Journal of
eISSN: 2574-9943


Research Article Volume 7 Issue 2
1Serviço de Dermatologia, Universidade de Mogi das Cruzes, Mogi das Cruzes, São Paulo, Brasil
2Serviço de Dermatologia, Universidade do Estado do Rio de Janeiro, Rio de Janeiro, Brasil
3Serviço de Dermatologia, Faculdade de medicina do ABC, Santo André, São Paulo, Brasil
Correspondence: Luciana Gasques, Universidade de Mogi das Cruzes. Av. São Sebastião 3125, sala 501, 78045-000 Cuiabá – MT, Brazil, Tel +55-65-98150-3366
Received: April 07, 2023 | Published: April 24, 2023
Citation: Gasques L, Okita A, Giraldelli G, et al. Management of striae alba with Infusion of drugs using MMP technique. J Dermat Cosmetol. 2023;7(2):41-44 DOI: 10.15406/jdc.2023.07.00231
Striae distensae (SD) better known as stretch marks, are a common disfiguring skin disorder, visible as linear scars which develop in areas of dermal damage as a result of excessive stretching of the skin. Despite being a benign lesion, it causes great psychological impacts for patients.
We report a series of cases with 10 female patients, aged 19-45 years, with striae alba, located on the thighs, buttocks, breasts, abdomen, legs and arms, treated with 3 monthly sessions of Percutaneous Medicated Microinfusion (MMP®) using a sterile product composed of elastin, chondroitin, ascorbic acid and hyaluronic acid. After treatment, the degree of patient satisfaction was assessed by applying a visual analogue scale (VAS), graded from zero to ten points. In addition, through the photographic record, we evaluated the density of stretch marks, size, thickness, brightness and depth, comparing the before and after photos 1 month after the end of the three sessions. The patients classified the responses between moderate and good at the end of the treatment.
Keywords: striae distensae, percutaneous medicated microinfusion, drug delivery, scars
SD, striae distensae; MMP, percutaneous medicated Microinfusion; VAS, visual analogue scale
Stretch marks are visible linear scars, which may be erythematous-violet (striae rubra) or hypochromic and atrophic (striae alba), depending on the evolutionary stage. These lesions develop in areas where there is dermal damage to collagen and elastin fibers as a result of overstretching the skin. The most commonly affected sites are: breasts, abdomen, inner thighs, buttocks and knees. The origin of stretch marks is multifactorial and is influenced by genetic predisposition, mechanical stress (pregnancy, growth after puberty, excessive and rapid weight loss or gain, obesity), use of topical and systemic glucocorticoids, use of antiretroviral protease inhibitors (Indinavir), diseases that present hypercortisolism such as Cushing's Syndrome and genetic disorders such as Marfan's Syndrome. They constitute an extremely common condition in the population, with studies indicating an incidence that can reach up to 88% in pregnant women.1
Although they do not represent health problems, they can have an intense psychosocial impact, especially on women, due to their disfiguring appearance.2 With increased access to information, demand by patients for aesthetic treatments is increasing. There are several therapeutic strategies available, but so far no single modality is considered to be exclusively effective. Multiple sessions using different therapeutic modalities targeting the skin at different levels are often necessary.
There are different therapeutic modalities available that aim to stimulate fibroblasts, promote neocollagenesis, correct pigmentation and atrophy, but until now no single modality is considered exclusively effective, multiple sessions using different therapeutic modalities targeting the skin at different levels are often necessary and have been associated with undesirable adverse effects.3,4 The CO2 laser is associated with pain during the procedure and risk of hyperchromia, which makes it contraindicated for high phototypes.5–8
Microneedling with a tattoo machine for percutaneous collagen induction, described in 1995, may be a therapeutic alternative for superior phototypes. Microinfusion of drugs into the skin (MMP®), described by Arbache et al. In 2013, uses a tattoo machine to promote drug delivery simultaneously with microneedling.9,10
The aim of this study is to describe the technique of microinfusion of drugs into the skin (MMP®) as an alternative in the treatment of striae alba, in order to stimulate collagen production and improve the quality of the skin and striae and evaluate the degree of patient satisfaction with photographic records before and after sessions.
Study design: Ten female patients, aged between 20 and 45 years, with white stretch marks on the buttocks, thighs, abdomen and breasts, who met the inclusion criteria: female, phototype II-V, BMI between 18, 5-25, who read, understood, agreed and signed the informed consent form (TCLE) authorizing the use of data and photos for scientific purposes. Exclusion criteria were: autoimmune diseases, decompensated clinical conditions, pregnancy, lactation, use of systemic immunosuppressants or skin lesions at the application site. The submitted project was approved by the Ethics and Research Committee (CAAE: 79512017.2.0000.5497).
Technique: Before the procedure, photographs of the patients were taken in the frontal position and at a 45-degree angle using a Canon 50D® camera, Canon® 18-135mm lens and Canon Speed Lite® 600 EX-RT flash. Depending on the extent of the area to be treated and the patient's pain threshold, in some cases, a topical anesthetic (7% lidocaine + 7% tetracaine cream) was used 30 minutes before the procedure.
Clean the site with 2% alcoholic chlorhexidine and start the procedure with micropunctures along the stretch marks, using a cartridge with 27 needles of 1.5 mm in length, arranged parallel to each other, with a speed of 80 rotations per minute, using 1- 2 ml, depending on the amount of stretch marks, of sterile medication composed of elastin, chondroitin, ascorbic acid and hyaluronic acid. The endpoint was bleeding dew level II, according to the classification by Lima et al.,7 (Figure 1). The process is carried out along the entire length of the stretch marks, with a first pass, at the end, a revision is carried out and in the places that did not reach level II dew, micropunctures are applied again with drug delivery.

Figure 1 Demonstration of the expected endpoint after microneedling and how the plastic film should be placed.
After the procedure, the area was wrapped with plastic film, and a 12-hour stay was recommended, with subsequent washing with water and neutral soap. The patients were treated with 3 sessions of MMP®, with an interval of 4 weeks between them.
One month after the end of the three sessions, the patients were again photographed as in the beginning. The patients at the end of the sessions, patients rated the treatment by applying a visual analogue scale (VAS) of satisfaction on a ten-point scale, where 0 = no improvement, 1-4 = mild improvement, 5-7 = moderate improvement, 7-9 = good improvement and 10 = complete improvement.
All patients classified the responses between moderate and good at the end of the treatment. (Figure 2 - Figure 6).
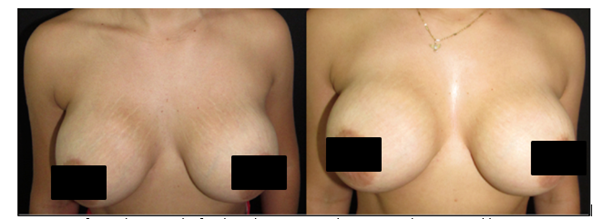
Figure 2 Before and one month after the 3rd treatment session. Best rated as 8 – “good improvement”.

Figure 3 Before and one month after the 3rd treatment session. Best rated as 9 – “good improvement”.

Figure 4 Before and one month after the 3rd treatment session. Best rated as 9 – “good improvement”.
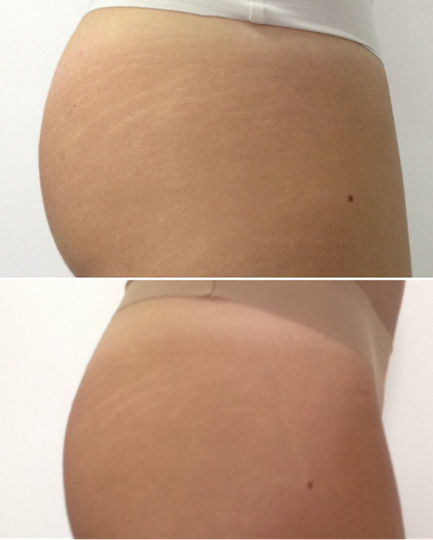
Figure 5 Before and one month after the 3rd treatment session. Best rated as 7 – “good improvement”.

Figure 6 Before and one month after the 3rd treatment session. Best rated as 7 – “good improvement”.
As adverse events, one patient developed hypochromia, managed with tacrolimus 0.1% twice a day, with complete improvement after 6 months. Two patients evolved with hyperchromia, with improvement after one month of local hydration. One patient had pruritus and the appearance of erythematous-edematous papules at the site, with improvement after the application of 0.05% betamethasone cream 2x a day for 3 days.
So far, there is no treatment that has been shown to be able to completely solve this condition, justifying efforts to find more efficient therapies.
Among the proposed treatments, there are studies with 0.1% topical tretinoin, combinations of 20% glycolic acid associated with 0.05% tretinoin and associated with 10% vitamin C.11
However, the topical application of medications has limited results, since the alteration is essentially dermal. The initial attempts to overcome the epidermal barrier for the application of drugs were with the use of Intense Pulsed Light (IPL) and several laser systems, such as fractional CO2, pulsed dye laser 585nm, Excimer laser 308nm, NDYAG 1064nm long pulse, 1550nm, 1565nm and 1540nm.12–18
The mechanism of action of these treatments on stretch marks is the production of sufficient dermal inflammation to destroy the fragmented collagen and the old extracellular matrix, with the formation of new collagen. Among those previously described, the CO2 laser is the most effective in remodeling the extracellular matrix.
In addition to these, microneedling is mentioned in the literature as a therapeutic option. Initially described by Orentreich et al.,19 it is a safe technique with excellent results that causes a dermal inflammatory process and neocollagenesis without total de-epithelialization.19–22
The microneedles promote microlesions that reach the dermis and create columns of superficial bleeding, triggering an inflammatory cascade, resulting in the proliferation of fibroblasts and the formation of type III collagen. In the healing maturation phase, there is conversion of collagen type I, with contraction and reduction of skin laxity.23
In a study, Nassar A et al.22 demonstrated that, in 90% of the treated patients, there was an increase in the thickness of the epidermis, an increase in collagen fibers and in the number of fibroblasts after 3 sessions of microneedling with intervals of 4 weeks.22
The combination of the beneficial effects of microneedling plus the delivery of the drug to its site of action, overcoming the difficulties and irregularities of dermal penetration, has been widely studied and improved, advancing by leaps and bounds. MMP overcomes some technical limitations of other treatments. Sterile medication is aspirated by capillarity and infused concomitantly with the perforation, through shear force, without the need for massage, which reduces the risk of bacterial contamination. In addition, the possibility of regulating the length and speed of needling allows for a more homogeneous application and with less dependence on the applicator's technique. The small size of the needle cartridges facilitates application in areas difficult to access by larger equipment, such as rollers.
It has not yet been determined how much of the retrograde blood flow – actively expelled through the columns generated in the other needling techniques – would act as a barrier to the passive penetration of the medication.
This is where the greatest innovation in the MMP technique resides, since the medication is actively taken to its site of action. Recently, a study using abdominoplasty skin and a high-precision scale quantified the applied medication that actually remains on the skin, thus increasing the safety of the technique.24
Therefore, we describe here a new therapeutic alternative that associates microneedling technique and drug delivery for the treatment of striae alba. This procedure has the advantages of low cost, little complexity with a fast learning curve, quantification of the infused medication, high patient satisfaction rate, possibility of treating patients with high phototypes, with low rates of adverse effects and high tolerability by patients.
None.
Authors declare there is no conflict of interest.

©2023 Gasques, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.