Journal of
eISSN: 2574-9943


Research Article Volume 7 Issue 4
1Ticiano Rossi Clinica e Spa-Private Clinic-Rua Martin Jacob, 130, Centro, Santa Maria de Jetiba–ES, Brazil
2CMA - Private Clinic-Rua Pedro Caneppa, 100, Centro, Paracambi - RJ, Brazil
Correspondence: Ticiano Rossi, Ticiano Rossi Clinica e Spa-Private Clinic-Rua Martin Jacob, 130, Centro, Santa Maria de Jetiba-ES/Brasil, CEP 29645-000, Tel +55 (27) 999746880
Received: September 15, 2023 | Published: October 3, 2023
Citation: Rossi T, Sardenberg CV. Brazilian hug lips: a new approach to treating inverted and atrophic lips with hyaluronic acid. J Dermat Cosmetol. 2023;7(3):109-113. DOI: 10.15406/jdc.2023.07.00246
Background: Inverted and atrophic lips are always a major challenge when we opt for treatment with hyaluronic acid. In most cases, the correct indication would be surgical correction (Liplifting). However, we bring a new technique to provide improved lip inversion with aesthetically natural results.
Methods: Six female patients aged between 30-80 years old and without any previous lip treatment were selected. The application of hyaluronic acid was carried out following the criteria developed by the authors, and deposition of hyaluronic acid using the C-shaped technique or "embrace" technique (HUG lips).
Results: By following the technique and quantities (ml) of hyaluronic acid described, we achieve natural and satisfactory results for lip eversion.
Conclusion: According to our study, we observed an improvement in lip definition, correcting atrophic lips, without the need for surgery, with a high level of satisfaction among treated patients.
Keywords: lips, lip filler, difficult lips, atrophic lips, inverted lips, new lip technique
The lips have a crucial importance both in facial aesthetics and in the performance of functions such as chewing and speaking. A beautiful lip is related to attractiveness and youth Figure 1.
Every day, the search for the correction of inverted lips that are difficult to treat conventionally, non-surgically, is becoming more common in our clinics, mainly using hyaluronic acid. We know that these types of lips are still a major challenge when using hyaluronic acid, as due to anatomical changes, we do not always achieve the desired results.
The main causes of inversion and atrophy of the upper lip are:
The result of this entire process in the region is, in addition to its lengthening, a thinning of the vermilion, erasure of the philtrum, atrophy and inversion of the lip.
Lip vascularization
The lips are very vascular and the path, distribution and location of the labial arteries are very variable. There are countless articles published that describe the patterns of the lip vasculature and there is no technique or standard of lip treatment with hyaluronic acid that is better in terms of safety. All techniques can carry risks, especially in relation to arterial occlusion (Figure 2).
“In general, the labial arteries can run in three anatomical planes: submucosal plane or wet mucosa,intramuscular plane, semimucosal plane or dry vermilion. The lips are formed by an internal portion - labial mucosa or wet lip, a transition zone- lip vermilion or semimucosa and an external portion represented by skin and its appendages. At the limit between the internal portion of the labial mucosa and the transition zone of the lip or semimucosa, there are the fibers of the orbicularis oris muscle, which delimits two fat compartments:
Clinically, the results suggest that a safer plane for injecting soft tissue fillers is the Subcutaneous plane, as the artery is located in both the upper and lower lip, deep in the submucosal plane. Despite concerns about not achieving optimal volume results, especially in lips with poor volume, the subdermal plane should be the target. From an anatomical point of view, deep injection into the body of the labrum presents a greater risk of intra-arterial injection, as the needle/cannula is inserted blindly. Superficial injection can be controlled visually as the tip of the needle/cannula is still visible. This can be used to control shallow product placement as opposed to deep product placement. Positioning the product superficially and closer to the wet/dry mucosa transition line can invert the lip, as the lip is placed against the other lip or teeth.2
For lips with little volume and an increase in the distance from the nasal base to the lip contour, we know that the first choice of treatment is surgical reconstruction with the Liplift technique (Gull-wing surgery) for later refinement with hyaluronic acid. However, in this study we want to demonstrate the improvement obtained through treatment exclusively with HA, without prior surgical intervention.
In this report, we describe an unprecedented technique for treating thin, inverted, atrophic lips called BRAZILIAN HUG LIPS, using a filler with high malleability and low residual BDDE– Rennova lips lido , 20 mg/ml of hyaluronic acid ( Panaxia LTD Bat Sheva , Israel ) to improve lip aesthetics naturally.
06 patients were selected, according to the inclusion criteria:
Guidelines were followed to avoid unwanted results.
Guidelines for improving aesthetic results with lip augmentation (to avoid "duck" or "sausage" lips.3,4
The filler used was – Rennova lips lido , 20 mg/ml of hyaluronic acid ( Panaxia LTD Bat Sheva , Israel) and the cannula Softfil microcanula flexível essencia 22Gx50mm.
Before treatment, a 30-minute medical consultation was held to review medical history and explain the procedure. A consent form was signed by the patients.
Topical anesthetic (manipulated formula: prilocaine 1.5%, tetracaine 7%, Lidocaine 7% gelcreme) was applied to the junction of the upper and lower lips, as well as throughout the perioral region.
Marking and technique
Flexible cannulas were chosen because they allow a uniform distribution of the filler and, due to their malleability, they make it possible to create a C-shaped contour across the entire lip. The blunt tip and greater flexibility of the microcannula provide sliding under the dermis with less trauma and greater safety when compared to the traditional hypodermic needle. Furthermore, it is possible to approach a wider region with fewer insertion holes, which considerably reduces adverse effects such as ecchymosis, hematomas and the risk of intravascular injection; thus improving post-procedure recovery time.5,6
Upper lip treatment
Two pertuits were initially made with a gauge needle 21Gx25,4mm at 0.5 cm, below the right and left nasal ala (Figure 3). Next, a 22-gauge flexible cannula (Softfil microcanula flexível essencia 22 Gx 50mm) Was introduced. The cannula was positioned in the subdermal plane, in a downward path towards the moist lip or submuscular region. To facilitate access to the submuscular plane, we perform a slight eversion of the lip, using the thumb and index finger in a rotational movement (Figure 4).
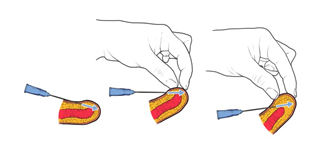
Figure 4 Description of the movement of the cannula from the skin to the sub muscular plane (the cannula contours and hugs the lip – HUG Lips).
In this plane (submuscular), we deposit a bolus of AH (amount described below) and then move the cannula upward in a “hug” (HUG), depositing the AH along the entire path by retroinjection until reaching the central point of the red (semi mucous). At this limit, we stop the injection so that there is no unsightly interference with the contour.
We perform this sequence in 03 to 04 paths, starting parallel to the philtrum towards the labial commissure (right and left sides of the upper lip), as described below:
Totaling in the upper lip, approximately 0.73 ml.
Usually, atrophy and inversion are seen more frequently in the upper lips, but it is common to need to adjust the proportion of the lower lips to obtain better results.
Lower lip treatment
To restore volume to the lower lip, we divide it into right and left sides, locate the median point on the right and left sides and, from this point, draw a perpendicular line 1.5 cm downwards. In this place, we make the cannula entry hole (Figure 3). The cannula is introduced in a subdermal plane, now moving upwards towards the moist lip or submuscle region. In this plane (submuscle), we deposit a bolus of HA (amount described below) and then make a downward movement of the cannula, hugging the lip and depositing the HA along the entire path by retroinjection until reaching the vermilion-skin transition. At this limit, we interrupt the retroinjection so that there is no unsightly interference with the contour.
We carry out this sequence in 03 to 04 routes, as described below:
Totaling for the lower lip, approximately 0.78 ml
Once the application is complete, we perform a light local massage in order to homogenize the hyaluronic acid, as immediate moldability is interesting for the chosen technique and product. After 15 days, we reevaluate the patient to determine whether or not supplementation with the product is necessary. If any asymmetry occurs, correction with hialuronic acid is necessary. We emphasize that atrophic lips, in mostcases, require new treatment approaches with hyaluronic acid. Therefore, if necessary, we choose to do it 30 days after the initial procedure to allow the tissues to adapt to the product applied.
The procedure demonstrated good tolerability and it was reported minimal discomfort. It is important to mention that the relatively fast procedure and the hyaluronic acid with lidocaine contributs to the painless. Most patients considered the results satisfactory, considering the difficulty of treating inverted and atrophic lips from an aesthetic and functional point of view (Figure 5–9). The incidence of adverse effects was low, including swelling, bruises and discrete asymmetry. No cases of ETIP (Persistent Delayed Intermittent Edema) and vascular occlusion were reported.
The results of the articles published on the anatomy of the labial vascularization revealed that the most frequent location of the superior and inferior labial arteries is the submucosal plane with 58.5%, followed by the intramuscular 36.2% and the subcutaneous position 5.3%. The depth of the superior labial artery in the upper lip
was 5.6 ± 1.3 mm, while the depth of the inferior labial artery in the lower lip was 5.2 ± 1.4 mm. The artery is more often located in the red lip than in the cutaneous (hairy) lip: upper lip (83% vs. 18.7%) and lower lip (86.2% vs. 13.8%); this relationship was more evident, especially in the midline, as in all volunteers investigated (100%) the artery ran purely within the red lip. Clinically, these results support a more superficial injection technique in the subcutaneous plane regardless of lip position. An approach perpendicular to the labrum may increase safety as the artery is most often located in the red labrum.2
Tansatit et al.,7 suggested placing filler in the middle of the lip to avoid injection between the muscular layer and the mucosa. Cotofana et al.,8 agreed that injection in the subcutaneous plane is safer for lip augmentation and better for avoiding superficial arteries than in the midline of both lips.
Based on anatomical observations, the red edges of both lips are safe for superficial injection of fillers. All areas of the lower lip are secure, reflecting the small size of the ascending arteries. Recent studies have demonstrated that injections in the submucosal or moist mucosal plane carry greater risks of arterial occlusion. In the technique described here, we use the cannula perpendicular to the artery's path, which minimizes the risks of embolization and occlusion. In conventional filling techniques for inverted lips, the cannula is used lateral to the
oral commissure, which makes it possible to apply hialuronic acid in the submuscle plane and also in the red lip, but the technique presented here brings greater safety through injection. Perpendicular to the labial artery. Furthermore, the retroinjection from the submuscle plane to the vermilion, as if the hialuronic acid “embraced” the lip, provides projection and remodeling with elegant results for inverted lips that are difficult to correct.
The vast majority of patients with thin lips require treatment with hialuronic acid on the vermilion of the lip and also on the labial mucosa (moist lip) to provide anterior projection and volume, respectively. The “hug” technique - HUG LIPS - allows the product (hialuronic acid) to be distributed evenly from the submuscle plane to the subdermal plane (vermilion) and, as it is perpendicular to the path of the labial artery, the technique makes the technique safer. Unlike the effective techniques previously described, we noticed an advantage of the “hug” technique - HUG LIPS – with greater eversion power and uniformity not only in the areas with product bolus, but also throughout its entire path. Patients with lip volume deficit should be treated prioritizing volume restoration for Subsequente contour treatment, if necessary.
This is a new and innovative cannula technique that offers greater safety and a satisfactory degree of results for the treatment of “difficult” inverted and thin lips. Despite the high degree of satisfaction, safety and low rate of adverse effects, it is interesting to carry out new studies with a larger number of patients.
None.
Authors declare there is no conflict of interest.

©2023 Rossi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.