Journal of
eISSN: 2574-9943


Case Report Volume 8 Issue 3
1Medical student at the Federal Fluminense University – Niterói (RJ), Brazil
2MD, Dermatologist, Assistant Professor of Dermatology of Hospital Universitário Regional do Norte do Paraná, State University of Londrina – Paraná, Brazil
Correspondence: Rogério Nabor Kondo, MD, Dermatologist, Assistant Professor of Dermatology of Hospital Universitário Regional do Norte do Paraná, State University of Londrina – Paraná, Brazil, Tel 55 43 99972-5668
Received: August 05, 2024 | Published: August 20, 2024
Citation: Larissa MK, Rogério NK. Rothmund Thomson syndrome with late onset and good preventive control of non-melanoma cancer with acitretin: case report. J Dermat Cosmetol. 2024;8(3):74-75. DOI: 10.15406/jdc.2024.08.00270
Rothmund-Thomson syndrome is a rare autosomal recessive disease that presents with poikiloderma, short stature, alopecia, juvenile cataracts, skeletal abnormalities, and premature skin aging. The manifestation of the disease can begin in the first years of life and people with the syndrome have a greater chance of developing non-melanoma skin cancer. We report a case of late manifestation of the syndrome, treated with acitretin as a preventive measure for skin cancer.
Keywords: rothmund-thomson syndrome, autosomal recessive, acitretin, case report
Rothmund-Thomson Syndrome (RTS) is a rare, autosomal recessive genodermatosis, with unknown prevalence, but estimated to be less than 1: 1000 000. There are few reported cases, with just over 400 cases published in the literature.1 RTS is characterized by poikiloderma (combination of hyperpigmentation, telangiectasia and atrophy), short stature, alopecia, juvenile cataracts, skeletal abnormalities and premature skin aging, starting in the first years of life. People with the syndrome have a greater chance of developing non-melanoma skin cancer (NMSC) due to solar hypersensitivity and the abnormal or reduced capacity to repair altered DNA.1,2 We report a case of RTS with late onset of the syndrome, in which we used acitretin as NMSC chemoprophylaxis.
A patient, white, 56 years old, female, with diffuse alopecia, rarefaction of body hair, nail changes, bone changes, with bilateral cataracts, primary amenorrhea, short stature, attended the outpatient clinic of our university. On examination, alopecia, rarefaction of body hair, brownish macules on the face, trunk and limbs, more prominent in photo-exposed areas, in addition to breast hypotrophy and syndactyly (Figure 1 & Figure 2).
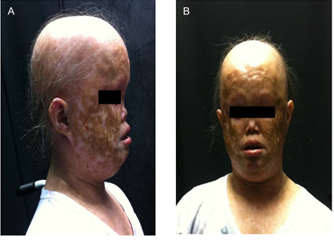
Figure 1 A Lateral view of the patient at 56 years of age showing alopecia, madarosis and hyperchromic spots on the face. (B). Front view.
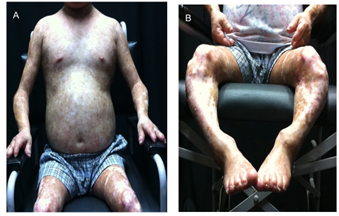
Figure 2 A Brownish spots alternating with hypochromic spots on the trunk, underdeveloped breasts, short stature, hypoplasias on fingers and toes, syntactyly. (B) Detail of anatomical deformities of the legs.
In the photograph files, at the age of 13, he presented brown lesions with telangiectasias on his face (reported from the first months of his life), but without alopecia, without madarosis, without cataracts and without bone changes. At the age of 45, he already had the onset of madarosis, but without alopecia or bone deformities (Figure 3).
Histopathological examination of the forearm skin showed atrophy of the epidermis, rarefaction of the appendages, melanophages in the upper dermis and hydropic degeneration of the basal layer (Figure 4).
RTS was described by Rothmund, a German ophthalmologist, in 1868, who observed children affected by poikiloderma, growth retardation, and juvenile cataracts in Bavarian villages where marriages were consanguineous. In 1936, Thomson, an English dermatologist, reported three patients with similar skin diseases, growth retardation, and skeletal defects, but no cataracts. In 1957, Taylor, an American doctor, determined the eponymous Rothmund-Thomson syndrome to describe patients with these signs and symptoms.3
The diagnosis of RTS is clinical, in which poikiloderma of the face is a major hallmark, associated with findings of cataracts, short stature, alopecia, photosensitivity and findings of changes in long bones. The mutation of the RECQL4 gene or the ANAPC1 gene confirms the diagnosis,4,5 however there may be a possibility that a gene that has not yet been described exists in 30% of cases.6 The anatomopathological examination is nonspecific, but highlights the atrophic dermo-epidermal junction with perivascular lymphocytic infiltrate.
In the present case, as there is no genetic service at the university, the authors paid to carry out the investigation of the RECQL4 gene, which is the most common gene involved (60% of cases), but it was not confirmed. Due to the costs of investigating the other gene, ANAPC1, and the risk of another yet unknown gene involved,6 the authors chose to diagnose RTS based on clinical findings.
The manifestation of the disease may occur early in life.1,2,3 In the present case, only malar erythema occurred early. Cataracts, alopecia, madarosis, deformities of hands and feet, changes in long bones and atrophies occurred in adulthood.
RTS can evolve into NMSC due to failure of keratinocyte DNA repair. Acitretin, a derivative of retinoic acid, can be used as chemoprophylaxis for NMSC, as it has antiproliferative and antiapoptotic action.7 We use acitretin (0.25 mg/kg/day) to treat cancerous fields and, to date, it has not there were emergences of NMSC.
Another problem with RTS is the emergence of osteosarcoma, in which there has been no evidence of neoplasia to date.
RTS is a rare genodermatosis. We hope that, by reporting the case, the article can contribute to the dissemination and understanding of the disease.
Work done by Dermatology Service, Hospital Universitário Regional do Norte do Paraná, State University of Londrina – Paraná, Brazil.
The authors declare no conflict of interest.
None.

©2024 Larissa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.