Journal of
eISSN: 2374-6947


Research Article Volume 11 Issue 2
1Department of Endocrinology & Metabolism, San Raffaele Pisana Institute, Rome, Italy
2Department of Research, Nefrocenter Research Network, Torre del Greco, Italy
Correspondence: Felice Strollo, Department of Endocrinology & Metabolism, San Raffaele Pisana Institute, Rome, Italy
Received: November 12, 2024 | Published: November 28, 2024
Citation: Strollo F, Guarino G, Satta E, et al. Should we cure or care people living with type 1 diabetes? a survey. J Diabetes Metab Disord Control. 2024;11(2):110-115. DOI: 10.15406/jdmdc.2024.11.00287
At the moment of type 1 diabetes mellitus (T1DM) diagnosis communication, adult patients experience disorientation, fear and uncertainty in front of permanent, adverse changes in their habits before considering insulin as a powerful tool to control disease, improve quality of life, and prevent severe complications. Indeed, an adequate series of services is required to grant not only medical but also humanistic assistance aimed to interpret persons’ needs and whish. This survey had 146 people with T1DM consecutively referring to the outpatient wards of a Diabetes Consortium in Italy complete a a self-administered questionnaire to examine some crucial moments experienced by at the time of diagnosis, during the educational process, and when feeling the voice tone of the professionals revolving around the treatment process while sending out their messages. A merciless picture emerged from the questionnaires, being most participants unsatisfied with the healthcare team approach, which they judged too technical and less prone to effective education. A missing point was especially helpful training on practical aspects of diabetes treatment, especially regarding appropriate insulin injections technique and the severe long term disease consequences complications deriving from poor compliance to them. Much remains to be done to improve the daily clinical, social, and personal conditions of persons with T1DM as pursuing the goal of euglycemia when treating diabetes involves a whole, complex process, including a series of actions aimed at supporting PwD in improving their interpersonal relationships, understanding their individual needs, and breaking down the barriers raised by old-fashioned, outdated professional attitudes.
Keywords: Type 1 diabetes, education, depression, diabetes care, nurses
At the moment of type 1 diabetes mellitus (T1DM) diagnosis communication, adult patients experience a complex series of emotions, including an invasive sense of fear and uncertainty in front of the need to inject insulin for the rest of their life repeatedly, and pending future complications. What might be the scariest and most disorienting message to accept is the permanent, adverse change in their habits.1 On the other hand, the desire to regain control of their health and live a full and active life let’s hope and determination take the lead when considering insulin as a powerful tool to control disease, improve quality of life, and prevent severe complications.2 At the bottom of it all is acceptance, i.e., the feeling that, despite the challenges, it is possible to adapt and move forward with the right support. The diabetes community, family, friends, and health professionals play a crucial role in such a journey by offering support, information, and encouragement. Nevertheless, it is not so easy to accept any chronic illness causing a deep review of habits, propensities, and expectations and sometimes fear, depression, and poor quality of life.3,4
Depression and diabetes mellitus (DM) are two conditions that often influence each other. Indeed, depression is common among people with DM and can cause poor adherence to treatment, diet, and lifestyle, thus impairing disease management.5 At the same time, DM can increase the risk for depression through disease management-related stress.6,7 That is why both depression and metabolic derangement require an integrated approach, including medical (i.e., antidepressants as needed) and psychological care as helpful tools to attain reasonable disease control.8
In Italy, healthcare is universally granted to everyone, almost free of charge, with minimal citizen participation in healthcare spending. Persons with DM (PwD) have been guaranteed treatment and assistance since the dedicated Law 115 was approved on March 26, 1987. The latter defined DM as a condition of high social interest and protected the right to health through a network of specialized services widespread throughout the national territory.
In primary care, General Practitioners (GPs) ensure DM prevention and diagnosis while entrusting specialist services with the diagnostic validation and screening, as well as management and follow-up of chronic complications, and share the treatment plan using the so-called "innovative" drugs (Sodium-Glucose Transport Protein 2 Inhibitors [SGLT2-is], Glucagon-Like Peptide-1 Receptor Agonists [GLP1-ras], and Dipeptidyl-Peptidase-IV Inhibitors [DPP-4-is]) included in the national register form of the Italian Medicines Agency (AIFA), and insulin.9 However, a good organization of care requires an adequate series of services granting not only medical but also humanistic assistance, i.e., taking care of and interpreting "persons" with their fears and needs across the board.10
This survey aims to examine some crucial moments experienced by people with T1DM at the time of diagnosis, during the educational process, and when feeling the voice tone of the professionals revolving around the treatment process while sending out their messages.
146 adults with T1DM aged between 18 and 40 years and with a disease duration of less than 5 years consecutively referring to our outpatient wards self-completed an 11-item non-validated, home-made, yet user-friendly multiple-choice questionnaire addressing the following areas: (i) anamnestic details, including disease duration, number of daily injections, and daily insulin dose, and data concerning diagnosis communication and the educational path followed; (ii) relationship with the care team and degree of satisfaction; (iii) unmet needs. Only upon request did they receive support from Health Care providers (HCP). The 11 items are reported in Table 1.
|
1 |
Diagnostic setting |
(i) Outpatient clinic |
|
(ii) Hospital |
||
|
2 |
Who communicated the diagnosis? |
(i) I don’t remember |
|
(ii) Doctor + Nurse |
||
|
(iii) Nurse |
||
|
(iv) Doctor |
||
|
3 |
At the time of diagnosis, did you understand what diabetes was? |
(i) Yes |
|
(ii) No |
||
|
(iii) I don’t remember |
||
|
4 |
Did you undergo educational training on diabetes? |
(i) Yes |
|
(ii) No |
||
|
(i) I don’t remember |
||
|
5 |
Did you get training on carb counting? |
(i) Yes |
|
(iii) No |
||
|
(iv) I don’t remember |
||
|
6 |
Who mainly contributed to your diabetes management training? |
(i) General Practitioner (GP) |
|
(ii) Nurse |
||
|
(iii) Pharmacist |
||
|
(iv) Diabetologist |
||
|
(v) Other people living with diabetes (PLD) |
||
|
(vi) Web |
||
|
7 |
Number of daily injections |
(i) Three |
|
(ii) Four |
||
|
(iii) More than four |
||
|
(iv) Continuous subcutaneous insulin infusion (CSII) |
||
|
8 |
How satisfactory do you consider periodic diabetes visits? |
(i) Entirely satisfactory |
|
(ii) Barely satisfactory |
||
|
(iii) Unsatisfactory |
||
|
(iv) Totally unsatisfactory |
||
|
9 |
How would you rate the attitude of doctors and nurses? |
(i) Too technical |
|
(ii) Useless |
||
|
(iii) Helpful |
||
|
(iv) Detached and directive |
||
|
(v) Empathetic but helpful |
||
|
(vi) Empathetic but not very helpful |
||
|
10 |
How do you rate the quality of your relationship with your care team, with 10 points being the worst? |
Add a tick on the number on the graph that suits you the best (10 as the worst, 0 as the most satisfying quality) |
|
11 |
What would you like to have improved in your diabetes care organization? (multiple answers are allowed) |
(i) more time allotted to visits |
|
(ii) better communication |
||
|
(iii) less paperwork and bureaucracy |
||
|
(iv) shorter waiting lists |
||
|
(v) more freedom in food choices |
||
|
(vi) lower costs |
||
|
(vii) user-friendly technology |
||
|
(viii) technological advances |
||
|
(ix) other |
Table 1 Questionnaire structure. People living with diabetes answer questions by choosing the one mostly fitting their conditions or way of thinking
The inclusion criteria included a diagnosis of T1DM and a disease duration of one to five years. We excluded subjects who were visually impaired/blind, not independent, needing support from a third person, suffering from other relevant degenerative neoplastic or autoimmune diseases, or illnesses judged by medical personnel to significantly interfere with personal well-being. Table 2 reports the general characteristics of the examined cohort. All subjects signed the written informed consent form, agreeing to participate.
|
M±SD |
Range |
|
|
Age (y) |
36.6 ± 4.4 |
18 - 40 |
|
Sex (M/F) |
74/72 |
- |
|
BMI (kg/m2) |
26.7 ± 3.8 |
22 - 28 |
|
Diabetes Duration (years) |
1.6 ± 4.7 |
5-Jan |
|
HbA1c (%) |
8.2 ± 2.3 |
5.2 – 11.7 |
|
Daily Insulin Dose (IU/day) |
28.7 ± 6.8 |
24 - 39 |
|
Glycaemic Variability (mg/dl) * |
174 ± 219 |
76 – 298 |
Table 2 General characteristics of enrolled subjects. (*) maximum daily interval on the 7-day average
The study was authorized by the Ethics Committee of the Vanvitelli University (Protocol No. 132/2024) as the Research Reference Centre, guarantor and coordinator of all the territorial outpatient facilities of the Nefrocenter Research Network (Diabetes Units: AID Stabia, AID Oplonti, AID Nocera, AID Nola, AID Irpino, Italian Diabetes League-Naples). It was conducted according to the original Declaration of Helsinki guidelines and its subsequent amendments.
Data are presented as means ± SD and percentage. Statistical comparisons were made using paired and unpaired Student's t-tests, with Yates correction, and by nonparametric tests as needed. The lower level of statistical significance was set at p < 0.05.
The characteristics of the enrolled cohort, described in Table 2, 3, show that participants were lean on average, equally distributed between sexes, in poor metabolic control, and with wide glycemic variability. Only 12% had a shallow cultural level, and 12% had a degree. 7% were unemployed, and all the others had an established business. 31% were single, 14% divorced, and the remaining 55% had their family unit. All 146 enrolled subjects completed the questionnaire. Figure 1 describes the care setting in which the T1DM diagnosis was made and communicated for the first time. In 47.5% of the cases, this occurred in the hospital and mainly after an episode of coma. Figure 2 illustrates the results regarding who first communicated the T1DM diagnosis. 12.5% of the subjects did not remember, while most participants did not have a precise memory of the circumstances despite recalling a doctor as the one who did so and, as seen in Figure 3, declared not being able to understand the meaning of that communication clearly.
|
Instruction |
% |
|
primary school |
14 |
|
middle school |
21 |
|
high school |
53 |
|
degree |
12 |
|
Work activity |
% |
|
unemployed |
7 |
|
student |
23 |
|
employee |
24 |
|
worker |
21 |
|
farmer |
10 |
|
teacher |
6.6 |
|
manager |
0.7 |
|
professional |
5 |
|
military |
1.3 |
|
religious |
0.7 |
|
retired |
0.7 |
|
Marital status |
% |
|
single |
31 |
|
married/cohabiting |
55 |
|
divorced |
14 |
Table 3 Socio-economic status
37% of interviewees did not remember having followed any educational training after the diagnosis, and 44% stated they had not followed any educational course (Figure 4,5). Only 15% declared having followed training on carbohydrate counting. In contrast, all the others stated either not having followed any course or not remembering (almost the same as not following it). Regarding the figure that they identify as the one with the most significant weight in the educational role, 35% induced the diabetologist, 30% the nurse, 10% the GP, 10% the pharmacist, and another 10% admitted they learned what to do through the web (Figure 6). These data seem relevant when referring to the injection system used. Indeed, 12.5% used insulin pumps, 12.5% self-injected insulin over four times, 62.5% four times, and 12.5% three times per day (Figure 7).
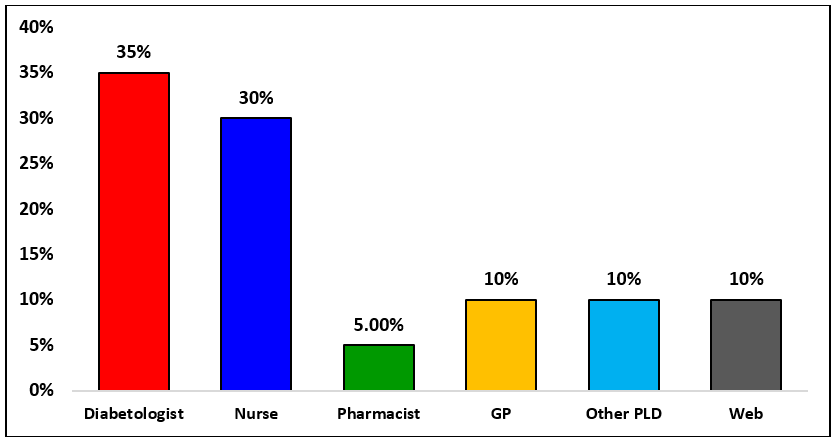
Figure 6 Who mainly contributed to your diabetes management training? GP = General Practitioner; PLD = People Living with Diabetes
Regarding the relationship between PwD and the care team, Figure 8 shows what the subjects thought about the usefulness of follow-up visits. 25% considered them barely satisfactory, 38% entirely satisfactory, 23% unsatisfactory, and 15% totally unsatisfactory. The reasons for these evaluations are reported in Figure 9. The doctor was judged to be often too technical (15%) - as opposed to the nurse less so (6%) -, seconded (25%) and managerial (17%), empathetic and practical (5%), or ineffective despite being empathetic (10%). What stands out is that the nurses' approach was considered very helpful (25%) and, in any case, more so than the doctors' (18%) (Figure 10).
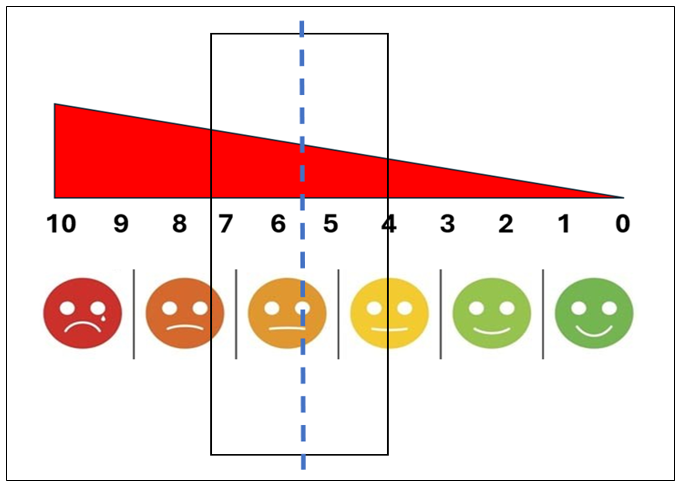
Figure 10 How do you rate the quality of your relationship with your care team, with 10 points being the worst? The dotted line indicates the mean, and the box indicates the SD.
Overall, the effectiveness and helpfulness of the whole care team scored between 4 and 7.3 on a 0-to-10 scale, with 10 being the worst score. When asked to express what they would like differently, PwD revealed specific needs for treating what many of them represented as an individual condition and, therefore, considered "their own" disease. Undoubtedly, they would have liked visits of a longer duration and with an improved method of execution, especially in terms of simpler, more practical language aimed at individual objectives. Above all, they would have liked less bureaucracy and much shorter waiting lists (Table 4). No correlation was found between the participants' opinions and socioeconomic condition or marital status, as all social groups of any marital conditions gave similar answers.
|
Answers |
% |
|
more time allotted to the visits |
80 |
|
better communication |
60 |
|
less paperwork and bureaucracy |
95 |
|
shorter waiting lists |
90 |
|
more freedom in food choices |
96 |
|
lower costs |
25 |
|
user-friendly technology |
44 |
|
technological advances |
33 |
|
other |
24 |
Table 4 What would you like to improve in your diabetes care? (Multiple answers allowed)
These data represent a split of how people with T1DM have perceived their condition for five years since diagnosis, i.e., a period in which the emotions evoked by life changes were still vividly present. Indeed, about half of the participants received their diagnosis in critical conditions, which made it difficult for them to become immediately aware of what was happening. However, their complaints about missing education can help explain the reasons for incorrect behavior and poor metabolic control. The most relevant aspect is the low participants' rating of diabetes visit helpfulness and treatment team performance. The data collected mercilessly stigmatized how, regardless of education, employment, or marital status, investigated people with T1DM considered inadequate time for education, communication skills, and understanding of their individually identified requirements and wishes, asking for a more practical and less directive approach, to be based on simple and understandable language. Indeed, PwD burdened with engaging self-care activities consider excessive bureaucracy and lengthy waiting lists for medical services enormous hurdles which, added up to everyone else's tasks, make life extremely complex. These comments are easily understood when thinking that those on a basal-bolus regimen have to self-inject insulin 1460 times yearly!
Equally mercilessly, it emerges that many HCPs display limitations in their approach to care, especially in terms of training on best injection practices. Recent investigations focused on such an item regarding knowledge, attitude, and behavior of PwD, doctors and nurses since the beginning of insulin therapy throughout the entire disease process in different hospital types.11 In 2023, 19,853 nurses from 82 hospitals in 15 cities in China completed a self-administered questionnaire on those aspects, showing that only 22.3% had good knowledge, 75.9% good attitude and 92.7 % good behavior depending on gender, age, education, work experience, type of ward, diabetes certificates, position held and most recent experience with insulin administration.12 Such results found further confirmation in a subsequent analysis conducted by Chinese researchers on 10,694 PwD, 2643 physicians, and 2816 nurses,13 in that, when reviewing patient glucose logs or meter downloads, clinicians paid more attention to the type and amount of insulin for a specific nutrition intake than to insulin administration modalities is given (i.e., the insulin injection technique).14
Skin lipohypertrophy (LH) due to incorrect injection technique is the leading local complication of insulin therapy. It affects over half of people who are on insulin. It has significant clinical consequences because, when injected into it (mainly because, due to its denervated structure, LH prevents sting pain), the hormone is absorbed irregularly and unpredictably, thus causing wide glycemic variability with high risk of hypoglycemia, inadequate glycemic control and poor quality of life. The above always depends on poor or ineffective therapeutic education.15 Therefore, clinicians should be aware of LH-related items. In 2021, hospital physicians from 13 cities in China completed 499 questionnaires on their daily clinical practice, from which unsatisfactory awareness and knowledge of LH and behavior concerning LH emerged. Such results were independent of working in primary, secondary, or tertiary hospitals), or being senior, attending, or resident physicians, despite seniors performing somewhat better.16 Only 38.7% of doctors could successfully identify all the hazards associated with LH; in any case, doctors from tertiary hospitals were better. The Authors concluded that physicians' understanding of LH was inadequate, especially in primary hospitals. Other research also underlines the need to increase doctors' knowledge of incorrect injection practices and LH, i.e., the most widespread yet underscored form of related complication.17,18
In conclusion, much remains to be done to improve the daily clinical, social, and personal conditions of persons with T1DM. With respect to that, HCPs must become aware that pursuing the goal of euglycemia when treating diabetes involves a whole, complex process, including a series of actions aimed at supporting PwD in improving their interpersonal relationships, understanding their individual needs, and breaking down the barriers raised by old-fashioned, outdated professional attitudes.
Sincere thanks are due to the person who participated in the study
No funding or sponsorship was received for this study or the publication of this article. None of the authors received funding or another type of payment for this paper.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
FS, GG, ES, MC, GC, and SG created and wrote the paper and approved the final text.
Felice Strollo, Giuseppina Guarino, Ersilia Satta, Maria Chiarello, Giuseppe Caccavale, and Sandro Gentile have no financial interests to declare in relation to the present manuscript.
This study was conducted in accordance with good clinical practice standards and following the original Declaration of Helsinki and subsequent amendments. Written informed consent was obtained from all the participants.
The Ethics Committee of Vanvitelli University approved this study (N. Protocol 132/2024).
Data reported in the current study are available from the corresponding author upon reasonable request.
This Open Access article is distributed under the terms of the Creative Commons License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited.

©2024 Strollo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.