Journal of
eISSN: 2374-6947


Case Report Volume 11 Issue 1
1Resident physician at the Internal Medicine, Department of Centro Hospitalar de Póvoa de Varzim/Vila do Conde, Portugal
2Attending physician at the Internal Medicine, Department of Centro Hospitalar de Póvoa de Varzim/Vila do Conde, Portuga
3Senior attending physician at the Internal Medicine, Department of Centro Hospitalar de Póvoa de Varzim/Vila do Conde, Portugal
Correspondence: uliana Chen Xu, Resident physician at the Internal Medicine Department of Centro Hospitalar de Póvoa de Varzim/Vila do Conde, Largo da Misericórdia, 4490-421 Póvoa de Varzim, Portugal
Received: February 25, 2024 | Published: March 19, 2024
Citation: Chen-Xu J, Coelho A, Lemos R. Charcot foot: the unknown diagnosis and the unwilling treatment. J Diabetes Metab Disord Control. 2024;11(1):18-20. DOI: 10.15406/jdmdc.2024.11.00271
A 55-year-old Caucasian female presented with one year old oedema of the right foot, flattened, and deformed with no scratch, wound or ulcer. There was no difference in temperature between the feet and it was not painful. The left foot had previously presented two episodes of diabetic ulcers which were treated successfully. The patient had a history of type 2 Diabetes mellitus with need of insulin therapy and associated organ damage. Foot radiography demonstrated and confirmed inactive consolidated Charcot neuroarthropathy. Comfortable custom-made footwear was advised by Orthopedics. No other follow-up was arranged. In Portugal, Charcot foot is not readily recognized, and its management is far from the recommended by the present literature. There are almost no published article about Portuguese Charcot neuroarthropathy cases. Therefore, it is important to showcase Charcot feet in order to make clinicians aware of its existence and their appropriate treatment.
Keywords: charcot joint, diabetes mellitus, diabetic neuropathy, rocker bottom foot
Charcot neuroarthropathy is a progressive degenerative disorder involving the bones, joints and surrounding soft tissues, affecting patients with peripheral neuropathy, specially impaired sensation, of diverse etiologies.1,2 These can be due to spinal cord injury, multiple sclerosis, poliomyelitis, leprosy, syphilis, syringomyelia, heavy metal poisoning, or chronic alcoholism, but the most common cause, nowadays, is the diabetic polyneuropathy.3,4 These patients are usually 50 to 60 years-old and most had diabetes for more than 10 years.1,2,3,5–8 Diabetic Charcot neuroarthropathy affects almost exclusively the feet and usually unilateral.5
Charcot foot is often misdiagnosed due to lack of knowledge and poor understanding of the pathogenesis behind it.2,9,10 It is thought that Charcot foot develops due to recurring micro-trauma to the foot with sensitive deficit (neurotraumatic theory), and sympathetic denervation with peripheral vasodilation and formation of arteriovenous shunting causing the increase of osteoclastic activity (neurovascular theory).1,4,5,11 Their prevalence is increased with aging, obesity, neuropathy, foot trauma or surgery, increased haemoglobin A1c levels, renal failure, iron deficiency anaemia, osteoporosis, and rheumatoid arthritis.2,5 Charcot foot is classified clinical, anatomical and radiologically. Clinically, there is an active and inactive stage, with days to months of progression separating these two3. Active stage presents with increased temperature of >2 °C compared to the other foot, redness, oedema, palpable pulses and sometimes painful.3,7,12 Inactive stage is categorized as a progressively receding inflammation, finally leading to a rocker bottom deformity.3,6 For the anatomical classification, we use the classification proposed by Sanders and Frykberg (Figure 1) while for radiological classification we use the modified Eichenholtz classification (Figure 2).2,6
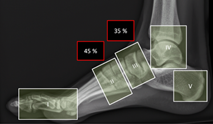
Figure 1 Anatomical classification of Sanders and Frykberg. Zone I: interphalangeal and metatarsophalangeal joints; II: tarsometatarsal joints; III: tarsal joints; IV ankle and subtalar joints; V: calcaneus. From Rosskopf et al.6
Most frequently, the Charcot foot involves tarsometatarsal (Lisfranc) and tarsal joints (Figure 1).3,12–14 When suspecting Charcot foot, besides the anamnesis and the objective description with temperature measurement, the first step is to do weight-bearing radiographs (antero-posterior and lateral images of both feet).4 However, early diagnosis is difficult since it might be normal in the inflammatory stage of the Eichen Holtz classification (Figure 2), therefore, MRI could be done for early diagnosis (bone marrow and soft tissue oedema, joint effusion and microfractures), monitoring disease progression and complications.6,15 As an alternative, CT and PET-CT can be used if MRI is contraindicated.6,15
|
Stage |
|
clinical findings |
radiological findings |
|
0 Inflammatory |
|
Localized warmth, oedema/swelling and erythema |
Almost normal or minimal abnormality |
|
1 Developmental / Fragmentation |
|
Marked localized swelling, warmth, and redness; minor bone deformity, joint instability (ligamentous laxity). |
Focal bone demineralization (osteopenia). Bony debris at articular margins. Fragmentation of subchondral bone. Periarticular fracture. Subluxation, and/or dislocation. |
|
2 Healing / Coalescence |
|
Continued but decreased warmth, oedema and erythema, major bone deformity, bone instability |
Absorption of fine osseous debris. Coalescence/fusion of bone fragments. Callus formation and/or new periosteal bone formation. Sclerosis of bone ends. |
|
3 Remodeling / Consolidation |
|
No warmth, swelling, redness, fixed bone deformity, joint stiffness |
Appearance of a mature fracture callus. Bony remodeling of major fragments. Sclerosis (rounding of bone ends) signify the finality of the permanent deformity |
Figure 2 Radiological classification of modified Eichenholtz. From Wanzou et al.2
Charcot foot is often misdiagnosed as an infection, gout or deep vein thrombosis1,3,5–7 and thus wrongly treated.
First line of treatment of active Charcot foot consists of offloading, with complete immobilization or protected weight-bearing in a total contact casting in order to prevent more trauma and it may take 3 to 18 months long.1,4–8 In the inactive phase, the foot should be accommodated into custom-made insole with therapeutic footwear adjusted to the deformities.1,5,14 Corrective surgery might be considered to improve patient ambulation and quality of life.5 Pharmacological treatments were proposed to aid the first line treatment, such as the use of bisphosphonates and calcitonin to inhibit osteoclastic activity, though clinical evidence has not yet been presented.8 Lastly, long-term surveillance by a specialist should be provided to the patient with Charcot neuroarthropathy.8
A 55-year-old hypertensive, dyslipidemic and diabetic with associated organ damage Caucasian female, presented with one year old oedema of the right foot with deformity. In that period, hemoglobin A1c levels were higher than 8%. The patient did not recall any trauma to the foot before the clinical picture and there was history of two episodes of diabetic ulcers in the left foot. There was no difference in temperature between the two feet, right foot was swollen and flattened when compared to the left foot (Figure 3)

Figure 3 Patient presented with oedema of the right foot, flatfoot with no wound, ulcer or scratch associated. Right foot had the same temperature as compared to left foot.
Investigations
The patient was referred to an orthopedic specialist and plain radiography of the feet was performed, though not weight-bearing images (Figure 4).
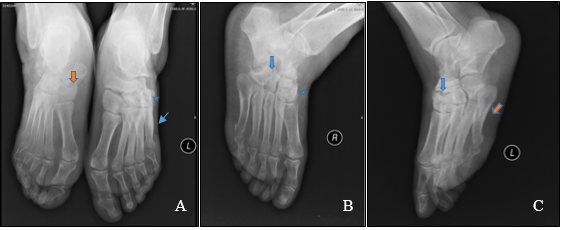
Figure 4 Plain radiography of dorsoplantar images of both feet (A: orange arrow shows degeneration of the right naviculocuneiform joint with collapse; star sign shows unclear image borders of the left cuneiform and cuboid bones; blue arrow shows consolidated fracture of the left 5th metatarsal); lateral image of right foot (B: star sign shows unclear margins of the cuneiform bones; blue arrow shows signs of bone absorption of the cuboid bone borders); and lateral image of left foot (C: blue arrow shows unclear margins of the cuneiform bones; orange arrow shows consolidated fracture of the 5th metatarsal). NOTE: the images are not in a loading position.
Foot radiography already demonstrated bilateral Charcot feet, although on examination, only the right foot showed clinical signs of foot deformity. Bilateral tarsal bones showed signs of osteolysis on radiography and, overall, left foot radiography looked worse when compared to the right foot radiography. No other imaging technique was performed. Literature has documented that 10 to 30% of the patients with Charcot foot have bilateral incidence.1,3,5,7,8 It might be probably 30% or more because these patients usually have difficulty controlling their diabetes and complying with the offloading therapy, consequently overloading the contralateral body, and accelerate foot degeneration.
Treatment
During follow-up of Orthopedics, the patient was advised to use appropriate footwear with custom-made insole, as offloading would not change the outcome already developed. No other therapeutic changes were informed, and no further specialized follow-up was performed.
Outcome and follow-up
The patient did not comply with the indications given by Orthopedics and continued weight-bearing without any modification in her usual footwear nor using custom-made insoles. The patient maintained her diabetes followed-up in Internal Medicine consultation and weight-bearing radiography of the feet was performed for follow-up of progression of Charcot foot, four years later (Figure 5). Clinically, both feet demonstrated flattened plantar surfaces.
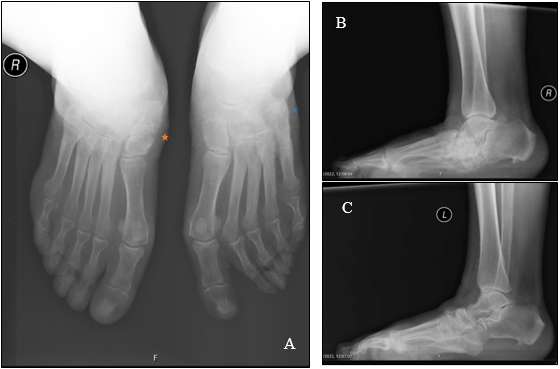
Figure 5 Weight-bearing dorsoplantar feet radiographs (A: orange star shows diffuse bony sclerosis especially seen in the right naviculocuneiform joint with remodeling; blue star shows fusion of the left cuneiform and cuboid bones and consolidated fracture of the 5th metatarsal bone); lateral image of right foot (B: disorganized tarsal and tarsometatarsal joints with unclear bone borders and diffuse remodeling; calcaneal bone absorption and bony fragments); and lateral image of left foot (C: unclear margins of the tarsal bones, diffuse sclerosis and consolidated fracture of the 5th metatarsal).
Charcot neuroarthropathy has various causes, but diabetic etiology is the most common. In Diabetes, it usually affects the foot. It is mostly unilateral but there is a high probability of progressing bilaterally. In an active phase, it is essential to offload the affected foot for as long as necessary to allow reduction of inflammation and delay progression. For an inactive Charcot foot, footwear should be adapted to the patient in order to avoid complications and allow, at least, some comfort and quality of life. However, the main struggle is the early diagnosis of this pathology that slips away by many physicians, allowing progression, that results in consolidated degeneration of the foot with predisposition to recurrent complications. Another difficulty is making the patient compliant to the medical indications, since most of the time they undervalue their diagnosis or they comply to the treatment partial or prematurely until their self-evaluation of recovery.
There is a need to disseminate knowledge on Charcot foot and, in Portugal, there are not many documented cases nor guidelines as to how we should manage these cases, therefore there should be more cases documented in order to allow health professionals to recognize this pathology and provide better care for the patient.
The authors declare not having any conflict of interest related to this paper.
No financial aid was received for this article.
JCX contributed to the conception and design, acquisition of data, analysis, and interpretation of data, drafting and revising the article and giving the final approval of the version to be published. AG and RL contributed to the conception and design, revising the article, and providing the final approval of the version to be published. JCX as guarantor, accepts full responsibility for the work. All authors reviewed the manuscript.

©2024 Chen-Xu, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.