Journal of
eISSN: 2574-9943


Case Report Volume 6 Issue 1
1Serviço de Dermatologia do Complexo Hospitalar Padre Bento de Guarulhos, Brazil
2Faculdade de Medicina da Universidade do Sul de Santa Catarina – UNISUL, Brazil
3Serviço de Dermatologia do Hospital Santa Teresa – Secretaria de Estado de Saúde de Santa Catarina, Brazil
4Serviço de Dermatologia e Anatomia Patológica do Hospital Universitário Polydoro de Ernani São Thiago – Universidade Federal de Santa Catarina, Brazil
Correspondence: Gustavo Moreira Amorim, Adress 135 Duarte Schutel street, apartment 402, downtown, Florianópolis, Santa Catarina, Brazil, Tel +5548999827097
Received: February 18, 2022 | Published: April 8, 2022
Citation: Oliveira TP, Leal LM, Molozzi B, et al. Juxta-articular nodules with transepidermal elimination in a patient with Raynaud’s phenomenon: the challenging differential diagnosis between rheumatoid nodule and granuloma annulare. J Dermat Cosmetol. 2022;6(1):19-21. DOI: 10.15406/jdc.2022.06.00201
We report the case of a 51-year-old female who presented with firm, painful papules and nodules for 9 months, in the extensor proximal metacarpophalangeal and interphalangeal joints in both hands. She did not have a previous diagnosis of rheumatoid arthritis. She also denied arthralgia or arthritis. The patient had livedo reticularis and a history compatible with Raynaud’s phenomenon was reported. The histopathological exam showed well-developed confluent palisaded granulomas with homogenous eosinophilic necrobiosis, with signs of initial transepidermal elimination and no mucin. Thus, we are faced withthe challenging differential diagnosis of rheumatoid nodule preceding rheumatoid arthritis versus perforating juxta-articular granuloma annulare (pseudorheumatoid nodule).
Keywords: rheumatoid nodule, granuloma annulare, livedo reticularis, raynaud’s phenomenon, rheumatoid arthritis
Infiltrated, deep, juxta-articular lesions, with minimal or even no changes on the overlying skin, always represent a challenge for the dermatologist. We present a case of a middle age woman with erythematous papules and nodules over the joints of the hands and elbows, trying to bring the attention to the propedeutic approach and differential diagnosis.
A 51-year-old female, married with two children, housewife, with hypertension on use of hydrochlorothiazide and carvedilol, referred to the dermatology clinic due to appearance of lesions on her elbows and the back of her hands for about 9 months. During the period, the lesions had been progressing in size and number. She reported pain associated with the lesions and, occasionally in some of them, pruritus.
On physical examination, erythematous papules and nodules with a smooth surface, over the metacarpal-phalangeal and in the proximal and distal interphalangeal joints, hands and elbows were noted (Figures 1 & 2). Some of the lesions exhibited small areas of ulceration, covered by keratotic scales (Figure 3). Additionally, livedo reticularis was noted in the upper and lower limbs.

Figure 1 Erythematous papules and nodules with a smooth surface, over the metacarpal-phalangeal and in the proximal and distal interphalangeal joints, on the left hand.

Figure 2 In an enlarged view, erythematous papules over the metacarpal-phalangeal and in the proximal interphalangeal joints, on the left hand. On the the fifth left finger we can identify a yellow crust over the lesion.
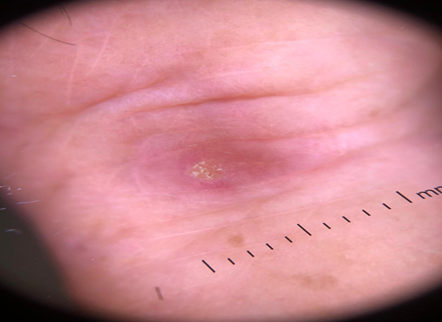
Figure 3 Dermoscopy showing a erythematous papule with a small area of ulceration, covered by keratotic scales.
She denied a previous diagnosis of arthritis or diabetes. She referred pain associated with the lesions, but without episodes of pain or swelling of the joints. She denied dactylitis or morning stiffness. However, she reported pallor, followed by cyanosis and local pain in her feet, predominantly in cold days.
With the diagnostic hypotheses of rheumatoid nodule, granuloma annulare, erythema elevatum diutinum and sarcoidosis, incisional biopsy was performed and histopathological examination showed palisaded epithelioid granulomas in the superficial and deep dermis, without plasma cells, with central fibrinoid necrosis, in addition to vascular ectasia with tumefied endotheliocytes and fibrin thrombi. The process touched the epidermis in foci, suggesting areas of transepidermal elimination (Figures 4 & 5).
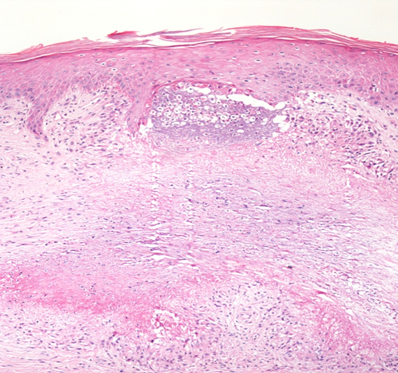
Figure 5 The lesion approaches the epidermis, outlining transepidermal shedding of necrobiotic collagen.
Laboratory investigation did not reveal abnormalities in the blood count or inflammatory proteins; ANA, Anti-Ro, Anti-La, and Anti-HCV were negative, but rheumatoid factor was positive at low titers (40 U1/ml; method: nephelometry; 30 a 79 U1/ml: weakly reactive).
With a diagnosis of rheumatoid nodule, intralesional infiltration of triamcinolone was proposed, combined with the inclusion of nifedipine in the antihypertensive regime aimed at controlling Raynaud’s phenomenon. Although, in our view, the nodules preceded the joint condition and there is no diagnosis of rheumatoid arthritis at the moment, the patient was referred to the rheumatologist for specialized investigation and follow-up. Rheumatologist rule out, at this point, Rheumatoid Arthritis, adopting a watch and wait conduct. Patient remains in follow-up in our out-patient clinic.
Cutaneous rheumatoid nodule is the most common extra-articular manifestation of rheumatoid arthritis,1,2 it is present in approximately 30-40% of patients throughout the course of the disease,3,4 however, 7% of patients already have nodules at the time of diagnosis of rheumatoid arthritis,2 and in patients with Felty's syndrome there is a high incidence of these lesions, up to 75%.5 Generally, rheumatoid nodules do not relate to the severity of progression of the articular condition and can appear before arthritis is installed.3 In any case, they are more frequently present in patients with a long period of illness, directly correlating with titration of the rheumatoid factor.2,3 Up to 90% of patients with nodular disease may have positive rheumatoid factor serology.3,5 Rheumatoid nodules are rarely associated with other diseases.2 However, some studies report presentation of rheumatoid nodules in patients with rheumatic fever, identifying a correlation with severe stages of this disease; when they present the nodules, 90.4% of the patients have cardiac involvement.2 There are also reports of an association with connective tissue diseases, such as systemic lupus erythematosus, however the non-specificity of rheumatological diagnostic criteria may suggest the overlap of rheumatoid arthritis and lupus.2 More sporadic is the association of rheumatoid nodules with spondiloarthropathies and hepatitis C infection.2
Another condition described even less frequently is rheumatoid nodulosis, in which the patient presents with nodular lesions, but does not have chronic synovitis, radiographic alteration or systemic symptoms, which is compatible with the patient in the present report. This condition is more prevalent in men, reaching up to 82% of cases.2 Smoking and local trauma are considered risk factors for the development of nodules.4 The lesions are covered with healthy or slightly erythematous skin, may be solitary or multiple, sometimes coalescing to form plaques or annular lesions,3 vary from 5 mm to a few centimeters in diameter, and can be either adhered to the periosteum and tendons, or mobile.3 They are painless on palpation and are typically located on pressure points or extensor surfaces of joints such as elbows, forearms, metacarpophalangeal and proximal interphalangeal joints, back, heels and other areas.1,4,6
They can also present in extracutaneous sites such as lungs, tendons, vocal cords, occiput and sacrum.2,4 Among the possible differential diagnoses of rheumatoid nodules are synovial cysts, granuloma annulare, gouty tophus, tumoral calcinosis, fibromas, xanthomas and others.7,8 Juxta-articular granuloma annulare (pseudorheumatoid nodule) is a particularly challenging differential diagnosis, presenting more commonly in children and mimicking the histological presentation of rheumatoid nodules.9 In a series of 14 cases of pseudorheumatoid nodule, no perforation or scales were observed, and no patients had a positive rheumatoid factor.9 Histological presentation in those cases was often indistinguishable from that of rheumatoid nodule, with scant mucin present in 11 of 12 cases.
Pseudo rheumatoid nodules, as the other forms of granuloma annulare, seem to affect more women than men; they are often symmetrically distributed. RN are just the opposite: they show a male predominance and usually assymetrical arrangement. Contributing to the case interpretation, patient does not have arthritis/synovitis and laboratory tests were basically normal (low titers of rheumatoid factor lack in specificity value).
Livedo reticularis, especially in its racemose form (irregular, incomplete, asymmetric), can be idiopathic, but it can be associated with collagen diseases in general, especially lupus and antiphospholipid syndrome, in addition to hemopathies, vasculitis, neoplasms, chronic infections and even medications (classically amantadin). Similarly, Raynaud's phenomenon can be idiopathic or secondary to collagen diseases and rheumatoid arthritis. Both can occur together, in overlap. The fact is that, so far, they are clinical findings and do not seem to be associated with systemic conditions in the patient studied.
The pathogenesis of rheumatoid nodules is still uncertain, but an increase in IL-23 and IL-17 cells has been studied in the skin of patients with rheumatoid arthritis compared to healthy patients, indicating that they are related to the formation of nodules.3,4 Likewise, ethiopatogenisis of pseudorheumatoid nodules is not clear. It seems to be a cell-mediated delayed hypersensitive reaction after a external stimulus. An infeccious trigger is also pointed out since treatments with antibiotics may play a role in treatment (specially in generalized forms).9,10
Methotrexate and leflunomide are medications that are known to accelerate the development of rheumatoid nodules, although the mechanism of action is still unclear.4 With regards to treatment, local injection of corticosteroids is the most widely used therapy, although there are few clinical trials demonstrating improvement with this therapy.2 Surgical excision is rarely indicated, except in cases of severe pain, nerve compression, ulcerations or recurrent infections.2 There are no treatment guidelines for pseudorheumatoid nodules since there is still little literature about it; watch-and-wait can be na option if lesions not bothersome. Cryotherapy, excision, and intralesional corticosteroids may be good choices. Probably intralesional corticosteroids have the best eficacy and safe balance.10
In our case, although histopathology favored rheumatoid nodule, we are faced with the challenging differential diagnosis of these two entities, and considering the clinical presentation, normal rheumatologic evaluation and the proximity of these two entities in the histopathological spectrum, the diagnosis of perforating juxta-articular nodular granuloma annulare is most likely.
None.
The author declares there is no conflict of interest.

©2022 Oliveira, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.