Journal of
eISSN: 2574-9943


Clinical Images Volume 2 Issue 6
Department of Medicine, Southern Central Hospital of High Specialty, Mexico
Correspondence: Marco A Trujillo Juarez, Department of Medicine, Southern Central Hospital of High Specialty, Mexico
Received: June 14, 2018 | Published: November 19, 2018
Citation: Juarez MAT. Well’S syndrome and trombosis. J Dermat Cosmetol. 2018;2(6):109-111. DOI: 10.15406/jdc.2018.02.00098
The well's syndrome or recurrent granulomatous dermatitis is reported the first time by Dr George Wells in United Kingdom of the department of dermatology at St. Thomas Hospital in 1971,1 the report was about four patients who had turret skin with plaques red-violet, slightlypruritic, edematous, recurrent character and disappear in weeks, months without trace. In 1979 Dr Smith added other name to the Well's syndrome and was the cellulitis eosinophilic reported two cases of the above characteristics of well's syndrome and eosinophilia in blood, all cases are unknown origin, the data that made this new entity were this cellulitis with finding histopathology of this rare disease, occur in the dermis forming "flame figures or similar to Fence" of the interstitial infiltrate of eosinophils, which consists in deposition and granules of eosinophil basic protein on the collagen fibers surrounded by histiocytes and some multinucleated cells. This is a characteristic finding is not pathognomonic of eosinophilic cellulitis, Well's syndrome, or recurrent granulomatous cellulitis. The etiological association was to bites, malignitis, and drugs like propionic acid.2
This syndrome is rare disease. Currently has approximately 100 cases reported, it has been described in newborn child,3 but they are presented mainly in adults, being involved sporadic and only a few families has been presented. The presentation of this case with, clinical, histopathological features according to the description and Dr.Well’s, accompanied by presentation so far not reported, the repetition thrombosis in thoracic limbs in a young woman without risk factors to developed venous thrombosis.
Keywords: granulomatous, eosinophilic, histopathological features, collagen fibers, propionic acid
It is of unknown cause, rare, injuries are in epidermis with “flame” or “fence”, less frequently in dermis, subcutaneous tissue and underlying muscle, was observed a greater presence of lymphocytes’ CD3+/CD4+ releasing interleukin 5 (IL-5) and could stimulate the degranulation of eosinophils cause inflammation in the dermis.4 In studies of ultra structure of collagen fibers (Figure 1) are integrated studies immune fluorecence show tanks basic protein of eosinophils. The cause relation-effect have been associated with drugs, like propionic acid, infections, neoplasm like the trigger but there is so far an agent is defined by what may be the overlap of an existing disease.5
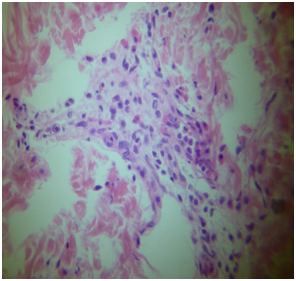
Figure 1 Nodular collections of esosinophil’s with some degranulation on collagen fibers as could be seen in Wells Syndrome.
Clinical picture is characterized by itching or burning sensation in the regions where the lesions are present like popular form, erythematous background and within days evolved to lilaceousplaques, unique or multiple in the economy, being similar sudden appearance and disappearance, indurate lesions reaching, hyperemic or purplish with duration of one week and disappear more slowly with recurrence in the same areas can coexist constitutional symptoms such as fever, joint pain, no scar, the resolution is complete, the treatment, since it is description the use of antihistamines, steroids or treatment of accompanying box. But none drugs is specific yet.
A 36year old woman, originally from the Gulf of Mexico, with a smoking habit of 2-3 cigarettes per day, a history of fibrocystic mastitis of 13years of detection, married without contraceptive ingestion BMI 24.3, Normal blood pressure. The clinical picture started in 1990 with nodular lesions on right thoracic limbs (Figure 2), sudden onset, slightly pruritic, violaceous, and progressing to lower limbs, of different diameters, the "plates" giving per se without leaving any traces, approximately a week later, returning to present this picture a year later, for which he seeks medical help and empirical treatment is given with resolution of the picture 2weeks later, in 1992 he presents venous thrombosis picture evidenced by angiographic study that involves the cephalic vein from the wrist joint, in addition to peripheral eosinophilia of 1302/mm3 preceded the thrombosis picture of skin lesions already described was treated for 6months with anticoagulation resolving the picture satisfactorily 3days later. On this occasion, the picture of dermatosis in lower and upper limbs, has had a more rapid evolution of 48 hours of evolution, as well as pain in right thoracic limbs that has increased progressively in the last 24hours, with oppressive pain to the mobility of thoracic limbs, volume increase and local temperature of the affected limb up to the axillary region.
Laboratory studies show white cytometry, total leukocytes of 5600/mm3 with eosinophilia of 1500/mm3, platelets of 15000/mm3, TP 11.9 ", INR 1.0, TPT 38.2", C–reactive protein 50U, ESR 39mm/hr, Cytometry Red Hb 13.2gr/dl, Erythrocytes 5.3million/ml, VGM 91ft, average concentration of hemoglobin 32, negative VDRL, negative ANA, C3, C4 and CH50, negative anticardiolipin, negative lupus anticoagulant, Factor II and Factor V Leiden without mutations, the thrombophilia study also included serum determination of homocysteine with result of 6.9umol/Protein C by chromogenic method with 87% functionality, Protein S with 65% functionality, alpha-2-antiplasmin 61% activity, antithrombin III 93% functionality, Immunoglobulins: IgE 154UI/ml, (normal reference 10-180IU/ml), corrected calcium 9.2mg/dl, glycemia 99mg/dl, creatinine 1.2mg/dl, magnesium 1.8 mg/dl, negative rheumatoid factor. Imaging studies: right thoracic angiography: evidence of thrombosis of the right humeral vein and finally the report of the histopathological study of skin in lesion area was: "lesions in the form of a flare in the dermis" compatible with eosinophilic cellulitis (Figure 3). With the integration of this diagnosis the medical treatment was with Prednisone 50mgs/day in one shot, and for 6 months I presented recurrence of dermal lesions even under treatment of glucocorticoids with peripheral eosinophils in ranges of 600 to 850 total. He is currently receiving intermittent treatment of isotipendyl acid with a single relapse in 2003 and eosinophils in the range of 150–270 total and ESR of 08–28mm/hour. He has not presented more thrombotic events so far and neither has he presented more pictures of recurrent dermatitis in the last 7years.
The syndrome described initially by Wells1 with the Smith2 who was when he was called eosinophilic cellulitis, later than Spigel and Winkermann6 who are called "Wells syndrome to this unusual dermatosis and peripheral eosinophilia, the etiopathogenic mechanism is unknown until now, reporting associations as a mechanism Probably they are very diverse. The characteristic histopathological lesion called in "Flama" ò in "palisade" accompanied by histiocytes, is not a determining factor per se for the diagnosis since this lesion is possible to find it in other pathologies,2,7 the present case, in this case of Two thrombotic events without alterations in the coagulation tests, the histopathological study of characteristic "palisading" lesion and peripheral eosinophilia have not been reported so far, so that the spectrum of Wells syndrome or recurrent eosinophilic dermatitis is increasingly broad in its presentation, where we now highlight the thrombosis lesion and joins the already known reactions, such as insect bites, drugs, neoplasms, phenomena immune, such as caffeine protein,8–12 vaccines, such as tetanus,13 make us see the wide range of possible trigger events, but not its real etiology, there are more and more reports of this pathology as clinical cases, it is difficult in another way at least for the moment, but we must keep in mind this entity the clinicians before the presentation of dermal lesions, peripheral eosinophilia and histopathological study with lesions suggestive of Wells syndrome.
None.
The author declares that there is no conflict of interest.

©2018 Juarez. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.