Journal of
eISSN: 2574-9943


Mini Review Volume 2 Issue 4
Department of Dermatology, Universidad Militar Nueva Granada Bogota, Colombia
Correspondence: Claudia Marcela Arenas Soto, Department of Dermatology, Military Central Hospital, Universidad Militar Nueva Granada Bogota, Colombia,
Received: May 17, 2018 | Published: August 23, 2018
Citation: Soto CMA. Microneedles: a therapeutic alternative in melasma. J Dermat Cosmetol. 2018;2(4):207-210 DOI: 10.15406/jdc.2018.02.00079
Background: Melasma is an acquired hypermelanosis of the skin, which compromises the photo-exposed areas of the face. It mainly affects women and the darker photo types (Photo types of Fitzpatrick III-V), causes a great impact on the quality of life of patients who suffer from it, being of concern the therapeutic options available. Micro needles are a novel adjuvant therapeutic modality, their procedure is simple, well tolerated and with cosmetic benefits.
Objective: To conduct a review of medical literature related to micro needles for the treatment of melasma
Method: A literature search was performed using the PubMed, Medline and Embase databases. Additionally, the bibliography of relevant articles was reviewed.
Keywords: melanosis, pigmentation, microneedles, collagen
Melasma is a dysfunction of melanogenesis, which produces symmetrical hyperpigmented macules in the skin's exposed areas, prevalence has been estimated in 1% of the general population and is higher in at-risk populations, its pathogenesis is not clear, but have described some triggers such as ultraviolet rays (UVR), pregnancy, sex hormones, inflammatory skin processes, the use of cosmetics, steroids and photosensitizing drugs, family history is also considered an important risk factor.1 These factors trigger different signaling pathways such as those dependent on the melanocyte stimulating hormone that induces cyclic adenosine monophosphate (MSH/cAMP), also the tyrosine kinase receptor (KIT) and the Wnt transduction pathway, which regulate positive tyrosinase and transcription factor associated with microphthalmia (MITF), which results in the stimulation of melanogenesis and the development of melasma.2
The most usual presentation is located in areas of the forehead, nose and upper lip, respecting the areas that are not exposed to the sun. Histologically, it may show greater epidermal or dermal pigmentation, increased melanocytes, increased melanosomes, solar elastosis, and occasionally perivascular lymphohistiocytic infiltrates.3 The treatment of melasma has become a great challenge that seeks to improve the quality of life of patients who suffer from it; within the therapeutic alternatives arises the microneedle technique, it is a minimally invasive, safe, well tolerated and effective procedure.
The main concept dates from 23years ago with Orentreich and Orentreich who described the management of scars and wrinkles with intradermal needles.4 Later in 1997 Camirand and Doucet described a technique with tattoo guns to improve the appearance of postsurgical scars by releasing tension.5 The first micro needle device was developed in 2000 for rejuvenation and in 2003 Fernandes developed a cylindrical device with multiple needles.6
The normal human epidermis has a transepithelial potential (PET) that varies in different parts of the body (10-60mV). In human skin, the transepithelial potential (PET) is measurable and is established mainly after the asymmetric distribution of sodium ions (Na+) in the lower and upper sections of the epidermis. In the normal human epidermis, the measured values of the transepithelial potential are between 10 and 60mV and vary according to the anatomical location. The role of PET in the normal epidermis has not yet been identified; but after a skin injury, disruption of PET induces an endogenous continuous electric current field (100-200mV/mm) directed towards the center of the wound. This endogenous electric field could be involved in the process of wound healing by attracting cells, which would facilitate re-epithelialization. Increasing and decreasing TEP values correlate with changes in the expression of the potassium sodium pump (Na+/K+ ATPase). The distribution of Na+/K+ ATPase pumps also varies according to epidermal differentiation.7
The micro needle technique or also called collagen-inducing therapy produces a controlled lesion of the skin, these micro-lesions trigger a cascade of healing that starts generating electrical impulses, which are caused by the modification of the transepithelial action potential. The micro needles when penetrating the stratum corneum generate a short circuit of the endogenous electric fields, this activates the Na+/K+ pump seeking to reestablish the inter and intracellular electrical potential caused by the injury; subsequently the cells that surround the channels produced by the needles, detect these repeated penetration stimuli, creating a polarized electromagnetic field, which stimulates the DNA to generate gene expression of proteins from the surrounding cells, with consequent migration of epithelial cells, endothelial cells and releases growth factors such as: platelet-derived growth factor (PGF), transforming growth factor alpha and beta (TGF-α and TGF-β), connective tissue activating protein, connective tissue growth factor and growth of fibroblasts (FGF) (Figure 1). The migration, proliferation and fixation of fibroblasts to the intercellular matrix initiate neocolagenesis and neovascularization, this matrix arrangement allows the deposition of type III collagen and eventually its replacement by type I collagen.7‒10
The most frequent adverse effects of the technique consist of edema, erythema, and solar sensitivity. In a lesser proportion, pain may occur during the procedure, bruising and irritation.12 Few cases of post inflammatory hyper pigmentation have been reported.13,14 The formation of scars has been related to the length of the needles on surfaces in contact with bony prominences.15 No study has reported cases of bacterial super infection, the use of sterile elements and disinfection prior to the procedure is sufficient to avoid it. Some studies have reported infections with herpes simplex virus, which were successfully treated with acyclovir.16,17 (Figure 1) (Figure 2) (Table 1)
Microneedle devices |
Rollers manuales |
Electrical devices with micro needles |
Definition |
Manual device with cylindrical roller with 24 circular dies. Each matrix is equipped with 8 steel micro needles, in total 192 needles (Fig2A). |
Automated microneedle device similar to a ballpoint pen. Use disposable needles and guides; adjust according to the length of the needle (Fig2B). |
Types |
-Basic C8 with a needle length of 0.13 mm, used to enhance the penetration of topical agents. |
Dermapen: The tip contains 9-12 needles arranged in rows. Presents rechargeable battery that operates with 2 modes (high speed 700 cycles / min and low speed 412 cycles / min). |
Advantage |
C8, C8-HE and Beauty Mouse cosmetic use, per patient. |
Ability to adjust speed and penetration depth. |
Disadvantages |
Non-disposable needles |
|
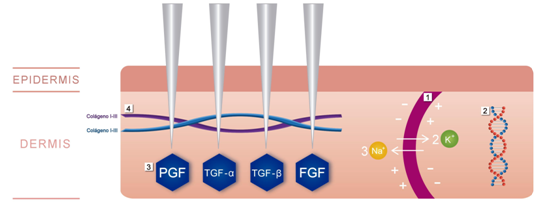
Figure 1 Mechanism of action of the microneedles.
The micro needles began to be used for the treatment of acne scars and it was observed that in patients with concomitant melasma, there was an improvement in the decrease of the pigment in the skin.18,19 In this way, it was begun to be explored as a means of transdermal drug administration in a population with Fitzpatrick III-IV-V phototype, for the treatment of hyper pigmentation disorders.20 The long-term improvement of recalcitrant melasma after micro needle treatment has been reported in case series studies, however, the exact mechanism that promotes skin clearance is unknown.18,19
In a small study conducted in patients from the northeast of Brazil by Lima and colleagues, after the performance of 2sessions with micro needles subjective improvement of the skin smoothness and greater luminosity in patients with recalcitrant melasma was observed. A decrease of 70% in the MASI, 13% increase in luminosity and 55% decrease in the melasma quality of life scale was evidenced. In the histological findings, it was considered that micro needle therapy promotes the proliferation of fibroblasts and superior dermal neocogenesis, decreases the contact of the melanocytes with melanogenic stimuli and improves the protection against ultraviolet radiation due to epidermal thickening.18
Lima et al reported effectiveness of micro needle treatment in 22cases of patients with recalcitrant melasma, followed 2days after the application of depigmentation therapy and sun protection, with maintenance of clearance at 2 and 11months of follow-up. The author considers that the trauma caused should be mild and the use of depigmenting and sunscreen should be mandatory.19 Budamakunkla and colleagues observed better results in 60patients with moderate to severe melasma treated with micro needles plus the application of topical tranexamic acid compared with microinjections.20,21,8 Fabbrocini et al. Demonstrated in a pilot study of 20patients diagnosed with melasma that the combination therapy of micro needles with topical depigmenting agents is more effective than monotherapy with topical depigmenting agents.8,20,21,
The inducer therapy of collagen with micro needles in hyper pigmentation processes constitutes a simple, economic, well tolerated, effective, novel adjuvant therapy, with long-term cosmetic benefits and few adverse effects. It is a procedure that stands out for the epidermal preservation, in addition to stimulating the production of collagen and elastin at the dermal level, which contributes to the decrease of the visible pigment. Thanks to the formation of micro channels can be used in conjunction with topical depigmenting improving its absorption and effectiveness.
None.
Author declares that there is no conflict of interest.

©2018 Soto. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.