Journal of
eISSN: 2574-9943


Case Series Volume 2 Issue 2
Consultant Dermatologist, Eve Clinic Male', Maldives
Correspondence: Riti Acharya MD, Consultant Dermatologist, Eve Clinic Male', Maldives, Tel +9609 7933 94
Received: January 13, 2018 | Published: March 15, 2018
Citation: Acharya R. Cutaneous larva migrans at unusual sites - a case series. J Dermat Cosmetol . 2018;2(2):97-99. DOI: 10.15406/jdc.2018.02.00051
Cutaneous larva migrans (CLM) is a creepy eruption caused by animal hookworm larva infestation on human skin. It is common in tropics, sub‒ tropics and among travelers. CLM presents as serpiginous tract on skin exposed to contaminated soil. Feet, legs, thighs and buttock are usually affected due to walking and sitting on beach areas. Disease is self‒ limiting, usually subsiding within 6‒8 weeks. It is successfully treated with Albendazole tablets. Five cases of CLM among the residents of Maldives is presented in the study with the objective to highlight the unusual locations (chest, abdomen, low back, fingers, forearms) of the disease.
Keywords: creepy eruption, cutaneous larva migrans, serpiginous, sites, itching
Cutaneous larva migrans is skin eruption caused by infestation and migration of animal hookworm larvae in the human skin. It is common in tropics and sub‒ tropics.1‒3 CLM has become common among travellers. The disease mainly occurs in resource‒poor communities.1 CLM presents as typical erythematous, serpiginous, pruritic, migratory skin eruptions. Lesions usually depends on area in contact with the ground like feet, legs and buttocks.2,3 Diagnosis is made on clinical ground of serpiginous eruption in patient with history of exposure.1‒4
Here we report 5 cases of CLM all seen among the residents of Maldives presenting at unusual sites (Table 1).
Cases |
Age (years) |
Sex |
Duration (Weeks) |
Sites |
Symptoms |
Case 1 |
28 |
M |
2 |
Low back |
Itchy rash |
Case 2 |
35 |
M |
2 |
Right lateral chest |
Itching with insect crawling inside the skin |
Case 3 |
12 |
M |
1 |
Right middle finger |
Itching with redness of skin |
Case 4 |
16 |
F |
3 |
Left forearm |
Itchy rash with pain and sticky discharge |
Case 5 |
33 |
F |
3 |
Lower abdomen |
Severely itchy mobile rash |
Table 1 Summary of clinical characteristics of five cases
Case 1: 28years male, presented with itchy eruption over the low back since 2 weeks. He initially noticed a pimple associated with itching. Over a period of week it increased in size and itching. He was diagnosed as Contact dermatitis and treated with topical steroid and antihistamine for a week with mild resolution of symptoms (Figure 1).

Figure 1 Single serpiginous tract resolving with hyper pigmentation and scaling towards natal cleft and progressing towards lower back.
Case 2: 35 years male, presented with itchy rash over the Right lateral chest since 2 weeks. Patient complained of insect crawling inside the skin with frequent change in position. He had noticed the rash developing into blisters while moving forward and resolving with darkening of skin at previous site. He was anxious about the condition and wanted immediate relief (Figure 2).

Figure 2 Single serpiginous tract resolving at one end with hyper pigmentation and active at other end with blistering and surrounding erythema located over Right side of chest lateral to nipple.
Case 3: 12 year old boy complained of severe itching and redness on his left middle finger since 1 week. He had history of regularly beach activities during weekends. Examination revealed erythema and few spots of hyper pigmentation. Serpiginous tract was noticed only on stretching the skin (Figure 3).
Case 4: 16 years female presented with itchy rash over the left forearm since 3 weeks. She also complained of pain and sticky discharge since 5 days. The rash began as a red papule and started moving downward in a linear fashion. Severe itching caused erosions and eczematisation (Figure 4).
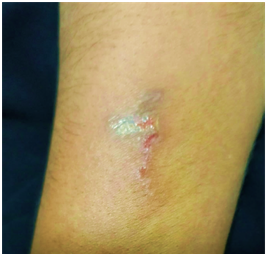
Figure 4 Serpiginous tract with few areas of erosion and eczematisation on extensor of left forearm.
Case 5: 33 years female complained of mobile rash over the lower abdomen since 3 weeks. This was associated with severe pruritus disturbing her sleep. She initially noticed a single red papule which developed into a line moving downward and becoming dark. She was worried when she noticed a new tract appearing at the lower margin of old one (Figure 5).

Figure 5 Serpiginous tract resolving with hyper pigmentation over lower abdomen just above the scar of LSCS. Thin erythematous short tract is seen at the lower end of old lesion.
Presence of typical serpiginous itchy rash supported by epidemiology with history with regular visit to beach, made the diagnosis of cutaneous larva migrans highly suggestive. All the patients were successfully treated with Albendazole tablets 400mg for 3 consecutive days and Anti‒histamine for 2 weeks.
A “creepy eruption” is defined clinically as a linear or serpiginous, slightly elevated, erythematous track that moves forward in an irregular pattern. It was first described by Lee in 1874. When animal hookworm larvae cause a creeping eruption, the disease is called hookworm‒related cutaneous larva migrans (CLM). Main species responsible for CLM are Ancylostoma braziliense and Ancylostoma caninum.1,4 It is a common occurrence in tropical and subtropical countries.1‒4 With the growing frequency of travel to these areas, CLM cases are seen elsewhere.2
Adult worm resides in the intestines of cats and dogs and shed eggs in feces. Warm humid environment with loose sandy soil of the beach favors the egg to develop into infective larva. Humans become accidentally infected through contaminated soil. Upon walking bare foot, sitting and lying in the beach area, the larva penetrates through follicles, fissures, or intact skin. Larva uses their proteases to penetrate the human epidermis. Lesions are usually located on the feet, buttocks, and thighs—i.e. parts of unprotected skin that encounter contaminated soil. Only 7% of lesions are seen on the trunk.2 However, there are increasing number of reports of involvement of unusual locations like scalp, face, oral and genital mucosa.1, 3 Topographic distribution of tract varies with age in endemic area. Children of endemic areas have more lesions on the buttocks, genitals, and hands; whereas lesions in adults are almost exclusively found on the legs and feet.1 Walking bare foot in the beach exposes feet and legs to contaminated soil. Similarly, lying and sunbathing renders thigh, buttock, back and occiput vulnerable for larval penetration in adults. Sitting, crawling and playing in sand might be the possible explanation for larval tracts seen in buttocks and hands of children.
After penetration larvae migrates within the epidermis, causing an inflammatory reaction. Within few days intense itchy rash appears. This develops into linear or serpentine tract that spreads 1‒5 centimeters a day.4 Vesico‒bullous, Papulo‒pustular (Folliculitis), bacterial super infection, eczematous rash are uncommon manifestation of CLM. Lesion heals naturally within few weeks to months of infestation.
Diagnosis is made clinically and is supported by history of travel or residing in endemic area. Occasionally eczematization and secondary infections make diagnosis difficult.3 Epiluminescence microscopy has been used to visualize migrating larvae. Biopsy of the lesion is not helpful for diagnosis. CLM cases are treated with powerful anti helmintics. Ivermectin is the drug of choice.1,3 Albendazole is used in places where Ivermectin is not available. Tiabendazole is the third choice but is poorly tolerated.
Awareness among general population regarding CLM, regular deworming of pets and stay animals in urban area, restricting animals around beach areas, using protective footwear may help in prevention and control of disease.
The publication of this case series is of interest because CLM cases were localized in uncommon topography.
None.
The author declares no conflict of interest regarding the publication of paper.

©2018 Acharya. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.