Journal of
eISSN: 2574-9943


Short Communication Volume 2 Issue 1
1Vascular Centre, Nuova Villa Claudia, Italy
1Phlebological Surgery Unit, Casa di Cura Villa Fiorita, Italy
2Operative Unit of Angiology, Ferrarotto Hospital, Italy
Correspondence: Palumbo FP, Vascular Surgeon Casa di Cura Villa Fiorita, Via del Ciclope, n-14 -90149, Palermo, Italy
Received: September 08, 2017 | Published: January 22, 2018
Citation: Palumbo FP, Failla G, Serantoni S, et al. Use of laser-speckle contrast analysis in the study of “non healing” leg ulcers-a preliminary studys. J Dermat Cosmetol. 2018;2(1):12-14. DOI: 10.15406/jdc.2018.02.00028
leg ulcer, wound, metalloproteinases, laser-speckle contrast analysis, prostacyclin
LASCA, laser speckle contrast analysis; ROI, region of interest; PU, perfusion unit; SSD, silver sulphadiazine dressing
In the recent years leg ulcers pathophysiological interest have been focused on the role of chronic inflammation that triggers changes in the skin leading to ulcer onset.1 Data emerging from biochemical findings on ulcer exudate, especially those concerning metalloproteinasis levels, suggest a new hypothesis on new activation pathways of chronic inflammation playing an important role on the cell population in the wound tissue.2
Noninvasive imaging approach could provide greater information about a wound than the classical visual inspection during healing phases and help to understand what happen in those “non healing” wounds. In this study Laser-Speckle Contrast Analysis (LASCA) was tested on “non healing” ulcers of different etiology.
When a coherent light (as laser light) hits an object the scattered light will form a random interference pattern consisting in dark and brightness areas or speckle pattern. If the object is stationary the pattern will be clear, but with movement (as blood flow) speckle pattern will changes over time. By CCD camera is possible to capture these changes and depending on the degree of movement the level of blurring.2,3The level of blurring is quantified by the speckle contrast and could be correlate with blood flow and blood perfusion measurement. Usually a helium-neon laser (633 nm) and CCD camera are employed for source and detector, respectively (Perimed AB). Aim of this research is the evaluation of skin circulation in vivo in patients affected of leg ulcers. Oxymethric studies on skin microcirculation based on survey of pO2 and pCO2 data have also shown that their values can be very low in areas of ulcer bottom and in the periwound.4–7 The application of the Laser-speckle Contrast Analysis (LASCA) allows to study in vivo perfusion of the skin, and particularly the area of ulcers and skin "healthy" environment.
15 patients (11 males and 4 females-average age 64,4 +/- 1,7 yy) affected of leg ulcers were enrolled at Operative Unit of Angiology in Ferrarotto Hospital (A.O.U. Vittorio Emanuele) Catania, Italy from march to june 2016 (Table 1).
All patients underwent to clinical, instrumental and serological examination and during admittance period routinary antiplatelet therapy was administred. In venous patients affected of post-thrombotic syndrome antithrombotic therapy was administred (acenocumarol or NAO) plus compressive therapy (high stiffness bandages) and local application of silver sulphadiazine surfactant polymeric dressing (Plurogel®, Plurogen Medline) directly on the wound. Vasculitic patients were assessed by arterial and venous echocolordoppler and serological immunoassays. In post-traumatic ulcer no arterial alterations were present. Therapy was carried out with steroids, analgesics and local advanced dressings in vasculitic ulcers (Figure 1).
In each patient Laser Speckle Contrast Analysis (LASCA) (PeriCam PSI System, Perimed Italy) on three regions of interest (ROI) corresponding to the bottom of the wound, periwound area and peripheral area of skin as healthy skin were studied (Table 2).
Data show increase of perfusion units (PU) in periwound areas in all ulcers. In venous and vasculitic PU were greater respectively 52,3 and 26% than healthy control. Also ischemic ulcers, even poorly, showed the same trend (Table 3).
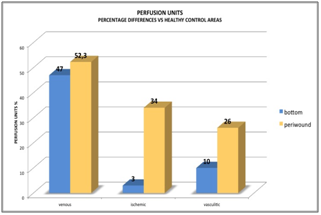
Table 3 Percentage difference of PU versus healthy control in ROI of bottom and periwound in arterial, venous and vasculitic ulcer, respectively.
In this last group iloprost infusion have reduced PU in perilesional areas and increased PU in the bottom of ulcer. No significative changes were present in vasculitic ulcers after iloprost administration (Figure 2). Local administration of SSD (Silver Sulphadiazine Dressing) was followed by reduction of PU both in the bottom and periwound areas (Table 4).
Data analysis at basal time highlight a greater amount of PU in periwound areas (ROI) than in the bottom and check areas.
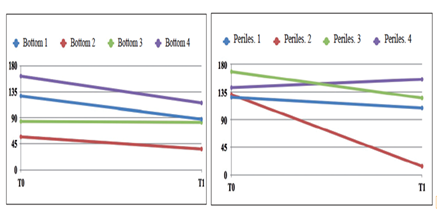
Table 4 PU in bottom and in periwound areas before and after administration of SSD Dressing (Plurogel® Medline).
After iloprost administration or SSD it can be observed a decreased number of PU in periwound and an increase in bottom areas (Figure 3).
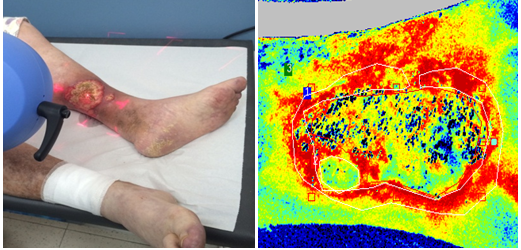
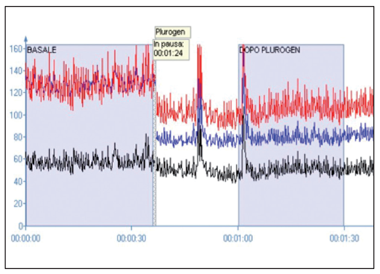
Figure 3 LASCA and oxymethric measurement in arterial ulcer before and after iloprost administration (30 min) (above). After Plurogel®Medline administration with PU and oxymetric values decreased in 30 min.
Despite the limited number of cases examined, the preliminary data review implies a number of considerations:
This could be interpreted as the primary cause of the chronicity of the lesion and the presence of elevated levels of MMPs in the exudate and ulcer tissue confirm the state of chronic inflammation.8,9
Even the administration of the SSD dressing (a transparent gel and which does not alter the refraction of the laser light) capacity is able to determine, especially in the bottom of the ulcer, the PU alterations observed after infusion of iloprost. It is not yet clear whether this information is related to anti-inflammatory and antibacterial properties of the dressing.
Data analysis highlights in all the ulcers the alteration of skin microcirculation especially in periwound areas where a greater number of PU is reduced. After the administration of iloprost or after local application of topical SSD dressing, at the same time as PU numbers in the bottom are increased. Because of Iloprost and SSD antiinflamatory properties it could be argued that in periwound areas a chronic inflammation is present and should be the real cause of delay in tissue repair. The data so far examined are not, of course, significant from a statistical point of view, but open up new diagnostic horizons in the field of wound care. Compared to other methods such as O2 tensiometry, LASCA allows to evaluate in vivo and in real time microcirculation directly in the bottom of ulcer so as to verify the effectiviness of both systemic and local therapy.
The authors are grateful to Dr. Giusto Dalla Favera and Dr. Elsa Lo Jacono to for their support.
The author declares no conflict of interest.

©2018 Palumbo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.