Journal of
eISSN: 2574-9943


Case Report Volume 9 Issue 3
Lusíada University Center, Santos, São Paulo, Brazil
Correspondence: Hudson Dutra Rezende, Lusíada University Center, Santos, São Paulo, Brazil, Tel +55 11 9 88987290
Received: July 04, 2025 | Published: July 22, 2025
Citation: Rezende HD, Bilia BM, Raimundo APA, et al. Meyerson phenomenon: A marker of benignity or a diagnostic trap? J Dermat Cosmetol. 2025;9(3):71-72. DOI: 10.15406/jdc.2025.09.00294
Meyerson phenomenon is a rare observation in clinical practice. It was first described by Meyerson in 1971 featuring a peculiar pattern of eczematous halo dermatitis surrounding preexisting melanocytic nevus. Although benign melanocytic nevi are most likely to be associated with the Meyerson phenomenon, cutaneous melanoma has also been diagnosed in such context, calling attention to the need of questioning the so far harmless nature of the phenomenon. This paper offers new insights and recommendations on the diagnosis and management of the Meyerson phenomenon based on a case report.
Keywords: meyerson phenomenon, melanoma, dermoscopy
Meyerson phenomenon was first described by Meyerson in 1971 featuring a peculiar pattern of eczematous halo dermatitis surrounding preexisting melanocytic nevus.1,2 Up to now, the number of publications on the Meyerson phenomenon does not exceed one hundred reports in the literature, and no known epidemiological statistics are currently available, making it an unusual and often unfamiliar diagnosis for most dermatologists.1 Since the Meyerson phenomenon can be mistaken for malignant melanoma and Sutton nevus, also known as halo nevus, one must remain attentive in order to get to the right diagnosis.1
A 37-year-old woman presented with a 2-month history of pruritus on a previously existing pigmented lesion located on the right forearm. The patient denied local trauma, recent ultraviolet exposure, and was not taking any medication. On physical examination, a solitary brown papule was seen surrounded by a symmetrical halo of sharp eczema (Figure 1A). Dermoscopy showed a central pigmented lesion bordered by vivid erythema and partially covered by flakes and crusts (Figure 1B).
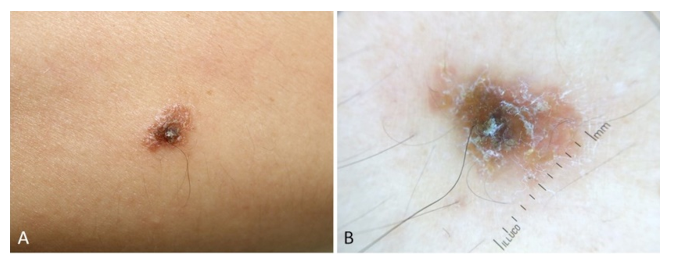
Figure 1 Meyerson phenomenon. A. Clinical presentation at first visit, showing an eczematous halo surrounding a melanocytic nevus. B. Dermoscopic view demonstrating scales around the central mole over a background of erythema.
After evaluating the patient, the Meyerson phenomenon was considered, and the lesion was excised for histopathological analysis, confirming the diagnosis (Figure 1C). The patient is currently under clinical follow-up and has not presented any further symptoms to date.
Since its original description by Meyerson in 1971, the Meyerson phenomenon has frequently been mentioned in the literature.1,3 Due to its rare occurrence,1 it is reasonable to think that many Dermatologists are not acquainted with the entity and are prone to overlook the diagnosis.
Peripheral skin changes adjacent to moles are not exclusive of the Meyerson phenomenon. The appearance of achromic halo surrounding melanocytic nevi is relatively common among children in whom Vitiligo may develop.4 In adults, the abrupt occurrence of a Sutton's Nevus is of great concern regarding the presence of a possible not yet detected melanoma, either of the skin or of the retina and central nervous system.5 For such patients, melanoma must be ruled out and performing an excisional biopsy of the lesion depends on the presence of atypical dermoscopic features.5
Similarly, in 2011 Rodins et al.,2 described a case of an early Clark level 1 melanoma arising within a severely dysplastic compound melanocytic nevus which was surrounded by an eczematous halo, adding yet another entity that may display Meyerson phenomenon.2 Of note, Meyerson phenomenon has been observed concurrently with separate halo nevi and have also been observed to evolve into halo nevi.2
Signs of regression and/or depigmentation of the central lesion are not expected for Meyerson phenomenon, as originally described, but the publication of a series of five children who all had some degree of depigmentation after resolution of eczema calls the attention for real exceptions when evaluating such lesions based on dermoscopic grounds.2
Even though the vast majority of Meyerson phenomena are related to benign skin lesions,2 the search for atypical signs by dermoscopy may be difficult, especially by unexperienced eyes, due to the presence of perilesional erythema, flaking and even central crusting. In this context, it is also important to consider the psychological impact of such presentations. The sudden change in appearance of a long-standing pigmented lesion, especially when accompanied by inflammation or crusting, can generate considerable anxiety in patients, often raising fears of malignancy. Early medical evaluation and appropriate counselling are essential not only to guide clinical management but also to provide reassurance and reduce emotional distress.
The authors of this paper believe that, for cases of Meyerson phenomenon where dermoscopy is doubtful and despite the low probability of associated melanoma, an excisional skin biopsy should not be postponed so that a malignant lesion can be promptly ruled out.
None.
The authors declare that there is no conflict of interest.
None.

©2025 Rezende, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.