Journal of
eISSN: 2574-9943


Case Report Volume 4 Issue 2
Department of Dermatology, University Hospital Hassan II, Morocco
Correspondence: Selma Benkirane, Department of Dermatology, University Hospital Hassan II, Morocco, Tel 00212661253442
Received: February 22, 2020 | Published: April 27, 2020
Citation: Benkirane S, Ziani J, Elloudi S, et al. Pregnancy tumor: a case report. J Dermat Cosmetol. 2020;4(2):36-37. DOI: 10.15406/jdc.2020.04.00147
During pregnancy, some skin tumors can occur accidentally due to hormonal changes. Pyogenic granuloma is part of it by acting on the vascular system and deserves special attention in treatment. The diagnosis is based on the clinic, dermoscopy and histology. We report a case.
Keywords: epidermal collar, dermoscopy, botryomycoma, amenorrhea
28-year-old woman, with no pathological history, pregnant with 34 weeks amenorrhea. She presented during the third trimester of pregnancy a budding lesion on the little finger of the right hand painful gradually increasing size and becoming bleeding on contact. Note that the patient does not report the notion of trauma. The clinical examination revealed a well-defined budding tumor of regular contours surrounded by an epidermal collar about 1,5cm in diameter, pediculate-based, purplish red, at the level of the palmar extremity of the little finger of the right hand (Figure 1). The dermoscopy was not very conclusive, revealing vascular lagoons associated with a whitish collar on the periphery (Figure 2).The somatic exam was normal. A pyogenic granuloma was strongly suspected, but a malignant tumor such as an achromic melanoma could not be ruled out. An exeresis was made (Figure 3) and the histological result was compatible with a botryomycoma. No occurrence was noted after two years (Figure 4).

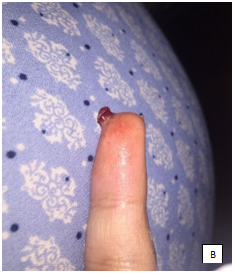
Figure 1 A budding tumor of regular contours surrounded by an epidermal collar (A)about 1,5cm in diameter, pediculate-based; (B) purplish red, at the level of the little finger of the right hand.
Pyogenic granuloma, also called botryomycoma or lobular capillary hemangioma, is a benign tumor of vascular origin of the superficial dermis, but hypodermic forms have also been reported. It can be found all over the skin in tegument and mucous membrane.1 It occurs as a result of chronic irritation, trauma or hormonal change during pregnancy.2 The usual clinical presentation is that of a single budding tumor of small size, brittle, which can bleed on contact, of preferential localization on the upper part of the body or the extremities presenting a great risk of recurrence. In dermoscopy, it typically has dots or globules of pink or light red color separated from each other by thick white lines (collagen septum). A white collar is often present at the periphery.3 The pathology can be found at all ages but is more common in children. Its prevalence varies from 0.2% to 9.6% in pregnant women and frequently develops between the beginning and mid-gestation, between months 2 and 5 of pregnancy related to hormonal changes.4,5 Localization in the gingiva is the most frequently described during pregnancy.
Our patient's tumor appeared during her third trimester at his finger. The high level of sex hormones (estrogen and progesterone) seems to play an important role in the pathogenesis of botriomycoma after the first trimester of pregnancy. Indeed, these hormones stimulate the expression of angiogenic factors in tissues which have an important role in vascular morphogenesis and are found in large quantities in pyogenic granulomas during pregnancy and in small quantities after childbirth.6–9 In our case, the hormonal imbalance due to pregnancy was considered the etiological factor due to the absence of others.
Histology confirms the diagnosis. The treatment is based on surgical excision, which illustrates the case of our patient. Other invasive options such as curettage, electrocoagulation or the application of silver nitrate are possible. The pulsed dye laser and the long pulse Yag laser can be effective on small lesions, with good esthetic results, but require suitable equipment and training.10,7 The topical treatments used so far are Imiquimod, but it is often poorly tolerated [8] and its efficacy is inconsistent, as is Timolol which is a non-cardioselective beta-blocker already recognized for its effectiveness in the treatment of hemangiomas of the child.
Several types of skin tumors develop or change during pregnancy, but fortunately the majority are benign and of no consequence to fetal and maternal health. In our case, achromic melanoma is the main differential diagnosis, if in doubt, surgical excision with histological study is required.
The author declares that there is no conflicts of interests.
None.
None.

©2020 Benkirane, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.