Journal of
eISSN: 2374-6947


Research Article Volume 7 Issue 4
1Yale New Haven Health Bridgeport Hospital, Division of Hospital Medicine, USA
2Medical Student, St. George’s University, University Centre Grenada, Grenada
Correspondence: Rajiv M Mallipudi, MD, MHS, Unit Medical Director, Hospitalist, Clinical Instructor, Yale School of Medicine, Yale New Haven Health Bridgeport Hospital, Division of Hospital Medicine, 267 Grant St, Bridgeport, CT 06610, USA, Tel 203-384-3000
Received: November 03, 2020 | Published: November 20, 2020
Citation: Mallipudi RM, Singh A, Shenoy VA, et al. Reducing length of stay for diabetic foot osteomyelitis patients. J Diabetes Metab Disord Control. 2020;7(4):109-114. DOI: 10.15406/jdmdc.2020.07.00210
Admissions for diabetic foot osteomyelitis (DFO) are associated with increased length of stay due to several modifiable barriers and one of which includes setting up intravenous (IV) antibiotics upon discharge. The aim of this study was to reduce the length of stay (LOS) by at least 10% for all DFO patients who underwent surgical amputation and required IV antibiotics upon discharge. Using a quality improvement approach, the patient journey was mapped out using Lean principles and areas of waste were identified. An innovative electronic order was created and implemented to facilitate placement of a PICC (peripherally inserted central catheter) line to be placed immediately after podiatry surgery to reduce the length of time between surgery and PICC line placement. Pre-intervention and post-intervention LOS was compared using Mann-Whitney test to analyze the non-parametric distribution of the data. The post-intervention group had a mean LOS of 7 days (pre-intervention group: 10 days, p-value=0.027), and the length of time between podiatry surgery to placement of the PICC line was a mean of 2 days (pre-intervention: 5.29 days; p-value=0.008). This study used Lean methodology to identify areas of waste, facilitate discharge and subsequently reduce the LOS for DFO surgical patients.
Keywords: length of stay, discharge planning, diabetic foot osteomyelitis, diabetic foot ulcers
DFO, diabetic foot osteomyelitis; DFU, diabetic foot ulcers; IV, intravenous; ED, emergency department; QI, quality improvement; IR, interventional radiology; LOS, length of stay; ALOS, average length of stay; PAD, peripheral arterial disease; CAD, coronary artery disease; CVA, cerebral vascular attacks; PICC, peripherally inserted central catheter; ED, emergency department
Approximately 40-80% of all diabetic foot ulcers (DFU) lead to diabetic foot infections,1–4 20% of these DFUs go on to develop diabetic foot osteomyelitis (DFO).1–5 Patients with DFO often require hospitalization for surgical excisional debridement of infected bone and at times the discharge process is delayed as patients await antibiotic sensitivities for long term intravenous (IV) antibiotics.6 Prior studies have demonstrated a correlation between increased patient length of stay with an increased susceptibility to acquiring hospital related illnesses and iatrogenic complications,7–11 as well as creating bottlenecks in the emergency department (ED) for patients awaiting hospital beds.12–14 Therefore, orchestrating a safe, unified and efficient multidisciplinary discharge protocol for patients has benefits for both patient outcomes and workflow for the healthcare system. Healthcare organizations can use industrial improvement methodologies for process improvement to enhance patient quality and safety, and reduce wasteful steps.15–20 Lean is a change strategy commonly used in healthcare to eliminate wasteful steps and improve workflow to benefit the patient.21–23 Hung et al.,22 showed that successful implementation of Lean requires leaders to consider the contextual factors that surround efforts to implement Lean in a particular setting. Nicosia et al.,19 noted the positive effects of implementing Lean Methodology principles to increase efficiency in the inpatient discharge process by engaging the entire team in the workflow process.19 Wertheimer et al.,24 presented how implementing key steps in the discharge process using Lean methodology were able to significantly reduce patient length of stay and increase patient discharge before noon.24
Based on prior literature, the success of decreasing patient LOS in a process improvement project using Lean management principles relies on multifactorial components which include: engaging key stakeholders in the sustainability of the process, eliminating wasteful steps in the discharge process, and establishing streamlined protocols with clear tasks amongst the healthcare team.7,21 However, none of these studies utilized a process improvement methodology to reduce the LOS for the DFO surgical patient population. Using a quality improvement approach, this study sought to reduce the LOS by at least 10% for all DFO patients who underwent surgical amputation that required IV antibiotics upon discharge by identifying key areas of waste in the management of the DFO surgical patient.
Study design and setting
This was a quantitative pre-intervention and post-intervention study which was conducted at a 501-bedacademic community hospital between August 15, 2019–February 15, 2020. The study was approved by the hospital administration in accordance with the quality assurance policy. This project was considered a quality improvement (QI) project; thus, IRB approval was not deemed necessary. No direct patient identifiers were maintained in the study database. An electronic dashboard was created from the electronic health record EPIC to capture podiatry surgeries conducted during the 6-month period of this study at the hospital. Inclusion criteria included DFO patients who underwent surgical amputation with bone removal that required IV antibiotics upon discharge and required a PICC line to be placed under the care of the hospital medicine attending service. The exclusion criteria included patients without DFO, no podiatric bone surgically removed, no IV antibiotics upon discharge or no PICC line placed. In addition, exclusion criteria extended to include that that had PICC line placed before podiatry surgery amputation, or patients who underwent surgery at an adjacent campus, or taken care of by internal medicine residents. Lastly, this study population excluded patients with a complicated hospital stay who stayed in the intensive care unit stay, expired in the hospital, or who left the hospital against medical advice. Pre-intervention data was collected from August 15, 2019–November 15, 2019, and the post-intervention data was collected from November 16, 2019–February 15, 2020. A total of 26 patients met the inclusion criteria, of which 14 patients were in the pre-intervention group and 12 were in the post intervention group Figure 1.
The research team met with multiple key stakeholders in different departments to identify the steps involved in admitting and discharging a DFO patient that undergoes surgical amputation of the foot. The goal was to identify key areas of waste that could be intervened on. The entire DFO patient journey from admission to surgery to discharge was mapped out using the Lean tool called value stream mapping Figure 2. This value stream mapping began from the moment the patient arrives to the emergency department to when they are discharged from the emergency department or discharged after surgery. Based on the value stream mapping key areas of delay were identified.

Figure 2 A map showing each step involved from admission to surgery to discharge for the DFO patient that gets surgical amputation. The key areas of delay are identified numerically as follows:
The most significant delay for discharging DFO surgical patients occurred when patients were waiting PICC line placement after surgical amputation. Hospitalists waited for the bone biopsy results to return for infectious disease to review and then make a decision regarding IV antibiotics, and subsequently the hospitalist placed an interventional radiology (IR) consult for PICC line placement Figure 2. Following this exercise, the team held a formal presentation with the stakeholders including the Chiefs of the Divisions of Hospital Medicine, Podiatry, Infectious Disease, and Interventional Radiology and consensus was reached to focus the intervention on reducing the time delay for PICC line placement.
Intervention
Working in tandem with the Division Chiefs of these departments, we introduced an innovative electronic order set to provide the podiatry team the ability to immediately place an IR consult for PICC line after bone was removed (Figure 3–Green diamond). In this way, by the time bacterial sensitivities are resulted, the PICC line is already in place and the patient can be discharged immediately on appropriate IV antibiotics Figure 3. The intervention proposed used an innovative electronic order to provide the podiatry team the ability to immediately place an IR consult for PICC line after bone was removed (Green diamond). The electronic order set was disseminated throughout the entire hospital to effectively enhance communication between the podiatry, hospitalist, infectious disease and IR teams. The podiatry residents were coached in how to utilize the electronic order set, and instructed to place the PICC line order after surgery. This was encouraged by podiatry residency leadership. All hospitalists were informed of this process improvement workflow change too. All patients in the post-intervention group received the PICC line order via the electronic order set. Following the implementation of the electronic PICC line intervention, the research team collected weekly data on the post-intervention group through an electronic dashboard tracking all podiatry surgery patients. Each week the researchers would discuss with the resident podiatry team the importance of placing a PICC line order so the IR team could be notified. Compliance and sustainability were maintained through effective leadership education and celebrating results amongst the departments.
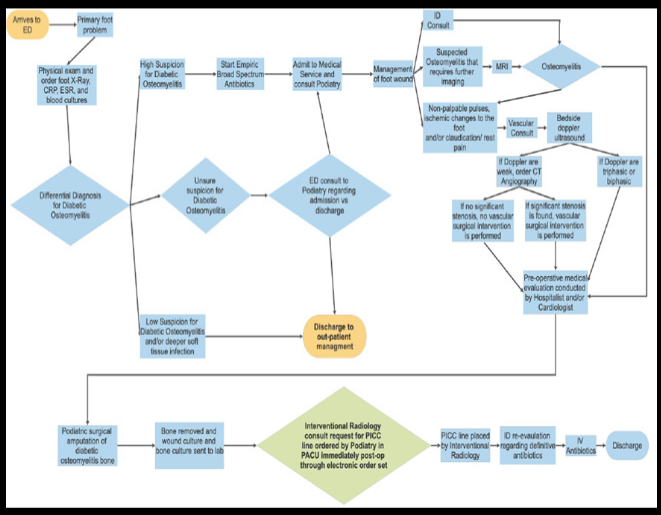
Figure 3 A redesigned map showing the intervention of the electronic order set in order to facilitate faster PICC line placement after podiatry surgical amputation for DFO.
Measurements and statistical analysis
The main outcome measures for the pre-intervention and post-intervention group were total length of stay (LOS) for each DFO patient and total length of time between podiatry surgery and PICC line placement. Data was imported from the electronic dashboard into Microsoft Excel and reviewed based on inclusion and exclusion criteria. Frequency data for the LOS was plotted for the pre-intervention and post-intervention group on a histogram. Similarly, frequency data for the length of time from podiatry surgery to PICC line placement for the pre-intervention and post-intervention group was also plotted on a histogram. Both histograms depicted a non-parametric distribution. The Mann-Whitney U test was selected to compare differences of means between the pre-intervention and post-intervention groups for both the LOS and length of time from podiatry surgery to PICC line placement.IBM® SPSS Statistics software was used to assess if there was a statistically significant impact (p-value<0.05) on the reduction of the overall LOS and if there was a reduction in the time between podiatry surgery and PICC line placement for the pre-intervention and post-intervention groups.
The post-intervention group had a mean LOS of 7 days (pre-intervention: 10 days, p-value=0.027), and the length of time between podiatry surgery to placement of the PICC line was a mean of 2 days (pre-intervention: 5.29 days; p-value=0.008) Figures 4 & 5. Interestingly, during the course of this study from August 15, 2019 to November 15, 2019, the average length of stay (ALOS) for all admitted patients in the hospital was 5.62 days, and from November 16, 2019 to February 15, 2020 the ALOS was 5.55 days. The surgical DFO population assessed in this study in the pre-intervention and post-intervention still had a longer LOS compared to the ALOS, which highlights the importance of the need to find feasible solutions to decrease LOS. Overall, these results show that the primary objective was achieved with an overall 30% reduction in LOS for all DFO patients who underwent surgical amputation and required intravenous antibiotics upon discharge from a mean LOS of 10 days to 7 days.
A key limitation to this study was the small sample size of the DFO population studied (N=26). Population size was limited based on the available DFO podiatry surgery patients within the hospital. The hospital where this study was done at is part of the largest healthcare network in the state and includes five large tertiary care centers with a total capacity of 2,409 beds. Although the population studied was N=26, if the electronic order set were applied for all eligible candidates within the entire healthcare network, the population size may have been N>100. Given this was the first study, this small project was launched to see if it would be successful at one hospital. Future trials can be done expanded throughout the entire healthcare network to see if this electronic order set also can expedite the PICC line placement earlier and in turn reduce LOS within the entire healthcare network. In addition, the intervention was limited to patients under the attending hospitalist service without resident involvement. Typically, resident involvement in a case prolongs the discharge process due to patients staying in the hospital longer to be seen by the attending and to have plans discussed between the resident and attending. Another limitation was that the study involved a specific IR physician team that was motivated and focused on the overall goal to be available 24/7 to help patients get a PICC line as soon as possible.
Future trials could explore if this electronic order would get similar results with other IR teams. An unrecognized limitation, noted after the intervention was complete, was that the electronic dashboard recorded all podiatry surgeries done and did not use the specific inclusion and exclusion criteria. Thus, data had to be individually reviewed and entered to ensure appropriate selection for the pre-intervention and post-intervention group. This can be a source of human error. Furthermore, the day-to-day staffing by different healthcare providers (ex: hospitalist physicians, physician assistants, or nurse practitioners) may affect the management of the patient and prolong the LOS. And lastly, the acuity of the patient illness may also vary the LOS, and this was not able to be measured to account for acute and chronic illness.
The intervention group using the electronic order set had a mean LOS of 7 days (pre-intervention group: 10 days, p-value=0.027), and the length of time between podiatry surgery to placement of the PICC line was a mean of 2 days (pre-intervention: 5.29 days; p-value=0.008). Despite the positive impact of the intervention on LOS, the LOS of DFO patients were still longer than the ALOS of all admitted patients in our hospital. This is the first study to date using Lean methodology to intervene on the LOS of the DFO surgical patient population. The significant take away from this study is that the use of Lean and this electronic order intervention alone had a 30% reduction in the LOS for the surgical DFO patient population. This is a meaningful reduction and demonstrates that these tools can be applied to other patient populations throughout the hospital. It would be interesting to assess the LOS of the DFO surgical patient population based on various subgroup characteristics such as those with peripheral arterial disease (PAD), coronary artery disease (CAD), cerebral vascular attacks (CVA), those patients that underwent revascularization surgery procedures prior to DFO amputation, and sex. Using a larger sample size, the sub-groups can be analyzed to see if there are statistical differences between the subgroups in regards to their LOS. The process of discharging patients is complex requiring multidisciplinary coordination with a diverse group of healthcare providers to provide a safe discharge. Lean methodology and value stream mapping provided a systematic way to identify key areas of waste to reduce LOS. In addition, the success of this intervention emphasized the importance of engaging with key stakeholders when undertaking a process change initiative. Interviews with the healthcare teams and key stakeholders revealed that they appreciated having clearly delineated responsibilities and tasks inpatient care. This reduced the need for superfluous communication throughout the patient admission on what task needed to be done and when. By engaging with the key stakeholders, they felt an investment in the project to reduce the LOS and better enhance the patient experience, and help the overall healthcare system.
Through the use of QI processes and a unique electronic order set there was a reduction in LOS by 30% for all DFO patients who underwent surgical amputation and required intravenous antibiotics upon discharge. Lean methodology identified a key area of waste and introduced an electronic order set to effectively place a PICC line earlier for those that required it. The study emphasizes the importance of engaging key stakeholders in process improvement projects to be successful.
The use of Lean methodology tools and this innovative electronic order set shows promise in reducing the LOS of DFO post-op surgical patients. A future aim of this study should identify additional areas to intervene on based on the value stream mapping for the surgical DFO patient Figure 2, with the goal to decrease the surgical DFO LOS to be similar to that of the ALOS population. Furthermore, future studies should explore the application of this intervention on a wider scale throughout the healthcare system in a larger patient population.
A key area of interests for all hospitals is to decease the ALOS, which is complicated given the diverse patient population. It may be feasible to apply Lean methodology to other patient populations that typically have prolonged LOS (heart failure, pneumonias, ICU patients on ventilators, COVID-19, etc.). Just as it was shown in the DFO surgical patient population, identifying key areas of delay in other complex patient journeys may help reduce the LOS for particular patient populations and in turn decrease the hospital overall ALOS.
The authors acknowledge the assistance of the departments of hospital medicine, podiatry, infectious disease and interventional radiology in the collaboration on this project.
This is an original manuscript and no part of the manuscript has been published before, nor is any part of it under consideration for publication at another journal. There are no conflicts of interest to disclose and this research has not received any funding. All authors contributed substantially to the conception, formulation, drafting, and revision of the submission and take public responsibility for its content.
None.

©2020 Mallipudi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.