Journal of
eISSN: 2574-9943


Review Article Volume 7 Issue 4
HNS & FPS Medical Healthcare, 27, Boulevard Dubouchage, 06000 Nice - France
Correspondence: Frédéric Braccini, 27 Boulevard Dubouchage 06000 Nice, France, Tel +33 (0)4 93 91 91 92
Received: November 27, 2023 | Published: December 26, 2023
Citation: Frédéric B, Philippe K, Jérôme P, et al. Concepts and principles of medical rhinoplasty. J Dermat Cosmetol. 2023;7(4):158-163. DOI: 10.15406/jdc.2023.07.00254
Medical rhinoplasty, also known as non-surgical nose treatment, has risen to prominence as a highly favored facial aesthetic procedure. This technique leverages the stable and minimally dynamic nature of the nose, making it an ideal site for filler applications. Hyaluronic acid (HA) stands out as a safe and effective choice due to its homogeneity and diffusion properties. This article provides insights into the methods for successful medical rhinoplasty, emphasizing the importance of anatomical knowledge, precise techniques, and potential complications such as vascular embolization. With over a thousand cases documented since 2008, the authors share their expertise in achieving optimal outcomes while addressing the evolving landscape of non-surgical rhinoplasty.
Keywords: rhinoplasty, nose injections, nose filling with hyaluronic acid
Medical rhinoplasty, also known as non-surgical nose treatment, is increasingly favored in the realm of facial aesthetics. This procedure is especially effective due to the low mechanical stress in the nasal area, where facial dynamics are relatively minimal. Additionally, the stability of the nasal structure, including bones and cartilages, makes it an ideal site for filler injections.1 The longevity of these fillers is more pronounced in the nasal region compared to other facial areas, leading to higher patient satisfaction.2 While initially used primarily for rectifying post-surgery flaws, the application of this treatment has now significantly broadened.
Medical rhinoplasty
Rhinoplasty is predominantly a surgical practice, yet the advent of fillers and botulinum toxin has introduced new considerations for its indications and treatments. The alteration of nasal volumes during surgical rhinoplasty requires general anesthesia and is performed during a procedure that lasts several tens of minutes. It carries risks of swelling, hematomas, and infections.3 Medical rhinoplasty does not replace the surgical technique but rather complements it. It is indeed carried out under local anaesthesia during faster procedures. However, it also involves risks, which will be described later in this article.
Our team was among the pioneers, as documented in international literature since 2008, in showcasing the effective use of fillers for nasal enhancements, and we were also the first to publish a book dedicated to this area.1,4,5,6 Drawing from our extensive experience with over 1000 cases of medical rhinoplasty,1,2,4,6–8 this article delves into a thorough examination of this technique, its applications, and the management of potential complications.1,2
Our approach to treatment involves an artistic analysis of the nose, considering both its standalone characteristics and its integration within the face's three-dimensional context. We focus on two aspects: the individual volumetry of the nose and its harmonious integration with facial features, especially in terms of the naso-frontal angle, naso-labial angle, and cheekbone projection.
The introduction of injectable fillers has also led to their off-label use in non-surgical nose jobs, capable of transforming one's profile in less than 15 minutes. Additionally, the use of fillers for the lips and chin contributes to a comprehensive medical profiloplasty. By treating the cheekbones, particularly their projection, we can subtly adjust the nose's relative volumetry, particularly in profile views.
Anatomical foundations
Understanding the anatomical foundations is crucial for pinpointing the precise area for treatment and recognizing the potential risks associated with injections.4,7–10 The nose, which forms the central third of the face, can be linked to a hollow triangular pyramid with an osteochondral (bone and cartilage) framework. Its base is defined by the nostrils, while the apex is at the nasal root. Over this osteochondral structure, there is a layer of perichondrium and periosteum, followed by a muscular layer, and finally, the skin envelopes the entirety.
We report: (Figure 1)
Understanding the interplay between the nose's mobile and fixed components is vital when planning either medical or surgical rhinoplasty. This understanding informs the approach based on the concept of morpho-dynamic anatomy. Hyaluronic acid (HA) injections in medical rhinoplasty are typically administered deep into the tissue, making contact with underlying cartilage or bone structures. Therefore, a thorough knowledge of both the nasal soft tissues and the structural framework is essential before initiating treatment with filler products.
The nose is associated with various muscles, including elevators, depressors, and muscles that compress or dilate the nares. While their overall role is modest, there are exceptions like the depressor muscle of the nasal tip, which lowers the tip and increases the curvature of the nasal dorsum. The naris dilator muscles can become active, leading to an expansion of the nasal base. The levator labii superioris alaeque nasi muscle elongates the nose, enhances the curvature of the nasal dorsum, and decreases the naso-labial angle, causing a "gummy" smile and contributing to the formation of "bunny lines" along with the nasalis and procerus muscles in the midline.
All these muscles can be effectively targeted with botulinum toxin, allowing for selective immobilization as required for each specific case. The nose is well-supplied with blood through small-sized vessels, with the exception of the region near the internal canthus, where vessels are larger. Its vascular supply is derived from arterial branches of both the internal and external carotid arteries, respectively the ophthalmic and facial arteries. Venous drainage primarily occurs through the angular vein, but also involves the facial vein.
Despite this rich vascular network, the risk of hematoma is relatively low. However, there is a significant risk of vascular embolization, especially in areas like the nasolabial fold and the glabella.
Injections in the tip of the nose are generally safe when standard technical precautions are adhered to.11,12 The motor functions of the nose are controlled by branches of the facial nerve, while sensation is mediated by branches of the trigeminal nerve, specifically the infra-orbital and external nasal nerves. Damage to a nerve branch during a procedure typically does not have major consequences.
Injection products
In these treatments, we've utilized various filling products. To ensure the smoothness of the skin's surface, it's crucial to use products that offer an ideal balance in terms of homogeneity, diffusion potential in the treated areas, and above all, safety.4 The use of permanent fillers is advised against due to associated risks.5
Out of the numerous fillers available, our preference has increasingly narrowed down to HA. This filler is deemed safe for injection in all areas of the nose, including the fixed part and the nasal tip, where the skin tension is significant, and the product's tolerance needs to be optimal. The chosen HA product should be highly cross-linked to ensure greater stability over time.5,6,11
Through years of research and experience, HA emerged as the preferred material. Its relative safety for injection across different nasal regions – both in the stable area of the nose and the tip, where there's high skin tension – makes it an optimal choice. The product needs to be stable, fully tolerant, and safe.4,11,12,13 We utilize HA not only for its camouflaging abilities but also for its structural or physical properties.
Injection techniques
For best results, the procedure should ideally be conducted after applying an anesthetic cream to the entire area being treated, though it can also be performed without anesthesia. Special attention is required for the nasal tip, which is the most sensitive part. A comprehensive treatment plan must be established before beginning injections. Due to the high cutaneous tension in the nasal tip area, excessive injections can lead to product extrusion.4,14,15
Several treatment techniques are described below, with illustrations at the end of this article.
Insert the needle obliquely at a 45° angle until it reaches the bone, using the dominant hand.
With the other hand, press on the nasal bones' side walls with the thumb and index finger to prevent lateral diffusion of the product, which could undesirably reach the inner canthus and lacrimal ducts.
Sometimes, lateral access to fill the naso-frontal angle is necessary for satisfactory results.
A thorough massage of the product should be done afterwards.
For "long noses", filling a dorsum bump can visually create a "shortening" effect by increasing the frontal area's anterior projection.
Always aspirate before injecting and use small boluses. The recommended technique involves a 25G cannula.
Tip correction can be lifting a drooping (parrot beak-shaped) tip or defining a box-shaped nose.
Avoid multiple injection points and apply slow, progressive injection pressure to prevent cutaneous distress. The tip shouldn't remain pale due to the filling.
In over 1000 nasal injection procedures, we've observed no cutaneous necrosis. Necrosis is typically due to an embolic mechanism. Slow, progressive injection reduces cutaneous injury risk.5,11
The nose's rich vascularization and numerous substitution networks mean that for cutaneous necrosis to occur, these networks must be overwhelmed. Higher risk of embolization is associated with low reticulation products. Hence, we recommend high concentration, highly cross-linked products for nasal injections.4
Perform only when not planning simultaneous botulinum toxin injections.
Inject deeply, contacting the nasal spine to open the angle, then balance the columellar lines more superficially.4
This can also be done using a 25G micro cannula.
Primary medical rhinoplasty
Radix and tip treatment (to hide a dorsal hump)
Primary medical rhinoplasty
Reinforced structural support using HA
Secondary medical rhinoplasty
Treatment of “pollybeak nose”
Secondary medical rhinopasty
Treatment of “saddle nose”
Secondary medical rhinoplasty
Global aesthetic improvement
Functional medical rhinoplasty
Right Nasal valve treatment
Severe Complication of a medical rhinoplasty
Embolic disorders 2 days after HA injection, then after several days of hyaluronidase use, according to the protocol described in this article.
Sequences
Before proceeding with HA injections to correct nasal deformities, it's essential to have a thorough discussion with the patient. This conversation should cover the expected results, the entirety of the procedure, and clarify potential complications. Once the patient is fully informed, they should sign a consent form.
It is advisable to avoid over-correction during the initial procedure. Instead, plan a follow-up appointment about two weeks later to assess the results. If necessary, a second injection can be administered to achieve the desired outcome. The results from these treatments can typically remain stable for a period of 18 to 24 months.4,5,13–16
Use of ultrasonography prior to and following nasal filler Injections
The sound waves reflected back to the probe are captured and sent to the processor, where they are converted into digital images. When an ultrasound system is combined with a Doppler system, it is known as a Duplex. In Duplex ultrasound, blood flow is visually represented on the screen in red and blue colors, allowing blood vessels to be distinguished alongside other dermal structures.
All HA fillers are hydrophilic, meaning they bind to water. Since water does not reflect sound waves effectively, HA appears as black (echogenic) or light gray (hypoechoic) on ultrasound images (refer to Figure 2 & Figure 3). This characteristic is crucial in ultrasound imaging for distinguishing HA fillers from other structures.11,17
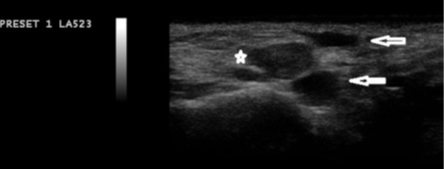
Figure 2 Several Accumulations of Hyaluronic Acid Filler, Including Two Anechoic (Black) and One Hypoechoic Deposit.*
Using ultrasonography guidance, it becomes easier to visualize blood vessels and accurately identify the tip of the cannula, significantly reducing the risk of inadvertently infusing filler into a blood vessel. Ultrasound or duplex examination can clearly display skin, underlying tissues including muscles, veins, and arteries. Additionally, it can reveal any injected filler, allowing for measurement of its pocket size and visualizing the plane of injection.11,18,19 2-dimensional laser speckle flowgraphy (LSFG) is another tool that can be used to identify ischemic states. It is useful for evaluating skin blood flow post-injection, which can aid in predicting the likelihood of skin necrosis.12,20
In terms of managing adverse events following HA injections, ultrasound can be highly beneficial. It's well-established that dissolving the filler can resolve most adverse events. HA fillers are easily detectable with ultrasound, making it possible to identify the size and location of the filler pocket. Under ultrasound guidance, hyaluronidase can be injected precisely into the problematic filler pocket.11,21
However, the real question concerns the absolute safety these devices offer, particularly regarding the risk of embolization. The development of newer, more advanced machines is hoped to address and mitigate these risks effectively.
Indications of medical rhinoplasty
Not every rhinoplasty case is suitable for a medical approach. While medical rhinoplasty is a fantastic alternative and complements traditional surgical methods, these two treatment options should not be seen as opposing each other. It's crucial for surgeons to understand the benefits and limitations of each. The decision for either approach should be guided by an artistic analysis and treatment plan, similar to surgical rhinoplasty. Pre-treatment computerized morphing can also be utilized.
This is one of the best indications for medical rhinoplasty. Treating the nasal tip and filling the junction with the lip and forehead can yield remarkable results.4
Any irregularities such as nasal bridge depression, asymmetry, or deviation can be addressed with fillers. The indications for these fillers are similar to those for cartilaginous grafts. Filler injections following surgical rhinoplasty can also be beneficial. Sometimes, adhesions revealed after nasal splint removal (like a mobilized bone or cartilage fragment) can be effectively managed with a HA bolus to prevent permanent retraction. Repeated injections can lead to fibrosis in the filled space, often avoiding the need for additional surgery.4 This option for post-surgical correction greatly enhances safety and reduces the chances of unsatisfactory results, increasing patient satisfaction. Surgical revisions are generally not recommended until at least a year after the initial surgery.
Using HA in the septal-triangular valve area can counteract the collapse that sometimes occurs after surgical rhinoplasty. This simple technique involves a direct transmucosal injection following local anesthesia with xylocaine nafazoline. The patient can immediately feel the benefits and help determine the quantity of product needed (usually between 0.1 and 0.3 CC per side). This injection serves as an alternative to the surgical use of spreader grafts and may need to be renewed once or twice a year to maintain results. It can also be combined with aesthetic procedures.4,5
Possible complications after nose filling
Complications arising from injections can vary depending on the site of administration. The rate of vascular complications is unclear due to very low number of reports in the literature. It varies between 0.001% and 0.05% of injection procedures.22 The literature notes minor complications like ecchymosis, granulomas, edema, and allergic reactions,11,12 which are managed similarly as for other facial areas. However, two major complications have been reported: skin necrosis and visual loss.
Skin Necrosis
This can result from local ischemia due to overly superficial injections, causing localized necrosis, or from distal embolization leading to extensive necrosis. Local ischemic events are often associated with injections in the nasal tip, dorsum, and glabella.13 Embolic necrosis events are linked to injections in the glabella and nasolabial fold.14 Skin ischemia with necrosis typically heals with moderate scarring and doesn't preclude future injections. Symptoms include immediate local blanching, followed by blue discoloration and then necrosis, along with abnormal pain at the injection site. Infectious complications are also a risk post-HA injection.15
Visual Loss
This serious complication is usually related to HA injections and lipofilling in the glabella or nasolabial fold.16 The prevailing theory suggests retrograde embolization as the primary cause, where direct injection into the dorsal nasal artery or supra-trochlear artery leads to occlusion of the ophthalmic artery. Angiographic studies post-visual loss from facial filler injections indicate retinal ischemia, either diffuse with distal occlusion (hyaluronic acid) or proximal occlusion with retrograde ischemia (lipofilling). This complication is severe, often with little to no recovery, and initial symptoms include sharp retro-bulbar pain, immediate visual loss, and sometimes ophthalmoplegia.17 Currently, there is no consensus on managing these complications Table 1.
|
Early complication |
Late complication |
|
Erythema |
Granuloma |
|
Edema, swelling |
Migration |
|
Echymosis, bruising |
Hypertrophic scar |
|
Lump, nodule |
Telangiectasia |
|
Blanching, discoloration |
Skin defect |
|
Skin necrosis |
Infection |
|
Infection, biofilm |
|
Table 1 Early and Late Complications17
Treatment of major HA complications
The primary goal in treating complications from filler injections is to dissolve the filler, improve blood flow, and promote vasodilation. Dayan et al.,19 recommend using hyaluronidase for all cases of vascular compromise, regardless of the filler type, due to its ability to reduce edema and theoretically lower the pressure in the occluding vessel.
The protocol includes local injections of hyaluronidase every 6 hours, administration of Enoxaparin 0.4mL, systemic steroids (1mg/kg/day for 3 days), application of nitroglycerine paste, and wound care, sometimes involving hyperbaric oxygen therapy. While aspirin and intravenous (IV) prostaglandins have been suggested, their efficacy is not conclusively proven.20 Antibiotics and antivirals may also be necessary if local infections occur.
In cases of visual loss, it's critical to administer a peribulbar injection of hyaluronidase within the first 90 minutes. This should be done using a 27G needle, injected in the inferolateral part of the orbital arch, along the floor of the orbit.4,21,23 This approach aims to rapidly address the occlusion and mitigate damage.
Precautions to mitigate the risk of complications:
Anatomical considerations play a central role in the prerequisite knowledge for performing medical rhinoplasty.1 It is essential to have a thorough understanding of the organization of soft tissues and nasal structures to place filler products in the correct planes, i.e., in contact with cartilaginous or bony structures. This optimization enhances the expected outcome and minimizes risks, particularly vascular ones.22 The integration of ultrasound to visualize blood vessels and guide injections can be a promising supplement, aiming for increased precision and safety.11,17 The morphodynamic anatomical approach emphasizes the need to tailor interventions based on individual patient characteristics.
The preference for hyaluronic acid (HA) due to its safety profile and lasting effects aligns with the literature consensus.4,11,12,13 Other permanent filler products should be contraindicated5 due to the high skin tension in the treated area and the considerable vascular risk. Complications underscore the importance of meticulous injection techniques and the prompt use of protocols, including hyaluronidase, to resolve undesirable events.
The decision to proceed with medical rhinoplasty is made only after a thorough pre-treatment discussion with patients to manage expectations and obtain informed consent.1,4
We advocate for ongoing collaboration among practitioners, researchers, and technology developers to enhance the safety and efficacy of medical rhinoplasty. The continuous exploration of new tools, such as two-dimensional laser speckle flowgraphy (LSFG), illustrates the field's commitment to advancing diagnostic capabilities and refining treatment strategies.12,20
Medical rhinoplasty continues to gain popularity, with an increasing number of practitioners adopting it. Standardized protocols are necessary to homogenize practices and secure the procedure. Continuous training should encompass these practices so that practitioners have the knowledge and tools needed to navigate the changing landscape of non-surgical interventions while prioritizing patient safety and satisfaction. Rigorous follow-up of results will allow for protocol adjustments.18,23
Medical rhinoplasty is highly effective in achieving aesthetically pleasing and stable results. An artistic approach is crucial for executing this technique and tailoring the treatment to each individual. This method demands a thorough understanding of nasal anatomy and the utilization of appropriate products. Adherence to strict protocols is essential to minimize side effects, particularly the risk of embolic migration of the injected product. Practitioners must be meticulous in their technique and vigilant in monitoring for any adverse reactions, ensuring a balance between aesthetic enhancement and patient safety.
None.
The authors declare there is no conflicts interest.

©2023 Frédéric, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.