Journal of
eISSN: 2574-9943


Case Report Volume 9 Issue 4
Department of Dermatology, Mohammed VI University Hospital Center, Faculty of medicine and pharmacy, Abdelmalek Essaâdi University, Tangier, Morocco
Correspondence: Ouiame EL Jouari, Department of dermatology, Mohammed VI University Hospital Center, Faculty of medicine and pharmacy, Abdelmalek Essaâdi University, Tangier, Morocco, Tel +212645768789
Received: August 25, 2025 | Published: October 9, 2025
Citation: Jouari OEL, Haddad MJEL, Gallouj S. Diagnostic challenges and dermoscopic insights of a secondary syphilis mimicking palmoplantar eczema: a case report. J Dermat Cosmetol. 2025;9(4):111-113. DOI: 10.15406/jdc.2025.09.00303
Background: Syphilis, a sexually transmitted disease caused by the bacterium Treponema pallidum, has seen a worldwide increase in prevalence. Often referred to as "the great imitator," syphilis is notorious for its varied presentations, which can lead to significant challenges in diagnosis.
Case presentation: A 35-year-old Moroccan man presented numerous bilateral palmoplantar erythematous, scaly, and itchy lesions. The lesions were present for 15 days and showed a rapid extension. During the clinical evaluation, multiple palmoplantar erythematous scaly lesions were observed, measuring approximately 0.5 to 2 cm in diameter, surrounded by a keratotic rim on an erythematous base. Dermoscopic findings revealed fine circular scaling around the lesions, defining Biett's collar, with dark erythema in the center that attenuated toward the periphery. Additionally, diffuse scaling was noted, with an orange background, accompanied by a spotty vascular pattern. The patient was initially treated for eczema with topical corticosteroids for 15 days; however, there was no improvement. Given the unusual presentation and potential red flags, serological tests were ordered. Ultimately, a diagnosis of syphilis was confirmed. The patient was prescribed benzathine penicillin, 2.4 million units via intramuscular injection.
At the time of presentation, the differential diagnoses encompassed palmoplantar psoriasis, allergic or irritant contact dermatitis, and dermatophytic infections such as tinea manuum or tinea pedis. Nonetheless, chronic eczematous dermatitis was favored as the initial working diagnosis, given the sharply demarcated erythematous and pruritic scaly plaques confined to the palmar and plantar surfaces.
Conclusions: This case of secondary syphilis presenting as palmoplantar eczema serves as a poignant reminder of the complexities involved in dermatological diagnoses. It emphasizes the need for clinicians to maintain a broad differential diagnosis and to be aware of the potential for sexually transmitted infections to present in atypical ways.
Keywords: syphilis, palmoplantar eczema, dermoscopy
Syphilis, a sexually transmitted disease caused by the bacterium Treponema pallidum, has seen a worldwide increase in prevalence. Often referred to as "the great imitator," syphilis is notorious for its varied presentations, which can lead to significant challenges in diagnosis. This diagnostic challenge is further exacerbated in patients co-infected with HIV, where the virus can alter disease progression and treatment outcomes.1 Although the symptoms of syphilis in HIV-positive individuals typically align with those seen in HIV-negative patients, there exists the potential for atypical manifestations, including severe and rare forms of the disease.
Recent epidemiological data highlight the resurgence of syphilis as a significant public health concern, particularly affecting men who have sex with men and individuals living with HIV.2,3 The rise in cases is often associated with high-risk behaviors, including multiple sexual partners and unprotected intercourse. If primary syphilis goes undiagnosed and untreated, it can evolve into secondary syphilis within 4 to 10 weeks, marked by systemic manifestations that can complicate clinical assessment.
At the secondary stage, syphilis can exhibit a plethora of atypical symptoms, often mimicking more common dermatological conditions, such as palmoplantar eczema.4–6 This phenomenon of masquerading as benign skin conditions makes accurate diagnosis particularly challenging for clinicians. In the realm of dermatology, distinguishing between these conditions can feel like navigating a labyrinth, as the diverse presentations of secondary syphilis can easily lead to misdiagnosis.
This article aims to examine a compelling case that highlights the complexities involved in diagnosing secondary syphilis when it presents in a manner that closely resembles a benign dermatological issue. By exploring this case, we aim to shed light on the importance of maintaining a high index of suspicion for syphilis in patients presenting with atypical skin manifestations, especially in high-risk populations. Ultimately, recognizing the potential for syphilis to imitate other conditions is crucial for ensuring timely diagnosis and effective treatment, thereby improving patient outcomes and public health responses.
A 35-year-old Moroccan man presented to our outpatient department with numerous bilateral palmoplantar erythematous, scaly, and itchy lesions. The lesions were present for 15 days and showed a rapid extension. He had no history of skin disease or other comorbidities and was not taking any medications or drugs. The patient reported no contact with local irritants and denied unprotected sexual intercourse.
During the clinical evaluation, multiple palmoplantar erythematous scaly lesions were observed, measuring approximately 0.5 to 2 cm in diameter, surrounded by a keratotic rim on an erythematous base (Figure 1 & Figure 2). Dermoscopic findings (Figure 3) revealed fine circular scaling around the lesions, defining Biett's collar, with dark erythema in the center that attenuated toward the periphery. Additionally, diffuse scaling was noted, with an orange background, accompanied by a spotty vascular pattern.

Figure 1 Palmar papular lesions, surrounded by a keratotic rim (Biett's collar), on an erythematous base.

Figure 2 a,b,c Multiple erythematous-squamous plaques and papules, infiltrated in some areas, on the sole and dorsal part of both feet.
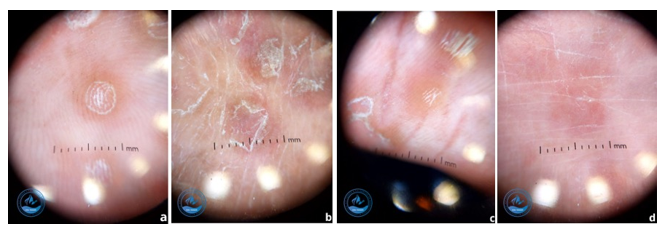
Figure 3 a. Fine circular scaling around the lesions, defining Biett's collar, with dark erythema in the center that attenuated toward the periphery. b. diffuse scaling in some areas. c. orange background. d. spotty vascular pattern.
The patient was initially treated for eczema with topical corticosteroids for 15 days; however, there was no improvement.
Given the unusual presentation and potential red flags, serological tests were ordered. The results indicated that both the Venereal Disease Research Laboratory (VDRL) test and the Treponema pallidum hemagglutination assay (TPHA) were positive, with titers of 1:32 and 1:5120, respectively. Tests for Hepatitis B surface antigen (HBsAg), anti-HBs, anti-hepatitis C virus, and anti-HIV antibodies were negative. Ultimately, a diagnosis of syphilis was confirmed.
At the time of presentation, the differential diagnoses encompassed palmoplantar psoriasis, allergic or irritant contact dermatitis, and dermatophytic infections such as tinea manuum or tinea pedis. Nonetheless, chronic eczematous dermatitis was favored as the initial working diagnosis, given the sharply demarcated erythematous and pruritic scaly plaques confined to the palmar and plantar surfaces.
The patient was prescribed benzathine penicillin, 2.4 million units (MU) via intramuscular injection. Furthermore, we advised him to abstain from sexual activity and recommended serological testing to his partners. Antiretroviral therapy was not administered. After three weeks, the lesions had almost completely disappeared.
The overlap in clinical presentation between secondary syphilis and eczema can lead to diagnostic delays. Clinicians may inadvertently treat eczema with topical steroids or other therapies, delaying appropriate syphilis treatment. This not only prolongs patient discomfort but also increases the risk of transmission to others.
In our case, eczematous dermatitis emerged as the primary clinical consideration due to the morphology and anatomical distribution of the lesions. The absence of therapeutic response to an adequate course of potent topical corticosteroids, however, constituted a pivotal diagnostic clue. Moreover, dermoscopic identification of Biett’s collarette in association with an orange-red background and spotty vascular structures provided additional evidence prompting reconsideration of the initial diagnosis and justified confirmatory serologic testing for syphilis.
Syphilis is a recognized infectious disease caused by the spirochete bacterium, Treponema pallidum subspecies pallidum. The infection is typically transmitted through sexual contact with infected individual.7 In recent years, there has been a notable rise in the incidence of syphilis, which may be attributed to shifts in sexual behaviors, an increased prevalence of HIV, and changing migration patterns.8
Cutaneous manifestations of syphilis are highly variable, underscoring the importance of considering syphilis in the differential diagnosis of any atypical dermatosis. Notably, involvement of the palmar and plantar regions is characteristic, with erythematous papules commonly displaying a scaly collarette. In some cases, the scaling can be prominent, leading to an eczematous appearance,9 as observed in our patient.
In the literature, only a few case reports have documented syphilis mimicking psoriasis,10 lichen planus,11 or pityriasis rosea.12 Hyperpigmented maculopapules have also been observed in some cases.13 However, this is the first documented case, to our knowledge, where secondary syphilis presents with features resembling palmoplantar eczema.
A key dermoscopic feature of secondary syphilis lesions is a diffuse orange or yellowish-red background, typically accompanied by noticeable vascularity. In the case of our patient, a spotty vascular pattern was observed in certain areas, along with both collar-like and diffuse desquamation, in addition to an erythematous and orange background.
Serological testing is crucial for diagnosing secondary syphilis. Screening tests, such as the Venereal Disease Research Laboratory (VDRL) test and the Rapid Plasma Reagin (RPR) test, detect non-specific antibodies. Positive results are confirmed with specific tests, such as the Treponema pallidum hemagglutination assay (TPHA) or the fluorescent treponemal antibody absorption test (FTA-ABS). While these tests are reliable, false positives may occur, particularly in patients with autoimmune diseases or other infections. Therefore, interpreting the results must be done within the broader clinical context, emphasizing the need for an integrated approach that combines clinical evaluation, dermoscopic, and blood testing to establish an accurate diagnosis.
Early detection and treatment of secondary syphilis are essential to prevent complications, including tertiary syphilis, which can lead to serious health consequences such as cardiovascular disease, neurological disorders, and organ damage. Prompt intervention not only alleviates symptoms but also reduces the risk of transmission to sexual partners, thus playing a key role in public health strategies.
The standard treatment for secondary syphilis is benzathine penicillin G, administered via intramuscular injection. For individuals allergic to penicillin, alternative treatment options are available, such as doxycycline or tetracycline.
Additionally, healthcare professionals should emphasize the importance of regular screenings for sexually transmitted infections (STIs) in at-risk populations. Educating patients about safe sexual practices, including the use of condoms and the importance of disclosing their STI status to partners, is essential to prevent the spread of syphilis and other STIs.
Ultimately, an integrated approach that combines early diagnosis, effective treatment, and patient education is essential for managing secondary syphilis and minimizing its impact on both individual health and public health.
From a public health perspective, missed or delayed recognition of syphilis not only perpetuates individual morbidity but also facilitates ongoing community transmission, thereby contributing to potential outbreaks, particularly within high-risk populations. This case underscores the imperative for early serologic screening in patients presenting with atypical palmoplantar dermatoses. Timely identification and treatment are not only critical for optimizing individual outcomes but also represent an essential component of broader strategies to curtail the spread of syphilis and other sexually transmitted infections.
This case of secondary syphilis presenting as palmoplantar eczema serves as a poignant reminder of the complexities involved in dermatological diagnoses. It emphasizes the need for clinicians to maintain a broad differential diagnosis and to be aware of the potential for sexually transmitted infections to present in atypical ways.
By enhancing awareness and education around such cases, healthcare providers can improve diagnostic accuracy and patient outcomes. Ongoing training in recognizing the diverse manifestations of syphilis is essential in preventing misdiagnosis and ensuring effective management, ultimately contributing to public health efforts in controlling sexually transmitted infections.
None.
Author contributions
All the authors contribute to draft and revise the manuscript before approving the final manuscript.
Statement of ethics
Written informed consent was obtained from the patient for publication of the details of their medical case and the accompanying images.
The authors declare there is no conflict of interest.
None.

©2025 Jouari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.