Journal of
eISSN: 2574-9943


Case Report Volume 4 Issue 1
1Department of Dermatology, Clinica Dermatologica Internacional, Spain
2Department of Pathology, Clinica Dermatologica Internacional, Spain
Correspondence: Ramirez-Bellver JL, Department of Dermatology, Clinica Dermatologica Internacional, Spain
Received: December 04, 2019 | Published: February 26, 2020
Citation: Ramirez-Bellver JL, Ruiz-Rodriguez R, Enguita AB. Plasma cell mucositis with exclusive involvement of the perianal region. J Dermat Cosmetol. 2020;4(1):23-24. DOI: 10.15406/jdc.2020.04.00144
We present the case of a woman who has had perianal ulcers for several years. Since no improvement was achieved with topical treatments, a biopsy was performed, showing a dense lymphoplasmocellular infiltrate. After ruling out other differentials, a diagnosis of plasma cell mucositis was made and intralesional betametasone was attempted, with almost complete resolution of the lesions in a few days and no recurrence in one-year follow-up.
Keywords: plasma cell mucositis, idiopatic lymphoplasmocellular mucositis-dermatitis, zoon mucositis
A 67‐year‐old woman presented with a 4‐year history of painful cutaneous lesions on her perianal region, which had been treated with high-potency topical corticosteroids, antibiotics, calcineurine inhibitors and antifungals without improvement. She referred slow but progressive growth of the ulcers, with no periods of remission. She denied gastrointestinal symptoms, fever or weight loss. She also denied manipulation of the area or application of irritating products. Her personal and family history were unremarkable apart from hypothyroidism treated with levothyroxine.
Physical examination revealed 2cm, well defined erosions with a slightly raised, erythematous border, with no exudation, symmetrcal, on the lower region of her intergluteal fold (Figure 1a). On the upper aspect of this fold a smaller ulcer could be observed (Figure 1b). Perilesional skin showed a shiny, whitish discoloration. Routine laboratory tests including quantiferon test, C‐reactive protein, erythrocyte sedimentation rate, serologies for lues, hepatitis B and C and human immunodeficiency virus, and chest X-ray were normal. Biopsies from both lesions were taken.
Plasma-cell mucositis was first described by Zoon1in 1952, for which has also received the name of Zoon mucositis1. This article described lesions on the penis and, since then, cases affecting the vulva, glans, oral mucosa, conjunctiva and vagina have been reported.2,3 In 2014 Mitkov et al.,2 reported the first case of plasmocellular mucositis affecting perianal region. Plasma-cell mucositis is more common in postmenopausic women and in males on the fifth and sixth decade of life. These lesions have received many names, some of them making reference to the anatomic location and others to the clinical aspect. To avoid confusion some authors have proposed the term “idiopathic lymphopasmocellular mucositis-dermatitis” to include this type of affection.4
Lesions consist of erythematous plaques, sometimes ulcered or eroded, with well-demarcated borders and frequently involving genital region (vulva, glans), and that can be asymptomatic or produce itching, pain or bleeding. Etiology is unknown, although cases secondary to trauma and autoimmune diseases have been reported.5 Although considered a benign condition, some authors think that, when affecting the glans, it could be considered as a premalignant condition, due to the maintained, chronic inflammation.6 Histopathology examination reveals a non-neoplasic, dense, rich in plasma cells infiltrate with epidermal atrophy, espongiosis and dilated capillaries. Differential diagnosis includes extra mammary Paget´s disease, erosive lichen planus, squamous cell carcinoma, cutaneous tuberculosis and sexually transmitted diseases. In our case, inmunohistochemistry stains (CD3, kappa and lambda chains, IgG4, anti-treponema antibody) confirmed the non-neoplasic nature of the cells and the absence of spirochaete. IgG4 stained positive for less than 1% of the cells, ruling out the possibility of an IgG4-related disease.
There is no standard treatment, and different responses to both topical and intralesional corticosteroids, topical antibiotics, tacrolimus and imiquimod have been reported.2 Since our patient had already used several topical treatments without improvement, we decided to infiltrate betametasone achieving a fast healing of the lesions with no recurrence after one year follow-up (Figure 3a&3b).
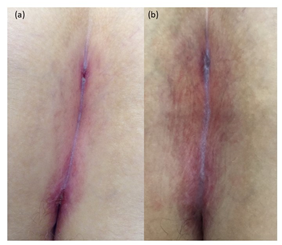
Figure 3 (a) Evolution of the lesions five days after one infiltration with betametasone. (b) one year later
We consider this case of interest for dermatologists, since differential diagnosis of perianal plaques is wide, and only one case of this entity with exclusive affection of the perianal region had been reported before; besides, we would like to highlight the fast and sustained response with intralesional corticosteroids, suggesting this treatment if topical therapy fails.
The author declare that there is no conflicts of interests.
None.
None.

©2020 Ramirez-Bellver, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.