Journal of
eISSN: 2373-6453


Opinion Volume 2 Issue 2
Institute of Progressive Medicine, USA
Correspondence: W John Martin, Institute of Progressive Medicine, 1634 Spruce Street, South Pasadena, CA 91030, USA, Tel 626-616-2868
Received: January 17, 2015 | Published: February 13, 2015
Citation: Martin WJ (2015) Chimpanzees Inoculated with Cytomegalovirus Contaminated Polio Vaccines may Explain Origin of HIV-1: Implication of Treatment in the Developing World. J Hum Virol Retrovirol 2(2): 00035. DOI: 10.15406/jhvrv.2015.02.00035
The reported early 20th century origin of human HIV-1 infection assumes a single group M (main) ancestral virus transmission to humans from a simian immune deficiency virus SIV (cpz) infected chimpanzee. The possibility remains that several chimpanzees may have individually transmitted related but slightly different group M HIV-1 infections to humans in the mid to late 1950’s. It is proposed that these events may have been the inadvertent consequence of inoculating stealth adapted rhesus cytomegalovirus (RhCMV) contaminated experimental polio vaccines into chimpanzees.
Keywords:HIV, AIDS, CMV, SCMV, SIV, Chimpanzees, Monkeys, Polio vaccine, Africa
SIV(cpz), Simian Immunodeficiency Virus of Chimpanzees; CMV, Cytomegalovirus; RhCMV, Rhesus Monkey Cytomegalovirus; SCMV, African Green Monkey Simian Cytomegalovirus; CPE, Cytopathic Effect
The genomic sequences of HIV-1 isolates are closely related to the sequences of simian immunodeficiency viruses of chimpanzees SIV (cpz).1 It is widely presumed, therefore, that a SIV (cpz)-derived virus can evolve into HIV. The time at which humans initially became infected with SIV (cpz) or with a SIV (cpz)-derived virus is less certain. Yet this is clearly relevant to the likely mode of virus transmission from chimpanzees to humans.
A particularly contentious issue is whether the onset of human infections predated the use of chimpanzees in the polio vaccine research conducted in Africa in the mid to late 1950’s.2-4 Support for an earlier origin of HIV has come from analyzing nucleotide sequence differences between regions of HIV amplified from a human plasma sample collected in 1959 (ZR59) and that of corresponding regions of HIV (DRC60) amplified from a patient’s biopsied lymph node obtained in 1960.2,5,6 Both the blood sample and the lymph node biopsy were from patients treated in Kinshasa (formally known as Leopoldville), in what is now known as the Democratic Republic of the Congo. The sequence data were obtained using the polymerase chain reaction (PCR).
The sequence comparisons were limited to very small fragments of the corresponding viruses, yet were sufficient to reveal approximately 11.5% nucleotide substitution.6 Both viruses were group M, representing the “main” group of HIV-1 viruses, which has largely led to the worldwide epidemic of AIDS. The other HIV-1 groups are designated O, N and P.7
Sequence comparisons between group M HIV isolates obtained in subsequent years from Kinshasa and surrounding areas of Africa, have allowed for an estimated minimum yearly time rate of nucleotide substitutions within group M HIV.8,9 When this “molecular clock” is applied to the differences between the ZR59 and DRC60 sequences, the presumed common ancestral virus is estimated to have existed approximately 40 years earlier. This dates the original or ancestral group M human infection to around 1920; well before the testing of polio vaccines.2,6
HIV-1 group’s O, N and P viruses are sufficiently distinct from group M viruses that each is considered as being derived from different SIV (cpz) infected chimpanzees.7 Yet, surprisingly, this consideration is not given to the possible separate derivation of ZR59 and DRC60 isolates from different chimpanzees. Thus, the sequence differences could have arisen within virus infected chimpanzees rather than within virus infected humans. Also not considered in the DRC60 sample is that sequence variations can exist between virus infecting different tissues, even within a single individual.10 Significant genetic differences have even been noted with human cytomegalovirus (HCMV) isolated from different sites of the same patient, in spite of the far greater fidelity of nucleotide replication of HCMV than that of HIV.11,12
The molecular clock approach to virus phylogeny can also be rendered unreliable by confounding influences that can variably accelerate the virus mutation rate.13 For example, major sequence alterations can result from genetic recombination between virus variants, as has occurred between some of the nine described subtypes (clades) of group M viruses. These are referred to as “circulating recombinant forms” (crf) and along with dual infections can pose problems in sequence-based tracing of the evolution of HIV-1.14-16
An even greater factor potentially accelerating genetic variability between HIV-1clades is co-infection with other viruses that can promote HIV replication. The prime example is CMV because it has various genes able to enhance HIV replication.17,18 Neither the ZR59 nor DRC60 patient samples were tested for coincidental CMV infection. Nor is the proposed 1920’s origin of human infection with HIV supported by compelling descriptions of AIDS-like illnesses in the ensuring 35 or so years. Based on the 1959 detection of ZR59 virus in only one blood sample of 672 tested19 and on the 1960 detection of DRC60 in tissues of only one of 27 patients samples,6 HIV was clearly not a highly prevalent infection at the time. Nor have there been any subsequent reports of finding HIV-1 sequences in other samples collected prior to 1960.
Edward Hooper3 suggested an association between the emergence of HIV and the testing of polio vaccines in the Congo, conducted under the direction of Hilary Koprowski20 of the Wistar Institute, Pennsylvania. It has been recorded that over 400 chimpanzees were used at a location called Camp Lindi, near the now abandoned Laboratory Medical de Stanleyville.4,21,22 Hooper3 successfully traced the clinical appearance of AIDS to Kinshasa in the early 1960. Based on first hand reports to the author by a now deceased individual who had worked at Camp Lindi, he correctly reported that technicians collected kidneys from primates and that the kidney tissues were finely chopped into sterile solutions. The tissues were probably not from chimpanzees, however, and were very unlikely to have been used to propagate polio vaccine virus for subsequent human use. Hooper3 has incorrectly assumed that the CHAT vaccine administered to humans was grown in cultured kidney cells of chimpanzees in a manner leading to its contamination with SIV(cpz). Subsequent DNA analysis of the CHAT vaccine clearly shows that it was produced using cultured kidney cells from rhesus monkeys.23 The name CHAT was derived from a child, Charlton, purposely inoculated with polio virus as part of the selection process for an attenuated virus.21,22 It is noteworthy that the virus stocks from which the CHAT strain was ultimately selected had previously been passaged in rodents, chick embryos, monkeys and other humans.
Albert Sabin24 detected non-polio, cytopathic virus within the CHAT vaccine. He noted that while it was difficult to maintain and transmit the cytopathic effect (CPE), it did indicate an unknown virus contaminant. Indirect evidence for the existence of a pathogenic agent within Camp Lindi includes the unexplained illnesses and demise of many of the imported chimpanzees. Based on the firsthand account, the supplier of the chimpanzees had to greatly extend his catchment areas for obtaining chimpanzees to help compensate for the illness-related losses of chimpanzees. The extended catchment area was likely to have included Cameroon, where the SIV(cpz)precursor(s) of HIV-1 is/are particularly prevalent.
Not only were the chimpanzees becoming sick, but the firsthand account also described a wasting illness among several of the animal handlers. It was locally referred to as “thin man syndrome.” Although no longer retrievable from Medline, a previously posted article described a number of the workers as being admitted to hospital because of rhino sclerosis caused by Klebsiella rhino scleromatis bacteria. This illness is a rather unusual but well recognized complication of AIDS.25 It is not unreasonable to suggest that these animal handlers may have been the source of different groups and subtypes of what has become HIV-1. In other words, some degree of genetic diversity within group M HIV-1 may well have initially occurred within infected chimpanzees, rather than all group M HIV-1 infections having resulted from a single infected human.
Molecular studies on various polio vaccines conducted by the National Institute of Biological Standards and Controls in the United Kingdom showed that 52/74 vaccines produced in primate kidney cell cultures were contaminated with CMV of the monkey species used to produce the vaccine.26 The analysis included the CHAT vaccine and showed that it contained DNA of rhesus monkey CMV (RhCMV). While the researchers were unable to culture live virus from the stored vaccine samples, this may well reflect inadequate culturing techniques, especially for viruses that have undergone “stealth adaptation” (discussed below). Similarly, a difference in culturing techniques could well explain Dr. Sabin’s positive findings and the insistence by Koprowski20 that his vaccine was not contaminated. It is not unreasonable to suggest that many of the chimpanzees at Camp Lindi were inoculated with RhCMV contaminated experimental polio vaccine. Co-infection with RhCMV may have led to the emergence of HIV-1 from SIV(cpz) within the inoculated chimpanzees. This concept is pictorially reflected in Figure 1.
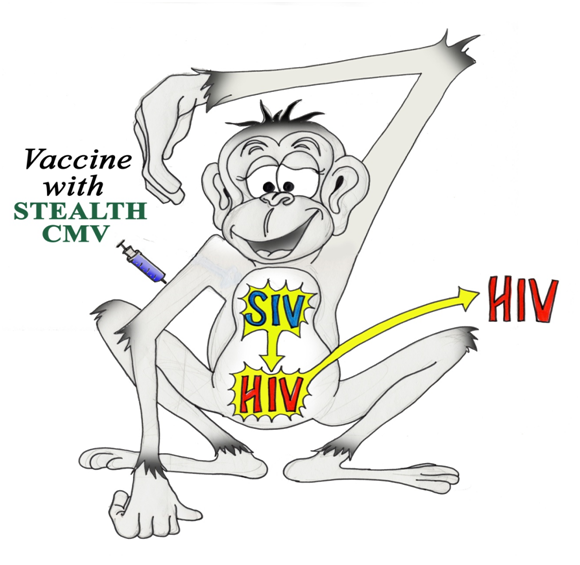
Figure 1 The possible evolution of SIV (cpz) towards HIV as a consequence of inoculating experimental polio vaccine containing stealth adapted cytomegalovirus’s of rhesus monkeys. CMV induced genetic changes in SIV may have facilitated the transfer of modified forms of evolving HIV-1 viruses into humans. This could explain the molecular differences between 1959 and 1960 identified group M HIV, rather than assuming that only a single transfer of an ancestral group M HIV-1 years had occurred approximately 40 years prior to HIV being first identified.
The importance of culture technique was subsequently revealed in the successful isolation of several atypical African green monkey simian cytomegaloviruses (SCMV) from patients with a range of neuropsychiatric illnesses.27-31 Under normal virus culturing conditions, these viruses tend to produce a rather transient CPE due to a repair process mediated through the alternative cellular energy (ACE) pathway.27,30 The intensity and persistence of the CPE are enhanced by using serum free culture medium and by the frequent replacement of the medium. Of further interest, the viruses do not ordinarily evoke an inflammatory response in the patients from whom they are isolated or in animals inoculated with the viruses. The lack of inflammation is explained by the loss or mutation of the genes coding for the relatively few antigens normally targeted by the cellular immune system. This immune evasion mechanism is termed stealth adaptation and can potentially occur with all types of viruses.27-31
A stealth adapted African green monkey simian cytomegalovirus (SCMV) has shown a rather remarkable genetic instability with multiple nucleotide changes.32 It can be expected, therefore, that stealth adapted RhCMV and SCMV, which have been inadvertently introduced into humans, have acted as HIV-1 promoters and facilitated the further formation of virus subtypes. There are five recognized subspecies of chimpanzees (Pan Troglodytes).33 The SIV (cpz), which most closely resembles HIV-1, occurs near exclusively in Pan troglodyte stroglodytes, (Ptt, or Central chimpanzee). There is a lower occurrence of a related SIV (cpz) in Pan troglodytes schweinfurthii, (Pts or Eastern chimpanzee), and an absence of SIV(cpz) in the remaining three subspecies.34 The majority of chimpanzees used in Camp Lindi were of the Pts sub species since this subspecies mainly inhabits eastern Congo. Still, given the heavy demand for chimpanzees and as suggested by the individual with firsthand experience of Camp Lindi, at least some of the chimpanzees at Camp Lindi were likely to have been SIV (cpz) infected Ptt subspecies.
The SIV (cpz) infection rate is quite variable among different colonies of Ptt and Pts chimpanzees.35 Moreover, sequence analysis shows that SIV (cpz) arose in the early 1900’s from a recombination between the SIV of red-capped mangabey monkeys and that of greater spot-nosed monkeys.36 Monkeys and chimpanzees were used in various research endeavors conducted in West Africa in the early 1900’s. These include studies on malaria,37 yellow fever38 and undoubtedly on other pathogens.39 It seems more likely that monkey tissues would have been injected into chimpanzees than for a hapless chimpanzee to acquire dual infections from eating meat from both infected species. This latter opportunity had existed for eons, yet had not occurred before the 20th century. Similarly, it is dubious to attribute the original human HIV-1 infection to someone eating bush meat from an infected chimpanzee, or having an open wound while handling infected tissues.40
The important message is that vaccine development involving the inoculation of pathogens into foreign species can potentially lead to the formation of new pathogenic variants from genetic alterations. The 1950’s decision to propagate attenuated polio virus in cultured kidney cells obtained from CMV infected rhesus monkeys allowed the interaction of Rh CMV with SIV (cpz). RhCMV induced nucleotide changes in SIV (cpz) could then have enabled the virus to pass into humans.
The switch from rhesus to African green monkeys as the source of kidney cells for the production of polio vaccines occurred around 1961. The African green monkeys used throughout the 1960’s and into the 1970’s were commonly infected with SCMV.41 It is possible, that co-infections of humans with stealth adapted SCMV and HIV led to further developments of the HIV genome. Even in its own right, stealth adapted SCMV is pathogenic for humans and dual infection with HIV could well contribute to the clinical characteristics of the AIDS epidemic.27,28,42
Consideration of the possible reasons for the emergence of HIV may help prevent future virus epidemics. The basic theme of this article is to underscore the potential hazard of intentional or inadvertent cross species transfer of pathogenic agents, especially viruses. The process of inoculation can bypass certain barriers that have successfully avoided the intermingling of viruses from different species. Similarly, the cultivation of human viruses in primary cultures of cells from known virus infected animals, as has been the case with many human vaccines, can encourage the development of new forms of pathogenic viruses. The timing of the solitary or repeated events leading to group M, HIV-1 infection in humans has yet to be definitively answered.
The Institute of Progressive Medicine is a component of MI Hope Inc., a public charity. The Figure was drawn by Sarah Martin Domb, MD.
None.

©2015 Martin. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World AIDS Day (December 1) is an International day to support global efforts for prevention and care against HIV infection all around the world. So, considering this day we are enthusiastic to publish articles on this topic to spread knowledge to all our readers. Take the opportunity in sending your valuable articles and get the best discount of 30% for your submissions to our Journal of Human Virology & Retrovirology (JHVRV).
World AIDS Day (December 1) is an International day to support global efforts for prevention and care against HIV infection all around the world. So, considering this day we are enthusiastic to publish articles on this topic to spread knowledge to all our readers. Take the opportunity in sending your valuable articles and get the best discount of 30% for your submissions to our Journal of Human Virology & Retrovirology (JHVRV).