Journal of
eISSN: 2574-9943


Case Report Volume 2 Issue 6
1Centro Universit
1Hospital Universit
Correspondence: Jader Freire Sobral Filho, Avenida Argemiro de Figueiredo, 2200, apto 402, Jardim Oceania, Jo, Tel 5583 9911 7652 7
Received: September 07, 2018 | Published: November 23, 2018
Citation: Souza AC, Filho JFS, Braz AS, et al. Touraine-Solente-Gole syndrome with acne vulgaris successfully treated with isotretinoin. J Dermat Cosmetol. 2018;2(6):118-120. DOI: 10.15406/jdc.2018.02.00100
Touraine-Solente-Gole syndrome or pachydermoperiostosis is a rare genodermatosis, affecting skin, bones and connective tissue, characterized by the triad of pachydermia, periostosis and digital clubbing. The authors report the case of a 26-year-old man presenting the dermato-rheumatic symptoms that characterize the complete form of the syndrome. He also manifested palpebral ptosis and severe acne treated with isotretinoin, in addition to exuberant polyarticular arthritis. Other causes of hypertrophic osteoarthropathy were investigated and not found.
What’s already known about this topic?
What does this study add?
Pachydermoperiostosis (PDP), also known as primary hypertrophic osteoarthropathy or Touraine-Solente-Gole syndrome, is a rare genetic disorder characterized by pachydermia (skin thickening), digital clubbing and periostitis (periosteum proliferation). Its exact incidence is not known, but the estimated prevalence is approximately 0.16%. 1It is more common and severe in men, with a sex ratio of 9: 1.1,2 The condition develops in childhood or, especially, in adolescence, and progresses for 10years or more when it usually stabilizes.2,3 Although an autosomal dominant inheritance with incomplete penetrance and variable expression has been confirmed, both autosomal recessive inheritances have been suggested, these may differ in severity and prevalence of clinical manifestations.4,5 Family history is found in 25% to 38% of patients.4 The syndrome was first described by Friedreich in 1868, who called it 'hyperostosis of the entire skeleton'.6 In 1935, Touraine, Solente et al.7 individualized PDP as the primary form of hypertrophic osteoarthropathy, distinct from the more frequent secondary hypertrophic osteoarthropathy, and is always associated with an underlying cause (e.g., cardiopulmonary diseases and malignancies). The primary form accounts for only 3% to 5% of all cases.5
Male patient, 26years old, white, showing thickening and wrinkling of facial skin associated with enlargement of hands and feet and increased volume of wrists, knees and ankles that started at age 17 and progressed with worsening deterioration, causing difficulty in socialization and injury to walking. He reported on acne breakouts about a year ago and also complained of excessive sweating on the hands and feet. He denied fever, fatigue, recent weight loss and arthralgia. He did not report complaints in the cardiac, respiratory or gastrointestinal systems. Last born of six children of consanguineous parents. The first four died in the neonatal period of causes not known to the parents, and the fifth child, currently 27, is healthy. No history of similar illness in the family.
On examination, he presented coarse facial features, with increased skin thickness and wrinkling of the forehead skin in several folds, deepening of the nasogenian folds and excessive oiliness. Multiple comedones and nodule-cystic lesions on the face, auricles and trunk. Bilaterally thickened eyelids with mechanical ptosis and ectropion. The skin of the scalp showed redundancy, with deep, cerebriform folds in the parietal region - cutis verticis gyrata. There was a significant increase in the volume of the wrists, knees and ankles, associated with edema, heat and limitation of joint movements; hypertrophy of the distal extremities of the upper and lower limbs, digital clubbing, vasomotor alteration and palmoplantar hyperhidrosis. Cardiovascular, respiratory and abdominal systems without abnormalities (Figures 1‒3).

Figure 1 Clinical course. (A) Patient at 20years of age with mild pachydermia and no acne lesions. (B) Patient at 26 years of age with skin folds on forehead, prominent nasolabial fold, blepharoptosis and nodulocystic lesions.
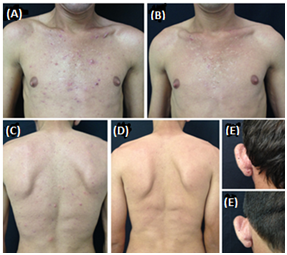
Figure 2 Response to treatment with isotretinoin. (A), (C) & (E) Comedones and nodulocystic lesions on the chest, back and posterior auricular regions, respectively, prior to treatment. (B), (D) & (E) Appearance following use of isotretinoin 20mg/day for four months.
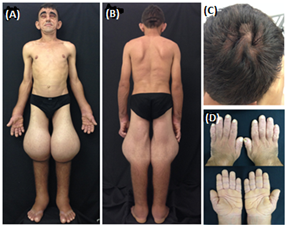
Figure 3 Clinical signs. (A) & (B) Significant increase in the volume of the wrists, knees and ankles; massive widening of the lower limbs. (C) Cutis verticis gyrata. (D) Enlargement and thickening of the hands, with digital clubbing.
In laboratory tests, serum biochemistry, inflammatory tests, and renal and hepatic function tests were normal. Rheumatoid factor, antinuclear factor and VDRL were negative. The growth hormone, parathormone, total testosterone and thyroid profiles were normal. Chest x-ray and skull (pituitary fossa) without changes. Radiographic examinations of the long bones demonstrated diffuse cortical thickening, enlargement of the metaphyseal regions and periosteal neosteogenesis of irregular aspect of the radius and ulna. Magnetic resonance analysis revealed a massive joint effusion in the knees, causing antero-posterior dislocation of the patella. With high gastric endoscopy, presence of hypertrophy of the gastric folds was detected. Ultrasonography of the abdomen with normal appearance. The diagnosis of Touraine-Solente-Gole syndrome was based on history, clinical manifestations, laboratory and radiological findings. Isotretinoin 20mg/day was started for acne treatment. The patient was referred to the Rheumatology, Orthopedics and Ophthalmology services for joint follow-up (Figure 4).
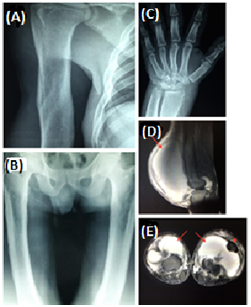
Figure 4 Radiological findings. (A) & (B) Marked thickening of the cortical bones and enlargement of the meta-diaphyseal regions of the long bones. (C) Periosteal osteogenesis in distal regions of the radius and ulna. Sagittal and axial T2-weighted magnetic resonance imaging of the knees, showing voluminous bilateral effusion in the joints (arrows) resulting in localized swelling with a mass effect and acute dislocation of the anterior and lateral patellae (dotted arrow).
PDP predominantly affects connective tissue, skin, and bones. Digital clubbing and periarticular tissue edema of large joints reflect the involvement of connective tissue. The cutaneous involvement comprises two parts: the dermal hypertrophy and the glandular hypertrophy. Dermal hypertrophy is demonstrated as thickening and progressive wrinkling of the skin on the face and scalp (cutis verticis gyrata). Glandular hypertrophy consists of hypertrophy of the sebaceous glands that presents as seborrhea, blepharoptosis and acne, and hypertrophy of the sweat glands as hyperhidrosis. The main bone alteration is irregular new periosteal bone formation in the long bones (periostitis).8
The etiopathogenesis of PDP remains unknown. In family cases, Uppal et al.9 identified mutations in the HPGD gene encoding 15-hydroxyprostaglandin dehydrogenase (15-HPGD), the main prostaglandin E2 (PGE2) degradation enzyme and Zhang et al.10 identified mutations in the SLCO2A1 gene encoding the prostaglandin transporter responsible for PGE 2 uptake. Both studies point to the central role of PGE2 in the pathogenesis of PDP. This prostaglandin has been implicated as mediator of several physiological systems and its production often rises in regions of inflammation.8 PGE2 may mimic the activity of osteoblasts and osteoclasts, and may be responsible for acro-osteolysis and formation of periosteal bone, in addition, it has vasodilator effects that may be responsible for prolonged local vasodilation, resulting in digital clubbing.4 The combination of skin thickening and bone enlargement may result in large enlargement of the extremities - enlargement similar to abutment of the lower limbs1,11 striking physical findings of our patient. An aged appearance, often seen, was observed because of thickened, wavy skin. The most frequently identified sign is digital clubbing,3 which was expressive in the reported patient.
Joint involvement includes joint effusion (41% of cases), often affecting the knees, and polyarthritis, usually symmetrical, present in 20% to 40% of cases.1 The characteristic radiological features are cortical thickening and periostitis of long bones, which is bilateral and symmetrical.1 Periosteal reaction is irregular and often involves the epiphyses, which distinguishes it from the secondary form that usually spares the epiphyses.1,12 Radiographically, this patient presented diffuse cortical thickening of the long bones with enlargement of the meta-diaphyseal, classic findings described in the literature. An important periosteal reaction was not characterized, with only irregular periosteal neosteogenesis in the distal third of the radius and ulna. An exuberant joint effusion in the knees stands out in the case reported, leading to antero-posterior dislocation of the patella.
Clinically, PDP is classified into three forms: complete (pachydermia with periosteal and digital clubbing), incomplete (periosteosis without pachydermia) and frustrated (pachydermia with minimal or absent periosteal involvement).7 The diagnosis should be based on the presence of at least two of the four criteria defined by Borochowitz, which are a history of family transmission, pachydermia, digital clubbing and skeletal manifestations such as pain or radiographic signs of periostitis.1 Our patient had the dermato-rheumatic manifestations of the complete form of Touraine-Solente-Gole syndrome. He also had nodule-cystic acne, blepharoptosis, hyperhidrosis, and gastric hypertrophy. The main associated diseases include anemia, myelofibrosis and gastrointestinal disorders (peptic ulcer, chronic gastritis, gastric carcinoma, Ménétrier's disease and Crohn's disease).8 Although these associations have not been observed in the patient, long-term monitoring and follow-up is necessary.
Differential diagnoses of PDP are secondary hypertrophic osteoarthropathy, acromegaly, thyroid acropachy, syphilitic periostitis and leprosy. Cardiovascular, pleuropulmonary or gastrointestinal conditions, causes of secondary hypertrophic osteoarthropathy, and the increase in growth hormone, prognathism and enlarged sella turcica that are present in acromegaly, as well as pre-tibial exophthalmos and myxedema characteristic of thyroid acropachy have not been observed in this patient.
At the moment, there is no specific treatment for this disease. Non-steroidal anti-inflammatory drugs and corticosteroids are used for symptomatic relief in cases of arthralgia/arthritis.1 Bisphosphonates (pamidronate,1 risedronate4 or zoledronic acid),8 tamoxifen, octreotide and colchicine1 have been reported as effective therapies in refractory cases. In the report by Mattuci-Cerinic et al.13 the treatment of pachydermoperiostosis with colchicine improved joint symptoms, folliculitis and pachydermia. Retinoids are used to improve skin manifestations. Isotretinoin induces apoptosis in human sebaceous glands; as a result, sebaceous gland hyperplasia is inhibited.4 Retinoids also decrease pro-collagen messenger RNA in fibroblasts, improving pachydermia.4 Isotretinoin at the initial dose of 0.5mg/kg/day dramatically improves cutaneous symptoms, including pachydermia and cutis verticis gyrata.12,14
Plastic surgery is indicated for aesthetic reasons. Bilateral blepharoplasty, tarsal wedge resection and excisions of the skin folds may be useful in some cases, but conservative management is sufficient in most patients.1 We started isotretinoin 20mg/day with a significant improvement in acne, we forwarded to ophthalmological services for corrective surgery evaluation. Triamcinolone hexacetonide was injected into the wrist joints to treat arthritis, with partial improvement. The involvement of the knees requires orthopedic surgical intervention due to the damage in the movements. Open surgical drainage and sinovectomy are still underway.
In conclusion, our case illustrates the value of the multidisciplinary approach in conducting PDP, in addition to the beneficial effect of isotretinoin for skin changes, especially nodule-cystic acne.
None.
None.

©2018 Souza, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.