Abstract
Background: Consumption of injecting drugs (mostly home-made drugs) and correspondingly needle sharing practice remains the main factor of spreading HIV among people who inject drugs (PWID) (55%) in Georgia. According to last BSS studies there are estimated 45 000 injecting drug users in the country.1,2 Significant amount of PWID still are beyond existing needle and syringe Programs (NSP) and have never tested on HIV (75%).3 The most hidden group for NSP programs are female and young PWIDs who are been considered to be one of the most vulnerable sub-population in this group. Needle and syringe program is being operating in 11 cities of Georgia and is represented by 14 harm reduction sites throughout the country. The program ensures coverage of significant portion of PWIDs (10,000-12,000 per month), and offers different services for HIV/AIDS prevention. Among delivered services Peer Driven Intervention (PDI) is one of the meaningful efforts to attract drug users to HIV prevention programs from more hidden sub-populations.4 PDI is the comparatively newly developed model for attraction the population of difficult availability for AIDS prevention programs, to facilitate distribution and consideration of the correct information, PDI reveals effective in the direction of HIV-AIDS educational prevention. Recruiting the drug users by the peers is carried out by means of monetary, promotional incentives -however it is comparatively cheap, compared to the traditional outreach model and is successfully applied for covering the large sample of the various groups of drug users - female and young drug users.5 Peers attracted by PDI are mostly never reached by any HIV programs, accordingly their knowledge and risky behavior stayed relatively unfavorable and poor.
Introduction
The objectives of this study are
- To analyze risky behaviors of PWIDs who are clients of Needle-Syringe Programs (NSP) more than 6 months and PWIDs who never have been in contact with harm reduction services and were recruited through Peer Driven Intervention (PDI).6,7
- Making comparative analysis of Risky Behavior and knowledge about injected drug related harm in PWIDs among PDI and NSP study participants.
Methods
The cross-section design and Non-Random Sampling Design Respondent Driven Sampling (RDS) - was used to recruit PWIDs that have never been in contact with HIV prevention programs (first sample) and are PDI participants, and convenience sampling to recruit PWIDs that are NSP clients for more than 6 months (second sample).8-10 The first sample recruitment commenced from the so-called “seeds”. Various characteristics of seeds were foreseen during selection. Each seed and further recruited PDI client upon filling the study questionnaire and going through the educational interview, was given 3 coupons with the unique codes, according to which each participant was entitled to bring along 3 more client. Without this coupon the client should not been involved into the program.
Each study participant was encouraged monetary awards for filling the questionnaire, teaching and attraction of the other PWIDs/further PDI clients. On its hand, additional incentives were envisaged according to number of correct answers (according to educational module test), as well bonuses were foreseen for recruiting women and the young PWIDs (18-25).11-13
The study had multisite and included 9 NSP centers in 8 cities of Georgia. Data collection has been done between March and September 2012. Total sample size composed of 2342 PDI participants and 1154 NSP clients. Structured questionnaire that underwent pilot examination was applied for the both sample. The criteria for inclusion in the study were defined:
- Respondent should be 18 year and over
- Inclusion in the study should be voluntary
- Person should not have any problem related to thinking, speech and mental health
- Person should not be included in any harm reduction program before (PDI study)
- Should have been included in harm reduction more than 6 month period (NSP study).
Data processing and analysis
For data processing statistic packet for social science (SPSS software version 19.0) was applied. In order to avoid any incompliance, the frequencies were recalculated with the purpose to check all the variables and the categories. Afterwards, the database was cleared according to the logical transfers of the questionnaire and the base testing was held for preciseness and completeness of the data. The records were checked by means of the so-called cross tabulation, through which the incompliant measurements were identified given inside the data of one respondent.
While processing the data, generally the descriptive statistical methods were applied for. In order to avoid any incompliance, the frequencies were recalculated with the purpose to check all the variables and the categories. In case of categorical variables, for detection of association among the variables the Pearson Chi-Square rate was applied for. The reliability level p<0.05 was defined as the statistically important.
Results
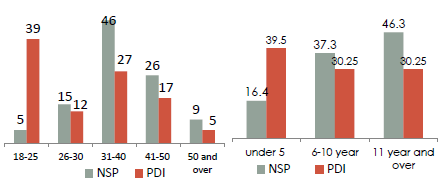
PWIDs attracted by PDI (first sample) are younger – the average age 32 (SD=8.5; min=18; max=67; mode 24; median=30) compared with the beneficiaries of NSP-average age 37.7 (SD=8.5; min=18; max=66, median=37). PDI became possible to reveal the young PWIDs compared with NSP. In particular, the young PWIDs group (18-25 years) is 39% of those covered with the PDI, while the coverage of this group in NSP did not exceed 5%. PWIDs recruited by PDI mostly are beginner drug users (Figure 1&2). Accordingly they have lower injection experience (39.5% - under 5 year) in comparison to PWIDs in NSP sample (46.3% - 11 year and over). The majority of PDI study participants - 63.2%, have never been undergone to HIV testing14 (Figure 2). Important was to find out that about half of NSP beneficiaries were tested on HIV a year ago or earlier, and the program includes beneficiaries with no HIV test experience (12.4).
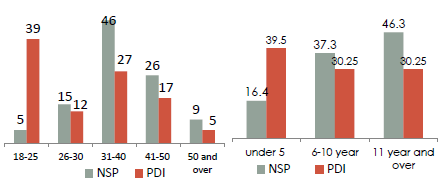
Figure 1&2 Testing practice on HIV. Among PDI study beneficiaries who had sexual relations with more than 1 partner condom use practice is lower than among NSP Respondents (Figure 3), who almost twice more often verify permanent use of condom with more than one partner. Unsafe sex behavior is mostly revealed in Batumi and Poti (seaside cities)
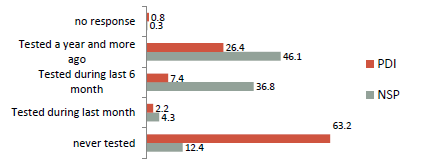
Figure 3 Testing practice on HIV (%).
Discussion
According to study results different characteristics of the both sample were revealed:
- PDI recruited PWID reveal new and young drug injectors, access to which is quite significant in terms of effective means of harm reduction/HIV prevention.15,16 Currently these groups of PWIDs are rather hidden groups for existing NSP programs in the country and require intervention targeted to them.17 Besides the young are still beginners, their drug injection experience does not exceed 5 years and they do not think they need help of any kind. Therefore, they refer rarely to the harm reduction programs. Attraction of the young PDI drug users undoubtedly is the successful result of such intervention, but it is also important to maintain such attracted population in NSP program.
- PDI recruited the large group of PWIDs with small injecting experience. Educational intervention of the indicated young users’ group regarding harm reduction issues and testing on various viral infections might be considered as significant intervention for achievement of minimization of the harms caused by the injection drug use (safe injection, overdose, safe sexual practice).
- As the way of transmissions, drug injection practice (55%) remains the most common way to transfer the HIV infection in the country. Taking into account strict drug law regulations, PWIDs represent the most hidden group and difficult to reach HIV testing services (Figure 3). Study revealed that majority of the PDI study participants - 63.2% has never been undergone to HIV testing; besides, meaningful was to depict that the HIV testing among them was held a year ago or earlier. Seams, that PWIDs, uncovered by harm reduction programs, have limited access to free HIV services, have low awareness about the importance about testing on HIV, have other barriers to undergo timely HIV test – as a result the country experiences high rate of late HIV diagnose among this group alongside with other high risk groups. Accordingly increasing the scale and scope of harm reduction programs will enable PWIDs increase their awareness and HIV testing rate.
- While comparing of the data of both studies, it was verified, that the practice of sharing of the injection facilities during the various period of time, almost equally is stated by the beneficiaries of NSP as well as the respondents of the PDI. It is of great interest that notwithstanding participation into NSP program definite part of the beneficiaries still refers to the risk behavior.18 However worth to mention that PDI beneficiaries, in comparison with NSP, state that they preferably share it with more than 1 needle partner, accordingly they more refer to risk behavior.
- Regarding safe sexual practice the study revealed that NSP study participants almost twice more often verify permanent use of condom with more than one partner, in comparison with PDI respondents,19 who reveal more unsafe sexual practice and rarely and never use condoms with them. Probably, this is caused by the fact that the beneficiaries of NSP by means of the harm reduction centers have more access to the free of charge condoms, the appropriate informational and educational materials, and may also receive the proper specialists’ consultancies (Figure 4-6).
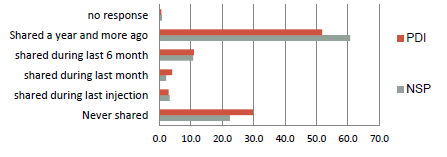
Figure 4 Needle/syringe sharing practice among IDUs during last 6months (%).
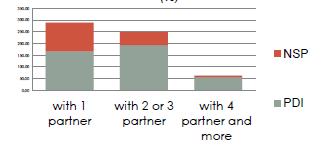
Figure 5 Needle/syringe sharing with partners (%).
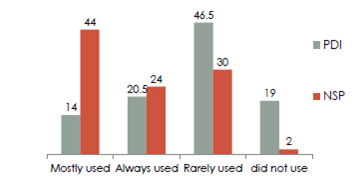
Figure 6 Condom using practice among IDUs who had more than 1 sex partner during last 30 days (%).
Regarding Needle/Syringe sharing practice it is important to note that in both cases needle sharing practice mainly was observed in more than 1 year ago. Significant difference in needle sharing risky behavior was not revealed among participants of both samples. However, while sharing of injection instruments, NSP beneficiaries preferably share it with 1 person, while PDI respondents more refer to the risk behavior and share the injection equipment with more than 1 partner (Figure 4). The results of PDI verify that among those who have never held testing for HIV infection, the sharing practice is verified with 70.7% of the beneficiaries, which is rather high indicator of the risk behavior.
Conclusion
Based on this study following findings were revealed:
- PDI had enabled to recruit new and young drug injectors, who are rather hidden groups for existing NSP programs in the country.20
- Needle sharing practice is common for both groups, but PDI clients mostly are sharing them with more than 1 partner in comparison with NSP clients.
- Large number of PDI clients has never tested on HIV.
- In comparison to NSP clients, PDI recruited PWIDs have unsafe sex behavior – they have several sex partners to whom they use condoms rarely or never.
- Unfortunately both samples demonstrate the same rates of sharing of injecting equipment. Future research is needed for development of new strategy that will reduce risky injecting practice.
Study results will be applied for:
- Developing recommendation for further development of harm reduction programs.
- Targeting proper actions and redesigning existing interventions for enable more positive results in terms of safe behavior among program beneficiaries.
Acknowledgments
GHRN and the author express their deep gratitude and acknowledgement to the Global Fund Project to Fight AIDS, Tuberculosis and Malaria for providing us with the opportunity to conduct such a meaningful studies; We thank I. Kirtadze for methodological arrangement of the research, for assistance during the statistical processing and for commenting of the report, thanks to the researchers of the Addiction Research Center “Alternative Georgia” - Irma Kirtadze and David Otiashvili Especial appreciation goes to Mzia Tabatadze MD. MPH. PhDc, HIV Policy and Advocacy Expert, Research Triangle Institute International for her input in study report preparation and writing process.
Conflicts of interest
References
- Kvashilava K. Research of the Legislation of Georgia towards overdosing while illicit use of drugs. Center for protection of the Constitutional Rights. 2012.
- Kirtadze I. Assessment of the risk behavior among the injection drug users. 2008.
- Assessment of the cost efficiency of the programs of syringes exchange, UNAIDS Georgian Office, 2011.
- Douglas D Heckathorna, Robert S Broadhead, et al. AIDS and social networks: HIV prevention through network mobilization, Sociological Focus. 1999;32(2):159‒179.
- Robert S Broadhead, Douglas D Heckathorn, Jean‒Paul C, et al. Drug Users Versus Outreach Workers in Combating AIDS: Preliminary Results of a Peer‒Driven Intervention. Journal of Drug Issues. 1995;25(3):51.
- Broadhead RS, Heckathorn DD, Weakliem DL, et al. Harnessing Peer Networks as an Instrument for AIDS Prevention: Results from a Peer‒Driven Intervention. Public Health Rep. 1998;113(S1):42‒57.
- Donoghoe MC, Stimson GV, Dolan K, et al. Changes in HIV risk behavior in clients of syringe‒exchange schemes in England and Scotland. AIDS. 1989;3(5):267‒272.
- Douglas D Heckathorn. Extensions of respondent‒driven sampling: Analyzing continuous variables and controlling for differential recruitment. Sociological Methodology. 2007;37(1):151‒207.
- Douglas D Heckathorn. Respondent‒driven sampling: a new approach to the study of hidden population. Social problems. 1997;44(2):174‒199.
- Douglas D Heckathorn, Salaam Semaan, Robert S Broadhead, et al. Hughes Extensions of Respondent‒Driven Sampling: A New Approach to the Study of Injection Drug Users Aged 18–25. AIDS and Behavior. 2002;6(1).
- Lomidze G. Research of supervision over the behavior among the women drug‒addicted, the Union “Step into the Future”. 2012.
- Research of the needs of the women drug users. Georgian Harm Reduction Network. 2012.
- Kirtadze I, Otiashvili D, O'Grady KE, et al. Twice Stigmatized: Provider's Perspectives on Drug‒ Using Women in the Republic of Georgia. J Psychoactive Drugs. 2013;45(1):1‒9.
- David Otiashvili. How Effective is Street Drug Testing? Addiction research Center Alternative Georgia. 2010.
- WHO/UNODC/UNAIDS. Technical guide for countries to set targets for universal access to HIV prevention, treatment and care for injecting drug users. Geneva. 2012.
- WHO/UNODC/UNAIDS. Technical Guide for countries to set targets for universal access to HIV prevention, treatment and care for injecting drug users. Geneva. 2009.
- Batselashvili L, Sinjikashvili M, Chelidze M, et al. Results of piloting of Peer Driven Intervention – did we reach targeted population? Addiction Research Center, Alternative Georgia. 2011.
- Des Jarlais C, Perlis T, Friedman SR, et al. Behavioral risk reduction in a declining HIV epidemic: Injection drug users in New York City, 1990‒1997. Am J Public Health. 2000;90(7):1112‒1116.
- Douglas D Heckathorn, Robert S Broadhead, Boris Sergeyev. Methodology for Reducing Respondent Duplication and Impersonation in Samples of Hidden Populations. Journal of Drug Issues. 2001.
- Study of the factors acting over the risk behavior of the drug‒addicted (injection and sexual risk behavior) New Vector, 2011.

© . This is an open access article distributed under the terms of the,
which
permits unrestricted use, distribution, and build upon your work non-commercially.