Journal of
eISSN: 2574-9943


Case Report Volume 2 Issue 1
1Department of Dermatology, University Hospital Lauro Wanderley, Brazil
2Medical student, Federal University of Paraíba, Brazil
Correspondence: Jader Freire Sobral Filho, Department of Dermatology, Professor of Dermatology-João Pessoa (PB), University Hospital Lauro Wanderley (HULW), Brazil
Received: August 26, 2017 | Published: January 12, 2018
Citation: Pires CG, Filho JFS, Azzouz MA. Cutaneous mastocytoma in childhood: case report. J Dermat Cosmetol. 2018;2(1):9-10. DOI: 10.15406/jdc.2018.02.00027
The mastocytosis is characterized by local or systemic accumulation of mast cells of unknown etiologic, for which is included in groups of infrequent desease. It generally appears in the childhood or in adults between the third and fourth decade of life and it may lead to different clinical pictures. The case of a six month-old female is presented with lesion cutaneous and histopathological characteristics from this illness.
Keywords: mastocytosis, children, progenitor cells, urticaria pigmentosa, VDRL
Mastocytosis refers to a heterogeneous group of diseases characterized by the hyperplastic proliferation and accumulation of mast cells in one or more organs. The skin is the most organ frequently affected.1,2 The incidence of 2 cases per 300.000 people per year is estimated and may be observed in all ethnic group. The desease is higher predominant in children and in adults between the third and fourth decade of life.3,4 Children are more affected before the age of six months in 50% of the cases.5
The etiology of the disease remains unknown. The current hypothesis is that occurs an initial mutation involving KIT D816V. It triggers an increase in differentiation from progenitor cells and cell clustering, through adhesion molecules CD2, CD58, CD29, CD47 and others.1
A new classification was made by the World Health Organization in 2008 which divides in cutaneous mastocytosisand systemic mastocytosis. The systemic mastocytosis characterized with involvement of the organs including liver, spleen, lymph nodes and/or bone marrow. Among the cutaneous forms, there are three ways: maculopapular cutaneous mastocytosis, cutaneous mastocytoma and diffuse cutaneous mastocytosis.6 The patient may present more than one clinical variant.4Some studies indicate a slight predominance in male.7,8
There is a great heterogeneity of clinical presentation and prognosis even within the same clinical form and it may be related to patient’s age.Mastocytosis may be associated with hypersensitivity, chronic diseases and neoplasms.8 This disease has an indolent initial course which may delay the diagnosis of this uncommon pathology in medical practice.
A 6-month-old female, caucasian, born and resident in João Pessoa, Brazil, presents a yellow-brownish solitary nodule with 2 cm on the face, which appeared at one month of age and remained of stable size (Figure 1). No other symptoms or previous pathologies are reported. The patient didn’t use any medication preceding the cutaneous lesion. He does not have any similar cases in the family. As possible diagnosis, were suggested the hypotheses of pilomatrixoma (Malherbe calcified epithelioma), tricoepitelioma, juvenile xanthogranuloma, X histiocytosis, cutaneous sarcoidosis, Spitz nevus, dermatofibroma and eruptive xanthoma. We chose to perform the skin biopsy whose histopathology was compatible with the diagnosis of solitary mastocytoma (mastocytosis, urticaria pigmentosa). Long bone radiography, VDRL, blood count, abdominal ultrasonography, liver and renal function were requested and all showed no alterations.
The Cutaneous mastocytoma is the second most common type of mastocytosis in childhood and presents as a single or multiple nodule of firm consistency and yellowish, pinkish or brownish color, usually located at the extremities of the limbs (Figure 2).4 If these nodules are exposed to any trauma including friction, they may lead to flushing and systemic symptom, which characterizes the Darier’s sign, considered pathognomonic of this illness.9
The diagnosis is based on a typical cutaneous condition associated with the presence of focal infiltrate composed of mast cells in the dermis in cutaneous biopsy, after exclusion of criteria that establish the diagnosis of systemic mastocytosis, through laboratory tests (Figure 3). The lesions are symptomatic in 60 to 70% of the cases and the main complaints are pruritus, erythema and edema and the presentation of Darier’s sign (Figure 4).8
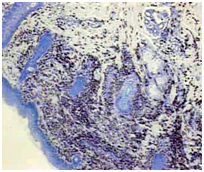
Figure 2 Cutaneous mastocytoma. Highlighted increased number of mast cells stained with toluidine blue where the granules become metachromatic in purple color (magnification 40x) (july 2017).
In this case report the patient had a single brownish nodule on the face, an unusual local of appearance of this dermatosis. He was asymptomatic and did not have the Darier’s sign. The most reliable marker for the severity and extent of disease is the serum level of tryptase.10 In our reality, this test is not widely available and not performed by the patient, as well as the analysis of the mutation in receptor KIT, since histopathology presented characteristics that allowed the conclusion of the case.
There is no consensus on the laboratory tests that should be performed or the frequency with which they should be ordered in children with cutaneous mastocytosis, since most cases of children are restricted to the skin. Therefore, the definitive diagnosis of systemic involvement by the disease would require bone marrow biopsy, which is not routinely performed. In the case presentation, we chose to request long bone radiography, VDRL, blood count, abdominal ultrasonography, liver and renal function. It was planned an annual periodic evaluation of the patient.
There is no curative treatment for cutaneous mastocytosis, only symptomatic, which does not change the course of the disease. As the patient was asymptomatic at the time of the evaluation, no specific therapy was required. It was recommend to the mother to avoid physical, biological and stimulating factors for the release of histamine by mast cells. The mastocytoma was excised at the time of skin biopsy. The prognosis in childhood is good and usually the mastocytoma regresses throughout the first years of life.10
None.
The authors declared that there are no conflicts of interest.

©2018 Pires, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.