Journal of
eISSN: 2374-6947


Research Article Volume 10 Issue 1
School of Public Health, State University of New York, Albany, Rensselaer, NY 12144, USA
Correspondence: Yang Yang, School of Public Health, State University of New York, Albany, Rensselaer, NY 12144, USA
Received: May 08, 2023 | Published: May 29, 2023
Citation: Yang Y, Zurbenko I. Hospital overcrowding caused by covid-19 and chronic kidney disease mortality. J Diabetes Metab Disord Control. 2023;10(1):66-73. DOI: 10.15406/jdmdc.2023.10.00254
The coronavirus disease (COVID-19) pandemic has been the largest public health emergency in recent decades. While there have been many epidemiology studies on this pandemic, less research has been done to examine its indirect impact on mortality. This paper utilizes Kolmogorov-Zurbenko (KZ) filter to examine chronic kidney disease (CKD) mortality trend in Florida hospitals and finds an indirect impact of the pandemic, namely the excess Florida CKD deaths due to pandemic-period hospital over-crowding. The results show that kidney disease patients suffer higher mortality from hospital overcrowding, thus prompting the need to allocate healthcare resource to more vulnerable patients. This paper also proposes a measurement method of hospital overcrowding with KZ filter. The strong correlation between CKD mortality and hospital overcrowding confirms that the level of healthcare has a significant influence on the wellness of CKD patients.
Keywords: time series, kolmogorov-zurbenko filter, hospital overcrowding, chronic kidney disease mortality
Hospitals play a key role in US healthcare system. Hospital’s emergency department (ED) overcrowding threatens public health by compromising patient safety and is a failure to ensure sufficient inpatient capacity to patients with severe illness.1 Hospital overcrowding can be associated with extended inpatient stay, increased healthcare cost per patient2 and increased staff stress,3 and a more deadly consequence is higher inpatient mortality.4,5 The Covid-19 pandemic that emerged in Wuhan,6,7 China in December 2019, presents an unprecedented challenge to US healthcare system.
There have been substantial studies on the origin, diagnosis, treatment and impact of the pandemic.8,9 Various risk factors of Covid-19 have been identified, such as CKD,10 Obesity and overweight,11 and cardiovascular,12 et al. In the meanwhile, Covid-19 is found to have indirect impacts on our society and healthcare system. Health system disruptions, such as insufficient staff availability, insufficient essential medicine, inpatient services/hospital beds not available, and closure of healthcare services etc., have been reported in nearly all responding countries by a WHO survey.13 From the first confirmed US Covid-19 case in January 2020, there have been several major waves. The early Alpha wave and Delta wave are more deadly, but the later Omicron waves have a lower fatality rate.14,15 However, Omicron variant has higher transmissibility caused sharp increase in hospital inpatients. During the peak of the pandemic, the hospital resources were usually exhausted rapidly and patients with various diseases were exposed to higher risk than usual time. Even in highly vaccinated state, patients still suffer from excess deaths.16
While healthcare resource availability has been found to have a direct association with Covid-19 mortality,17 a question is raised: what is the impact of this pandemic on US healthcare system and how well US hospitals are doing when severe disruptions happen? Governments and policy makers should do their best to prevent the scarcity of medical resources during the pandemic and allocate scare medical resources at a fair manner.18 Kidney disease patients are especially vulnerable to hospital overcrowdings. They need higher level of healthcare and more strict healthcare schedule, such as routine dialysis and health condition monitoring plan and usually exhibit an increased propensity to develop other fatal medical condition.19 They need higher level of healthcare and more strict healthcare schedule, such as routine dialysis and health condition monitoring plan. Without proper and timely healthcare servicer, CKD patients can easily develop renal failure and result in death. During the pandemic period, the vulnerability of CKD patients has increased in various aspects.20 They have to face more severe risks and are especially vulnerable to hospital overcrowdings.
KZ filter is low-pass filter and does not reply on parametric assumptions.21–23 With the ability to decompose the original signal into underlying separate components, KZ filter is commonly used in time-series researches,23–26 and are especially effective in handling non-linearity and non-stationarity datasets. This paper uses KZ filter to decomposes Florida mortality trend into long-term component, seasonality component and error term. Florida is the 3rd most populated and the 5th oldest state in the US. In 2020, 3.7% of Florida adults have kidney disease, higher than the national average rate of 2.9%. Kidney disease has become a severe health risk factor to Florida residents. As a result, this study selects Florida CKD mortality data and wants to find out whether hospital overcrowdings during the pandemic are associated with higher CKD mortality.
Data source
Hospital mortality data is based on CDC WONDER online databases. This dataset provides state-level death information on a weekly basis since 2018. The death is broken down into underlying causes, such as Major cardiovascular diseases, Diabetes, Influenza and Pneumonia, CKD, and Covid-19 etc. Another useful variable included in the dataset is the place of deaths. By this factor, this study identifies deaths happened in hospitals and examines their relation with hospital occupancy rates. Mortality is calculated as hospital deaths per 100,000 persons. Hospital occupancy rates are calculated based on Facility-level Hospital Utilization dataset. This dataset provides hospital utilization data on a weekly basis (Friday to Thursday) from 2020 July to 2022 June. All data are retrieved from hospitals’ reports to Department of Health and Human Services (HHS). The hospital population in this dataset includes all hospitals registered with Centers for Medicare & Medicaid Services (CMS) as of June 1, 2020. Non-CMS hospitals that have reported since July 15, 2020 are included as well. However, this dataset does not include psychiatric, rehabilitation, Indian Health Service (IHS) facilities, U.S. Department of Veterans Affairs (VA) facilities, Defense Health Agency (DHA) facilities, and religious non-medical facilities.
Hospital Utilization data provides facility-level information and each data point includes hospital’s name, location, total beds, occupied beds etc. Florida has 207 hospitals and hospital utilization data were aggregated at weekly level. There are 4 hospital occupancy ratios and this paper uses Inpatient Occupancy to measure hospital overcrowding since inpatients bed is the most important service provided in hospitals and inpatient beds occupancy is the most appropriate ratio to reflect the occupancy level of hospitals.
Inpatient Occupancy = Inpatient Beds Used/Total Beds
Covid-19 Inpatient Occupancy = Inpatient Beds Used due to Covid-19/Total Beds
ICU Occupancy = ICU Beds Used/Total ICU Beds
Adults Covid-19 ICU Occupancy = Adults ICU Beds due to Covid-19/Total ICU Beds
This paper also includes potential factors that might be related to death counts, such as healthcare resource and Covid-19 trend. Inpatient beds per capita and ICU beds per capital are good indicators whether the state has sufficient healthcare resource available to patient. Covid-19 trend is calculated as new Covid-19 cases per 1,000 persons. In this research, R is selected as the statistical programming tool since it includes all the necessary mathematical packages.
Multivariate regression
During the pandemic period, various disease mortalities might be impacted. This study is managing to find out whether CKD mortality is impacted by hospital overcrowding, so it conducts a multivariate regression of CKD mortality on hospital occupancy rates. However, hospital overcrowding may have impact on multiple diseases. To find out whether the relation between CKD mortality and hospital overcrowding is unique, this study also selects additional 5 diseases, and conducts multivariate regression of their mortality. These six leading diseases are: CKD, Disease of heart, cerebrovascular disease, influenza and pneumonia, Covid-19 and Chronic liver disease and cirrhosis. In each regression, the dependent variable is leading cause mortality, and the exploratory variables are healthcare resource measures, hospital occupancy measure and Covid-19 trend measure.
The regression formula is defined as:
Time series analysis with KZ filter
This study utilizes KZ filter to decompose the trend of CKD mortality in hospitals. KZ filter has two parameter m, the length of the moving average window and k, the iterations of the desired moving average.21 The formula is defined as:
The log transformed mortality series is composed of long-term trend seasonality component short term and error component The formula is defined as:
In addition to standard KZ filter, this study also uses two extension KZ filters: the KZ Adaptive (KZA) filter and the KZ Fourier Transformation (KZFT) filter. The KZA filter is reconstructed based on the original KZ filter and has the ability to identify the break points allowing for clear interpretation in the presence of a signal suppression due to noise. KZA filter is also used to identify the hospital overcrowding period. The duration between break points of inpatient occupancy trend is defined as overcrowding period. The KZFT filter has three parameters: m, k and f, which is a specific frequency of the data,21,27 and is used to reconstruct periodic signals from non-stationary data with evidence of seasonality.21 This study uses the KZFT filter to identify the seasonality component of CKD mortality.
Sample size and descriptive analysis
From 2018 to 2022 June, Florida has 287,544 deaths in hospitals. Table 1 provides Florida leading 15 deaths in hospitals details. Heart disease and Covid-19 are the top 2 death causes. Covid-19 has the highest standard deviation. CKD is the No. 10 death cause, and has similar weekly mean deaths and standard deviation to chronic liver disease. These results confirm that Covid-19 mortality is volatile due to outbreaks, while chronic disease mortalities are more stable. Covid-19 is a severer health threat to Florida residents. The higher variance in Covid-19 mortality is consistent with people’s assumption since Covid-19 death is highly associated with Covid outbreaks. In the last 2 years, there have been multiple major Covid-19 waves. Covid-19 deaths increase significantly during waves and then drop rapidly after the waves.
|
Total deaths |
weekly mean |
S.D |
|
|
Diseases of heart |
80,044 |
341 |
32 |
|
COVID-19 |
48,430 |
404 |
434.6 |
|
Malignant neoplasms |
43,312 |
184 |
18 |
|
Accidents (unintentional injuries) |
23,776 |
107 |
14.9 |
|
Cerebrovascular diseases |
15,862 |
67 |
10.3 |
|
Chronic lower respiratory diseases |
14,111 |
60 |
10.7 |
|
Diabetes mellitus |
12,062 |
51 |
10.7 |
|
Septicemia |
9,511 |
40 |
8 |
|
Influenza and pneumonia |
9,466 |
40 |
12.1 |
|
Chronic Kidney Disease |
7,787 |
33 |
7.4 |
|
Chronic liver disease and cirrhosis |
6,372 |
27 |
6.9 |
|
Essential hypertension and hypertensive renal disease |
4,039 |
18 |
4.5 |
|
Pneumonitis due to solids and liquids |
3,574 |
16 |
3.8 |
|
Certain conditions originating in the perinatal period |
2,532 |
14 |
2.8 |
|
Assault (homicide) |
1,869 |
13 |
2.9 |
Table 1 Florida Leading Causes of Hospital Deaths
To find out whether there might be latent factors behind mortalities; this study also conducts a factor analysis on these leading 15 causes mortalities and displays the result in Figure 1. Disease mortalities, regardless of acute disease or chronic disease, have loadings in factor 1, but are less impacted by factor 2. In addition, CKD mortality and cerebrovascular diseases mortality are at the far-right side of factor 1 axis. Most of disease mortalities have positive loadings on factor 1. In contrast, assault (homicide) mortality and accidents mortality are highly impacted by factor 2, but have small loadings on factor 1. This finding indicates that disease mortalities and non-disease mortalities have different patterns and might be related to different latent variables.
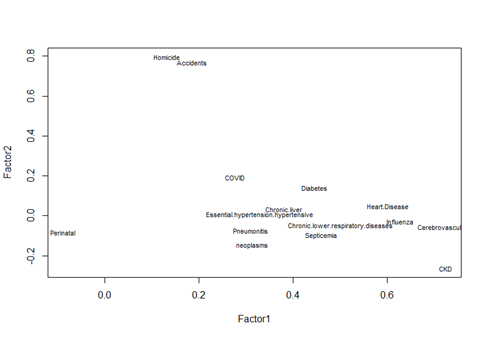
Figure 1 Factor Analysis Plot on leading death causes mortalities, disease mortalities and non-disease mortalities have different patterns.
Table 2 presents a comparison of the baseline demographics of the exploratory variables between Florida and the United States. One notable finding is that Florida has a higher number of available hospital beds per person compared to the national average. This suggests that Florida has more healthcare resources available to its residents. However, the pandemic has presented significant challenges for the healthcare system in Florida. Hospitals in Florida have been more crowded than nationwide hospitals during the pandemic period.
|
Florida |
US |
|||||
|
N |
Mean |
Standard Deviation |
N |
Mean |
Standard Deviation |
|
|
Healthcare Resource |
||||||
|
Inpatient Beds per 1,000 |
101 |
2.72 |
0.34 |
5,151 |
2.48 |
0.56 |
|
ICU Beds per 1,000 |
101 |
0.36 |
0.01 |
5,151 |
0.32 |
0.11 |
|
Hospital Occupancy |
||||||
|
Inpatient Occupancy |
101 |
0.71 |
0.09 |
5,151 |
0.63 |
0.1 |
|
Covid-19 Inpatient Occupancy |
101 |
0.08 |
0.06 |
5,151 |
0.07 |
0.05 |
|
ICU Occupancy |
101 |
0.76 |
0.05 |
5,151 |
0.7 |
0.11 |
|
Adults Covid-19 ICU Occupancy |
101 |
0.12 |
0.09 |
5,151 |
0.12 |
0.09 |
|
Covid-19 Trend |
||||||
|
New Covid-19 Cases per 1,000 |
128 |
2.31 |
3.02 |
6,528 |
2.01 |
2.88 |
Table 2 Baseline demographics of hospital occupancy rates
Multivariate analysis result
The multivariate regression results are shown in table 3. Covid-19 mortality has a strong association with inpatient occupancy. This is consistent with the fact that during Covid-19 outbreaks, there are unprecedented inpatients, and hospitals are under high operation pressure. A noticeable finding is that CKD and Covid-19 are the only two major diseases having significant association with inpatient occupancy. Due to the low volumes of CKD patients, it is unlikely that CKD inpatients caused higher inpatient occupancy. The higher CKD mortality might be a consequence of a more crowded hospital status. In contrast, chronic liver disease mortality has no significant association with hospital occupancy. The newly effective antiretroviral specialty medications reduce chronic liver disease patients’ dependence on hospital care. It indicates that chronic liver disease patients are less likely influenced by the hospital crowding.
|
CKD |
Diseases of heart |
Cerebrovascular diseases |
||||
|
Variables |
Coefficient Estimate |
P Value |
Coefficient Estimate |
P Value |
Coefficient Estimate |
P Value |
|
Healthcare Resource |
||||||
|
Inpatient Beds per 1,000 |
-0.003 |
0.84 |
-0.091 |
0.20 |
-0.01 |
0.67 |
|
ICU Beds per 1,000 |
-0.986 |
<0.001 |
-3.137 |
0.05 |
-0.751 |
0.15 |
|
Hospital Occupancy |
||||||
|
Inpatient Occupancy |
0.290 |
<0.001 |
0.048 |
0.90 |
0.234 |
0.07 |
|
Covid-19 Inpatient Occupancy |
-0.281 |
0.45 |
0.398 |
0.81 |
-0.435 |
0.42 |
|
ICU Occupancy |
0.248 |
0.20 |
1.870 |
<0.05 |
0.222 |
0.44 |
|
Adults Covid-19 ICU Occupancy |
0.055 |
0.79 |
-0.559 |
0.55 |
0.139 |
0.65 |
|
Covid-19 Trend |
0.000 |
|||||
|
New Covid Cases per 1,000 |
0.002 |
0.33 |
0.009 |
0.40 |
0.004 |
0.22 |
|
Influenza and pneumonia |
COVID-19 |
Chronic liver disease and cirrhosis |
||||
|
Variables |
Coefficient Estimate |
P Value |
Coefficient Estimate |
P Value |
Coefficient Estimate |
P Value |
|
Healthcare Resource |
||||||
|
Inpatient Beds per 1,000 |
-0.007 |
0.80 |
-1.666 |
<0.001 |
-0.014 |
0.30 |
|
ICU Beds per 1,000 |
0.221 |
0.74 |
-10.076 |
0.15 |
-0.43 |
0.15 |
|
Hospital Occupancy |
||||||
|
Inpatient Occupancy |
-0.026 |
0.88 |
7.156 |
<0.001 |
0.015 |
0.84 |
|
Covid-19 Inpatient Occupancy |
0.097 |
0.89 |
-68.310 |
<0.001 |
0.214 |
0.50 |
|
ICU Occupancy |
-0.096 |
0.80 |
3.637 |
0.34 |
0.287 |
0.08 |
|
Adults Covid ICU Occupancy |
0.074 |
0.85 |
55.728 |
<0.001 |
-0.103 |
0.55 |
|
Covid-19 Trend |
0.000 |
|||||
|
New Covid-19 Cases per 1,000 |
0.002 |
0.62 |
0.370 |
<0.001 |
-0.002 |
0.37 |
Table 3 Multivariate Regression Result
Figure 2 provide influential analysis results on CKD regression. Cook’s D and Hadi’s show that CKD mortality model is strongly influenced by observations in early 2021 and early 2022. During that periods, Covid-19 outbreaks are also at their peaks and hospitals are under higher pressure. This finding provides further evidence that CKD mortality might be influenced by other factors during Covid-19 peaks.
CKD mortality trend analysis
Figure 3 illustrates the trends of CKD deaths in both hospitals and all places across Florida. The in-hospital CKD death trend is similar to all-place trend. The number of CKD deaths in both settings is higher during the winter and early spring months compared to the summer season. This result is consistent with previous findings that there are a larger number of failing organs in winter and a higher mortality rate for patients with various diseases.20,28,29 Furthermore, the analysis reveals a significant peak in CKD deaths during early 2022, despite the recurring peak in CKD deaths observed every winter. This finding suggests that CKD patients in Florida have faced severe challenges during the last two years and have experienced a higher mortality rate during the pandemic.
With raw CKD deaths, this study calculates CKD mortality rate and conduct a log transformation on the mortality to obtain a more stationary data series. The log-transformed CKD mortality is decomposed into long-term, seasonality and error components by KZ filter and the results are shown in Figure 4. The long-term trend is estimated by where y(t) is the log transformed CKD mortality. During the pandemic period, the long-term component is at a relatively higher level and there is a very significant peak in early 2022. The seasonality component is calculated by . The short-term and error term is calculated by . Florida CKD mortality has a regular annual patter. However, in 2020 summer, there is an additional smaller peak, which might be caused by the outbreak of Covid-19. The error term has a mean of 0 and is distributed evenly in the last 4 years.
The break point is calculated by . The break point shows that Florida CKD mortality had a sharp increase in 2021 winter and then stayed at a high level. This unprecedented breakpoint cannot be explained by the seasonality and indicates the potential impact from hospital overcrowding. This paper then conducts diagnostics analysis on the error term of CKD mortality. QQ plot shows that residuals are normally distributed and the R2 is approximately 91.1%. The Q-Q plot shows that these points have a strong linearity, so it will be safe to conclude that the log transformation improves the normality of the dataset. ACF test on residuals proves the residuals are white noise Figure 5.
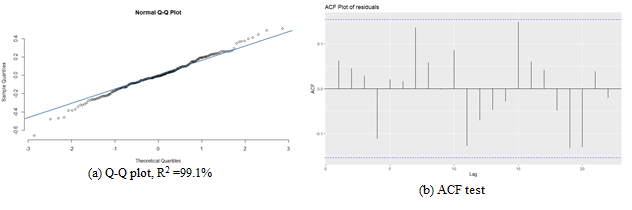
Figure 5 Diagnostic analysis on error term of log- transformed of Florida CKD mortality in hospitals. The residuals are normally disturbed and has no significant seasonality component left. All the lagged residuals are inside the bounds.
Hospital overcrowding’s impact on CKD mortality at hospitals
Florida hospital occupancy data is available after 2020 June. This paper selects inpatient occupancy rate as a measure of hospital overcrowding and plot its log-transformed trend. There are various measurement methods of hospital overcrowding. This study uses an initial measure of the break points of inpatient occupancy rate. The KZ filter is used first to identity the long-term trend where y(t) is the log transformed Florida inpatient occupancy rate. Then the KZA filter is used to reconstruct the break points and the formula is . This method provides visualized cut-of periods of hospital occupancy. Inpatient occupancy plots are displayed in Figure 6. The crowding situation of Florida hospitals had been relieved during 2020 summer and fall, but then it became worse in 2020 winter. The last November 2021 Omicron wave resulted in the worse crowding situation for Florida hospitals.
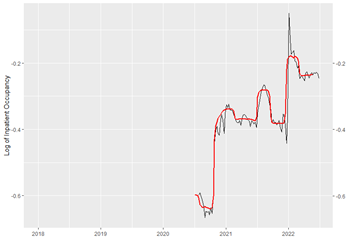
Figure 6 Log-transformed Florida inpatient occupancy trend and break points. Two obvious overcrowding periods can be identified by the KZA filter.
KZ filters have been used to identify periods with excess incidences.25–27 This paper decides to define hospital overcrowding periods as trend lines between inpatient occupancy trend break points. As a result, two hospital overcrowding periods during the pandemic are identified. The first overcrowding period is from 2021 early July to 2021 early September and the second overcrowding period is from 2021 late December to 2022 May, which is the end date of study. This paper runs a t-test to compare the overcrowding inpatient occupancy rate to non-overcrowding inpatient occupancy rate, and finds that the average overcrowding rate is 0.79, which is significantly higher than the non-overcrowding rate of 0.66. This finding further proves that hospital occupancy rates increase significantly during the Covid-19 outbreaks.
This paper then plots CKD mortality and inpatient occupancy rate concurrently in Figure 7. Over the last two years, there is only one breakpoint of CKD mortality and it follows the first 2021 summer hospital overcrowding period (figure 7a). After that, Florida CKD mortality has stayed at high level. This finding suggests that even though Omicron itself is not as lethal as previous variants, its heightened infectivity has resulted in extra pressure on the healthcare system. This impact on healthcare system is extremely dangerous for vulnerable patients, such as those with CKD. Furthermore, CKD mortality peak tens to last longer than hospital overcrowding, indicating that even after hospital occupancy drops to the pre-wave levels, CKD patients continue to experience higher mortality. These findings indicate that hospital overcrowding can result in irreversible long-term harm to the health of kidney disease patients. It is crucial to take steps to alleviate hospital overcrowding and protect the well-being of vulnerable patient populations.
CKD mortality and inpatient occupancy are also impacted by seasonal factors in the real world. Typically, CKD mortality is higher during winter season. In the meanwhile, hospitals also often experience higher pressures by during winter and must maximize their capacity to meet the escalating healthcare demand. Both the seasonality of CKD mortality and inpatient occupancy in the same chart (figure 7b). CKD mortality usually reached its annual peak between December and February. In the meanwhile, inpatient occupancy trend exhibits bi-annual peaks during both winter and summer seasons of each year. This chart demonstrates the significant overlaps between the seasonal trend of both CKD mortality and inpatient occupancy. The seasonal trend of hospital occupancy tends to precede the seasonal trend of CKD mortality and fluctuates more rapidly. These findings provide additional evidences that hospital overcrowding may cause excess CKD deaths, even in ordinary circumstances.
Before and after Covid-19 CKD mortality and comparison to CKD mortality at home
This study shows that there have been significant changes in CKD mortality during hospital overcrowding periods. However, since hospital overcrowding during pandemic is caused by Covid-19 outbreaks, there is concern about whether Covid-19 itself may exert a biological influence on CKD patients, thereby elevating CKD mortality rates. To explore this potential association, this study compares both CKD mortality in hospital and CKD mortality at home before and after Covid-19 outbreak. There has no research on whether hospital overcrowding may cause the increase in CKD mortality at home. This study may provide further insights into the effects of hospital overcrowding on CKD patients. The first Covid-19 cases in Florida were reported on March 1, 2020. In this case, this study defines dates before March 1, 2020 as “Before Covid-19 Period” and dates after March 1, 2020 as “After Covid-19 Period”. The t-test results of CKD mortality rates during these periods are shown in Table 4.
|
Before Covid-19 |
After Covid-19 |
P-value |
|
|
In Hospital |
0.1463 |
0.1605 |
0.001 |
|
At Home |
0.0588 |
0.062 |
0.0971 |
Table 4 Florida CKD Mortality Before and After Covid-19
Based on Table 4, the average of Florida CKD mortality in hospital before Covid is 0.1463 and the rate after Covid-19 is 0.1605. The p-value is 0.0010 and it indicates a significant change in CKD mortality in hospitals before and after Covid-19. In the meanwhile, Florida CKD mortality at home is 0.0588 before Covid-19 and 0.0620 after Covid-19 and the p-value is 0.0971. It indicates that the pandemic has no significant impact on CKD patients at home. These findings are further evidence that the increase in CKD mortality in hospital is caused by the hospital overcrowding, not the Covid-19 virus itself.
This study examines the impact of hospital overcrowding on Florida CKD patients. In the pandemic period, US hospitals have faced a severe challenge caused by Covid-19 waves. Due to the virus’s high transmissibility and severity, hospitals have to admit inpatients dozens of times than usual in a few weeks. The healthcare resources were exhausted in a rapid manner and patients with other diseases suffered collateral damage. This study showed that kidney disease patients were hurt significantly by the hospital overcrowding during the pandemic period. This damage could be long term and last for several week or months after Covid-19 wave. A more optimized and fair allocation of healthcare resource would be extremely helpful to kidney disease patients and could achieve a higher marginal healthcare benefit. Previous research has found some effective methods to alleviate hospital occupancy30; however, new methods need to be found in the face of unprecedented challenge from the pandemic.
As an older state, Florida has a higher proportion of elderly residents who require more medical attention. This has made it even more challenging for Florida to manage the pandemic and maintain adequate healthcare resources for its residents. Therefore, while Florida has access to more healthcare resources, it also faces a more severe challenge in managing the healthcare needs of its population during the pandemic.
None.
The author declares there is no conflict of interest in this job.

©2023 Yang, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.