Journal of
eISSN: 2373-6410


We report the case of a young woman with a history of cocaine use who presented with subarachnoid hemorrhage secondary to rupture of an aneurysm of the P1 segment of the posterior cerebral artery, treated via intracranial vascular microsurgery.
Keywords:Cerebral aneurysm, Posterior cerebral artery, Subarachnoid hemorrhage
SAH, Subarachnoidhemorrhage; CN III, Oculomotornerve
Posterior cerebral artery aneurysms are relatively rare, accounting for 1–2% of all intracranial aneurysms,1 and are located in the deep central portion of the brain.2 They may present in several forms, including saccular, dissecting, and fusiform aneurysms.3
A 29-year-old woman presented with sudden onset of headache, nausea, vomiting, and nuchal rigidity (Hunt & Hess grade II). The patient was a cocaine user and had a positive FTA-Abs and Wasserman reaction, indicative of acute syphilis.
Computed tomography of the head was consistent with a Fisher grade 3 subarachnoid hemorrhage (SAH). CT angiogram revealed an aneurysm of the P1 segment of the posterior cerebral artery (Figures 1 & 2).
The P1 segment of the posterior cerebral artery has a mean length of 6.8mm (range, 2.8-12.2mm) and a mean diameter of 1.85mm (range, 0.8-4.5mm). On average, there are 3.35 branches per segment arising from the postero-superior aspect of P1; in 96.4% of cases, they are the most proximal branches.4
The literature on P1 segment aneurysms is scarce, consisting solely of small case series. Yonekawa et al.2 reported seven cases of posterior cerebral artery aneurysms out of 1,027 aneurysms (0.58%) treated over a 10-year period. In a series of five cases, with one P1 aneurysm and one P2 aneurysm clipped via the pterional approach and three P2 aneurysms clipped via subtemporal craniotomy, the mean patient age was 54.5 years. Honda et al.5 published a series of 10 patients with posterior cerebral artery aneurysms (five male, five female; mean age, 57.6 years). Seven patients presented with SAH, two cases were discovered during a stroke work-up, and one was associated with Moyamoya disease. Three aneurysms were in the P1 segment, three at the P1-P2 junction, three in the P2 segm Despite the growing use of endovascular therapy for posterior circulation aneurysms, microsurgery is increasingly indicated as primary therapy for aneurysms of the P1 segment of the posterior cerebral artery, distal superior cerebellar artery, and posterior inferior cerebellar artery. For aneurysms of the P2 segment of the posterior cerebral artery, basilar trunk, proximal anterior inferior cerebellar artery, vertebrobasilar junction, and vertebral artery, microsurgery is indicated as second-line treatment when endovascular therapy is deemed unfavorable.7ent, and one in the P3 segment.5 In a series of 26 dissecting aneurysms, only one was located in the P1 segment.6
Our patient underwent a left pre-temporal craniotomy with dissection of the lateral sulcus and uneventful microsurgical clipping of the aneurysm (Figures 3, 4, & 5). Postoperatively, she developed severe vasospasm (Lindegaard ratio up to 6), lasting 10 days, and ipsilateral oculomotor nerve (CN III) palsy, which eventually improved (Figure 6).
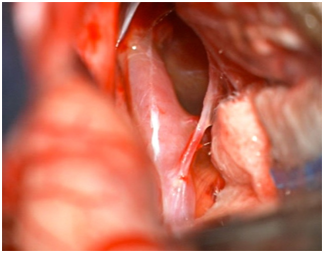
Figure 3 Control Brain CT scan, showing ischemia in the territory ofMicrosurgical view of left posterior cerebral artery and aneurysm neck.

Figure 6 Appearance of patient after microsurgical clipping of left posterior cerebral artery aneurysm.
Despite the growing use of endovascular therapy for posterior circulation aneurysms, microsurgery is increasingly indicated as primary therapy for aneurysms of the P1 segment of the posterior cerebral artery, distal superior cerebellar artery, and posterior inferior cerebellar artery. For aneurysms of the P2 segment of the posterior cerebral artery, basilar trunk, proximal anterior inferior cerebellar artery, vertebrobasilar junction, and vertebral artery, microsurgery is indicated as second-line treatment when endovascular therapy is deemed unfavorable.7
The authors declare there are no conflicts of interest or funding sources to declare.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.