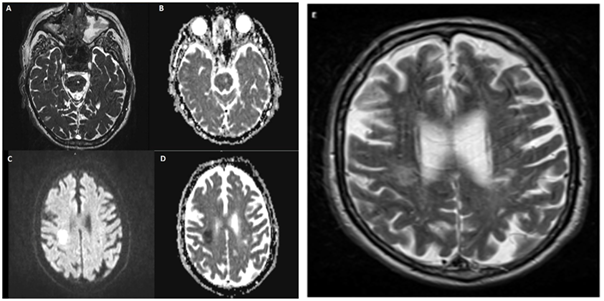
Figure 2 A & B. Axial T2 and ADC showing signal changes in the left cerebral peduncle, ventrolateral pontine tegmentum region, this signal prolongation is characteristic of microagniopathic ischemia. C, D & E; DWI, ADC & T2 images demonstrating restricted diffusion in the right frontoparietal centrum semiovale region suggesting a focal a focal non-hemorrhagic infarct A: T2, B: ADC, C: DWI, D: ADC, E: T2.
Anatomically, because involvement of upper and lower face the cortical infarct could not explain his current neurological deficit (Figure 1). Upon review of the MRI, the initial hyperintensity seen on Fluid-Attenuated Inversion Recovery (FLAIR) was interpreted as a hyperintense vessels signal (HVS) in the vicinity of the perforating prepontine long circumferential artery and not as an acute stroke.
Through a multidisciplinary approach led by oncology and stroke neurology, it was decided that the patient was not a candidate for tissue plasminogen activator (tPA), because of the increased risk of bleeding due to his existing thrombocytopenia. For the same reason aspirin therapy was also not initiated.
Clinically during the first week following his stroke the patient’s speech started to improve; however, his facial asymmetry did not. During the second week his left arm weakness started to recover slowly. On the third week, at discharged to a home facility, he continued to be hemiparetic with a persistent LMN VII facial weakness.
Occasionally, clinical signs and symptoms of a stroke which identify the location of the ischemic event may be misinterpreted or confusing. This is especially true in the case of microangiopathic stroke. Equally challenging is the fact that ischemic events related to thromboembolic sources can present within multiple locations, making clinical interpretation more difficult. Maintaining a high level of suspicion in conjunction with an advanced clinical knowledge of vascular anatomy becomes essential for making the accurate diagnosis.
Pontine infarcts represent around 7% of all ischemic events, and isolated pontine strokes contribute to around 15% of all posterior circulation infarcts.1,2
The pontine facial motor nucleus consists of a dorsal and ventral divisions that contain lower motor neurons supplying the muscles of the upper and lower face, respectively.6-8 The dorsal division receives bilateral upper motor neuron fibers while the ventral division receives input from contralateral fibers only, hence producing two distinct types of facial weakness; central or upper motor which involves the facial corticobulbar-supranuclear pathway, and peripheral, infranuclear, or lower motor neuron which involves the tegmentum of the pons.4,5 Lesions affecting the corticobulbar tract between the cerebral cortex and the facial motor nucleus in the pontine tegmentum involve the fibers to the ventral division. However, ipsilateral fibers to the dorsal division are unaffected, so clinically this will manifest as weakness of the contralateral lower face only. While infranuclear, peripheral, lower motor lesions manifest as weakness of ipsilateral upper and lower face due to involvement of dorsal and ventral divisions.6-8
Stroke related-isolated central type weakness is rare; however, peripheral-type ischemic events are even rarer. The pathophysiology behind such an uncommon condition is linked to focal microangiopathic occlusion of the perforating branches of the prepontine circumferential group.2-5 Radiologically, these types of strokes tend to be overlooked by radiologists, as demonstrated in this short series where all 5 cases were initially reported negative for a tegmental pontine stroke.2,3,4
Bell’s palsy is a frequent neurological condition accounting for 72% of facial weakness.2,9 It consists of an acute lower motor neuron facial paralysis, which is often preceded by a history of severe aching pain in and around the ear during the 24 hours prior to onset.10 Different than Bell’s palsy of viral or inflammatory origin, there are no pain symptoms with LMN CN VII facial palsy due to stroke. This is a diagnostic clue for physicians. With Bell’s palsy, there is an identifiable swollen or entrapped CN VII at the level of the internal acoustic meatus identifiable on CT-scan or MRI (Figure 3).10,11 On the other hand, in the case of perforating prepontine long circumferential artery occlusion, the CN VII structure is normal. Under these circumstances, a CT-scan with and without contrast, as well as a CT-angiogram may be insufficient. We propose that DWI MRI may be used as a gold standard for investigation. However, as reported by Oppenheima et al.,12 a false-negative DWI study is not uncommon during the first 24 hours of ischemic stroke, This is especially true for the vertebrobasilar territory distribution strokes.
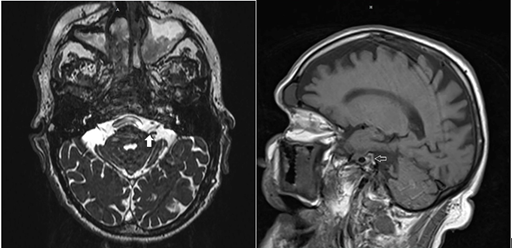
Figure 3 A & B. MRI demonstrates a structurally normal CN VII (Arrow heads) entering the internal acoustic meatus with no evidence of swollen and/or entrapped nerve.
Similar to previous cases, the tegmental pontine stroke was overlooked during the initial MRI. It is important to emphasize that hyperintensity of the ischemic brain in acute strokes is seen on FLAIR as early as 4 to 6 hours after the ischemic event, at a time when T1-weighted images (T1WI) and T2-weighted images (T2WI) are usually normal. FLAIR may detect decreased flow in the arterial bed during the acute phase of stroke. These slow-flowing arteries are depicted by FLAIR as hyperintensities against darker brain tissue leading to the hyperintense vessels sign (HVS).13 Acute occlusion of a perforating artery on top of hypoperfusion due to chronic small vessel disease is another possible explanation for this clinical manifestation and imaging.14
Another possible location for a brainstem stroke presenting with LMN CN VII facial palsy, different from the tegmental pons, is the one described by Ahn et al.4 As the corticobulbar tract descend from the pons into the ventromedial upper medulla, the tract decussates and subsequently ascend to the dorsolateral portion of the medulla; here the fibers synapse with the contralateral facial nucleus, stroke-related isolated LMN CN VII facial palsy can equally occur at this location, although extremely uncommon.4 In both circumstances the radiological infarct volume sizes is usually small or punctuate (≤5mm) and well circumscribed to the posteromedullary or pontine tegmental portion at the vicinity of the facial nucleus pathway. These anatomical areas are normally innervated by the perforating branches of the prepontine circumferential arteries.2-5
From the clinical point of view, there is a clear male predominance with hypertension and hyperlipidemia being possible associated risk factors2,4,5(Table 1). Interestingly, in 4 of the 5 cases the LMN CN VII facial palsy was on the left side (Table 1). Finally, different than Bell’s palsy where 80% of patients have an uncomplicated recovery of facial weakness (typically within 2-6 weeks), these stroke patients usually take longer to resolve10(Table 2).
|
No |
Age |
Gender |
Race |
Site of facial weakness |
Co-morbidities |
Ear pain |
Other symptoms |
Additional note |
|
1 *Agarwal et al.2 |
47 |
Male |
Asian-Indian |
Left |
HTN |
No |
Slurred speech |
MRI initially reported negative. Upon re-evaluation 4 mm infarct involving left dorsal aspect of the pons was identified |
|
2 *Novy et al.5 |
51 |
Male |
- |
Left |
HTN,HLP,DM-type II |
No |
No somatic or sensory dysfunction |
5mm acute ischemic lesion in lateral pontine tegmentum located at site of central facial nucleus corresponding to vascular territory of perforating artery belonging to long circumferential artery |
|
3 *Our reported patient |
79 |
Male |
Caucasian |
Left |
HTN, HLP, MDS |
No |
Upper extremity weakness>lower extremity weakness. Dysphagia, dysphasia |
Area of ischemia in the vascular territory of perforating pre pontine long circumferential artery |
|
4 *Oh et al.3 |
72 |
Female |
Asian |
Left |
NA |
No |
No other symptoms |
A brain diffusion-weighted MRI scan showed a hyperintense signal in the left dorsal pons in the region of the seventh nerve nucleus |
|
5*Ahn et al.4 |
83 |
Male |
NA |
Left |
HTN |
No |
Vertigo, nausea and vomiting |
Brain diffusion MRI revealed a hyper-intense signal on the left dorsolateral portion of the upper medulla and pontomedullary junction |
Table 1 Showing the clinical characteristics of previously reported cases. All ischemic events were documented on the left ventrolateral pontine tegmentum and earache was not a contributory factor
HTN: Hypertension; HLP: Hyperlipidemia; DM: Diabetes Mellitus; MDS: Myelodysplastic Syndrome; LMN CN VII: Lower Motor Neuron Cranial Nerve VII.
Characteristics |
Bell’s palsy |
Stoke related LMN CN VII palsy |
Possible etiology |
Viral, inflammation |
Thromboembolic event Perforating prepontine vessel occlusion. |
Risk factors |
Diabetes, immunodeficiency, Lyme disease, autoimmune disorders, medication and chemotherapy |
Hypertension, hyperlipidemia |
Findings on CT scan/MRI |
Swelling/ entrapment of cranial nerve VII at the level of internal acoustic meatus. |
Ischemic changes on imaging in tegmental pons or posteromedullary regions. Hyperintense Vessel Signal |
Recovery |
Quick (80% recover by 2 weeks) |
Slow, usually >2weeks |
After 12 weeks, recovery is incomplete |
Long term recovery-unknown |
|
Gender |
Equal |
Male (based on our cases) |
Table 2 Comparing the clinical attributes between stroke-related lower motor neuron CN VII deficit and Bell’s palsy
Our comments are based purely on data obtained from previous reports; we are very aware of the fact that making a conclusive clinical judgment with such minute patient sample has very limited implications. A larger sample study of similar patients is required for scientific conclusions and guidelines for such cases.
Prepontine long circumferential perforating artery stroke must be actively investigated in adult male patients with concurrent hypertension and hyperlipidemia presenting with acute onset LMN CN VII facial paralysis without associated facial or ear pain.
None.
None.

©2016 Defillo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.