Journal of
eISSN: 2574-9943


Case Report Volume 6 Issue 3
1Head and Neck Surgeon, Hospital de Juaçaba, Santa Catarina, Brazil
2Medical student, Federal University of São Paulo, Brazil
3Plastic surgeon, Federal University of São Paulo, Brazil
Correspondence: Roney Gonçalves Fechine Feitosa, Plastic surgeon, Federal University of São Paulo, Brazil, Tel +551155764848
Received: June 30, 2022 | Published: July 13, 2022
Citation: Manfro G, de Oliveira GAF, Feitosa RGF. Use of the deltopectoral flap for reconstruction of a complex cervical defect: case report. J Dermat Cosmetol. 2022;6(3):50-51. DOI: 10.15406/jdc.2022.06.00208
We present a case report of a patient who underwent complex reconstruction of the pharynx and esophagus with microsurgical anterolateral thigh flap and deltopectoral flap for reconstruction of an extensive defect in the cervical region. We will discuss a little about the deltopectoral flap, which was the first choice for the reconstruction of cervical defects in the past, but nowadays it is still an important tool for head and neck defect reconstruction.
The deltopectoral (PD) flap, also called the Bakamjian flap,1 was first described by Aymard in 1917. Aymard described the lifting of a medially based fasciocutaneous flap from the skin of the shoulder which was then intubated and used for nasal reconstruction.2 In 1931, Joseph, using illustrations by Manchot from 1889, justified and published illustrations of DP flaps as vascularized pattern flaps.3,4 The PD flap, however, did not arouse much interest among surgeons at the time, until it was reintroduced by Bakamjian in 1965. The latter reported the use of PD for pharyngoesophageal reconstruction after laryngopharyngectomy1. The PD flap became the most commonly used flap for head and neck reconstruction and enjoyed great popularity in the 1960s, but its popularity gradually faded with the advent of pedicled myocutaneous flaps and microsurgical flaps.
Among its advantages, the DP flap is thin and flexible and has an excellent match of color and texture to the head and neck area. Its anatomy allows for quick and easy harvesting. Its donor area has a minimal functional deficit and can be easily concealed. The flap can be used even in patients with anterior pectoralis major flap if the skin of the PD flap has not been incised during the procurement of the pectoralis major flap. Its pedicle can be divided and returned to minimize donor site morbidity and improve the aesthetic outcomes of the donor and recipient sites. Moreover, it is a fast dissecting flap, with tissue characteristics compatible with the head and neck. It is also an alternative in situations where other flaps have been lost, in cases of extensive cervical emptying and high-dose cervical radiotherapy. The skin graft is usually necessary to cover the donor area, with the exception of small defects in patients with flaccid skin.
As for the disadvantages, in female patients, scarring can also lead to breast asymmetry and nipple distortion. Necrosis of the distal flap is not uncommon if the skin paddle is extended too far into the deltoid region without a delayed procedure. Hirsute skin can be problematic for patients, but epilation (e.g., with a laser) can always be performed later.5 The purpose of this study is to highlight the role of the deltopectoral (PD) flap as a reconstructive option for defects in the head and neck region even today, even in the midst of microsurgery.
A 65-year-old male patient with a history of laryngeal squamous cell carcinoma treated with laryngectomy 10 years ago developed a recurrence of the disease at the base of the tongue with a salivary fistula to the skin. He underwent oncologic surgery that generated a circumferential pharyngeal defect and an anterior neck skin defect as shown in Figure 1. Reconstruction of the pharynx defect was performed using a microsurgical anterolateral thigh fasciocutaneous flap (Figure 2), and the neck skin defect was reconstructed using a deltopectoral flap. Surgery had been performed at Juaçaba Hospital, Santa Catarina, Brazil, by the senior author and team.
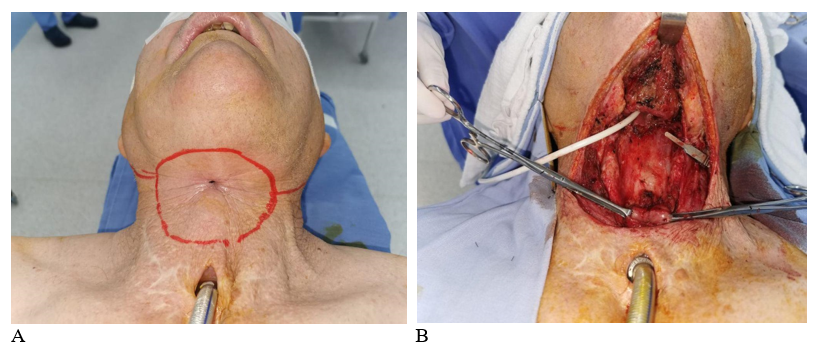
Figure 1 A) Recurrence of laryngeal squamous cell carcinoma at the base of the tongue with exposure of salivary fistula to the neck. B) Defect resulting from oncologic treatment; circumferential pharynx and, anterior neck skin defect.
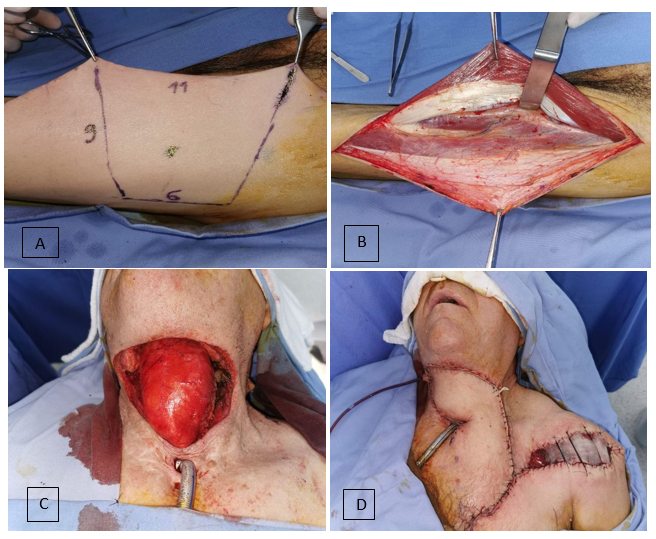
Figure 2 A and B) Planning and collection of anterolateral thigh flap for the pharynx and proximal esophagus reconstruction. C) Pharynx already reconstructed, and one can now notice the size of the anterior cervical skin defect. D) Deltopectoral flap already performed and good coverage of cervical defect. A skin graft was performed to cover the donor area in the left shoulder.
A retrospective chart review was performed to collect information on patient demographics, indications for surgery, defects for reconstruction, surgical techniques, donor site complications, and recipient site complications.
For reconstruction of the circumferential defect of the pharynx and proximal esophagus, the microsurgical anterolateral thigh fasciocutaneous flap was chosen, considering its malleability and possibility of molding in a cylindrical shape. As for the skin defect, the fasciocutaneous flap based on the second and third perforators of the internal mammary artery (deltopectoral flap) was chosen, since the patient had already undergone anterior cervical emptying and no longer had the transverse cervical perforator that supplies the supraclavicular flap.
The skin medial to the DP groove is reliably nourished by the internal perforators, but the skin lateral to the DP groove is usually nourished by the musculocutaneous perforators arising from the deltoid muscles. The extended portion of the DP flap beyond the DP groove is therefore essentially a randomly patterned flap. Where necessary, extension is limited to a 1:1 base-to-length ratio. The deltoid flap was designed by estimating the arc of rotation required to reach the defect and harvested latero-medially.
The insertion depends on the defect. For neck or lower face defects, the skin between the defect and the donor area can be excised, allowing for one-stage reconstruction. Alternatively, the skin bridge can be left intact and have the DP flap placed over the neck skin. The performance of the deltopectoral flap lasted one hour. The latter would require a second division of the pedicle with or without the return of the pedicled component.
The average follow-up time for the patient was 24 months. He underwent surgery after resection of the tumor. None of the flaps were compromised, and the donor regions (thigh and left anterior thoracic region) healed uneventfully. The flap was monitored by clinical and Doppler methods. In the postoperative period, it evolved well, without fistulas or flap ischemia. From the third week of post-op on, the patency of the neopharynx was tested with methylene blue, and there was no leakage of the dye (Figure 3A).
Few flaps have the advantages that the PD flap can offer: a thin, flexible pedicled flap with minimal donor area morbidity and excellent color/texture match to the head and neck area.5
The additional advantage of the PD flap is that it can be quickly lifted and positioned on the posterior wall, requiring minimal de-epithelialization. This also converts a complex circumferential defect into a 'partial' defect and consequently does not contribute significantly to surgical time. Of course, the surgical time to perform the reconstruction may be longer for the novice surgeon as there is an expected learning curve associated with flap removal and placement, valuing and taking into consideration the size of the defect that needs to be covered and the quality and characteristics of the surrounding skin and tissues to allow for a successful reconstruction.6
Over the last decades, several flap variations have been developed, which further increase their versatility, allowing, when appropriate, the combination of a PD and a second flap. In this sense, we highlight, for example, associations of the PD flap with the pectoralis major flap.
The improvement of microsurgical techniques in the last decades allowed obtaining the PD flap as an internal mammary artery perforator (IMAP) flap.7,8 The perforators were localized with manual Doppler preoperatively. The flap is made in the usual manner until the perforators are identified. They are then dissected through the intercostal muscles. The costal cartilages are often removed to increase exposure. This technique can be applied to obtain both pedicled and free IMAP flaps.
Therefore, even with the advent and advancement of microsurgery, the PD flap is very useful in many clinical scenarios. In our opinion, the PD flap is indicated for patients with skin or mucosal defects in the head and neck region and should be considered more often as the first option in need of reconstruction.
The DP flap still has multiple unique advantages (technical simplicity, reliable axial blood supply, large size, thickness, and flexibility, and is an alternative in situations of loss of other flaps, extensive cervical emptying, and high-dose cervical radiotherapy) that few other reconstructive options can offer. Its versatility and reliability guarantee its role as an important reconstructive tool.
None.

©2022 Manfro, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.