Journal of
eISSN: 2574-9943


Case Report Volume 2 Issue 5
1Department of Pathology, Armed Forces Medical College, India
1Department of Medicine, Armed Forces Medical College, India
1Department of Dermatology, Armed Forces Medical College, India
Correspondence: Deepak Vashisht, Department of Dermatology, Armed Forces Medical College, Pune-40, India, Tel +9173 7868 9648
Received: September 09, 2018 | Published: October 3, 2018
Citation: Vashisht D, Anwita S, Sukriti B, et al. Basal cell carcinoma arising at tattoo site of radiotherapy field marking in a patient with multiple malignancies. J Dermat Cosmetol. 2018;2(5):71-73. DOI: 10.15406/jdc.2018.02.00088
Basal cell cancer is one of the commonest human malignancies. It has also been reported as a part of various genetic syndromes. There are scarce reports of basal cell carcinoma arising at tattoo sites with roughly ten cases reported in literature on cosmetic tattoos, postulated to be due to the trauma of procedure and carcinogenic effect of dyes in tattoo ink. Therapeutic ionizing radiation causing DNA damage is an independent risk factor. Herein we report a patient with history of Non Hodgkins lymphoma, adenocarcinoma stomach, colon and prostate, treated with radiotherapy and chemotherapy, which developed Basal cell carcinoma at the site of therapeutic tattoo used for radiotherapy skin marking.
Keywords: basal cell carcinoma, tattoo ink, radiation
BCC, basal cell carcinoma; CHOP, cyclophosphamide, doxorubicin, vincristine, and prednisone; NHL, Non hodgkins lymphoma; DNA, deoxyribonucleic acid
Basal cell carcinoma (BCC) typically develops over sun exposed sites as a slow growing locally invasive lesion which rarely metastasizes. It is thought to originate from pleuri potential cells of the basal layer of epidermis. The loss of inhibition of patched/hedgehog intracellular signalling pathway which is vital for regulation of cell growth and differentiation and changes in tumour suppressor genes like TP53 play a central role in pathogenesis of basal cell carcinoma.1 Basal cell carcinomas have also been described at previous trauma sites of piercings, surgical scars and at sites of tatoo inks.
The pathogenesis of malignancy developing at a tattoo site can be explained by trauma induced by the procedure, the carcinogenic dyes and metallic salts in the tattoo, and by product of these dyes upon exposure to radiation, and the chronic inflammatory reaction in dermis to get rid of the foreign particle.2 Therapeutic radiation is an independent risk factor for development of Basal cell carcinoma specific to the site of radiation field due to radiation induced mutagenesis with direct DNA damage forming mutagenic photoproducts as well as indirect DNA damage due to formation of reactive oxygen species.3 Also Basal cell carcinoma has been reported in Non Hodgkin lymphoma survivors treated with radiotherapy and chemotherapy with alkylating agents leading to DNA damage.4 Various syndromes associated with gastrointestinal and reproductive tract malignancies have Basal cell carcinoma in addition to the other primary neoplasms.5 We report a patient with multiple malignancies treated with radiotherapy, chemotherapy and surgery that developed Basal cell carcinoma at the site of previous tattoo used for skin marking for radiotherapy.
An 80years old male patient presented to our department with a gradually progressive asymptomatic dark colored lesion at the site of black tattoo ink used for marking skin for directing the radiotherapy beam for adenocarcinoma prostate 12years before. His past medical and surgical history included: multiple treated malignancies in last 35 years in the form of Non Hodgkins lymphoma occurred in 1983 treated with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) regimen and radiotherapy, adenocarcinoma of the stomach in 1996 and adenocarcinoma of the rectum in 2003, which were managed with chemotherapy and surgical resection. In 2006 the patient developed an adenocarcinoma of the prostate managed with chemotherapy and radiotherapy. No family history of multiple malignancies was present in parents, siblings or children. Examination revealed a solitary well defined black colored plaque measuring 05cm x 02cm at 11 o’ clock position from umbilicus in umbilical region not associated with any tenderness or overlying ulceration (Figure 1). Dermoscopic examination revealed leaf like areas at the periphery of the lesion, blue grey ovoid nests, absence of pigment network and specks of black and brown pigment (Figure 2). An incisional biopsy was done from the lesion in view of dermoscopic pattern favoring basal cell carcinoma. Histopathology revealed stratified squamous epithelial lining with irregular proliferation of tumour from undersurface of epidermis and extending into dermis (Figure 3). Tumour nests comprised of basaloid cells with peripheral palisading showing mild pleomorphism with high nucleocytoplsmic ratio. Retraction artefact was seen (Figure 4). There was no lymphovascular or perineural invasion. Immunohistochemistry revealed BerEP4 positivity with no loss of BCl2, negative for epithelial membrane antigen and Carcinoembryonic antigen. Histopathological findings were consistent with Basal cell carcinoma. Patient was managed with wide surgical excision of tumour with 05mm margins and post operative histopathology specimen showed all margins free of tumour. Patient is on regular follow up for any recurrence of Basal cell carcinoma at the same or any other site and also other malignancies.

Figure 1 Solitary well defined black colored plaque measuring 05cm X 02cm at 11 o’ clock position from umbilicus in umbilical region.
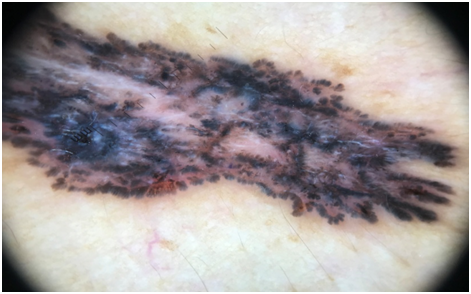
Figure 2 Leaf like areas at the periphery of the lesion, blue grey ovoid nests, absence of pigment network and specks of black and brown pigment.
An individual’s risk of developing BCC depends on genotypic, phenotypic and environmental factors. While the primary risk factors are UV light exposure and genetic predisposition there are other significant risk factors like advanced age, male sex, radiation exposure in the form of UVA, UVB or therapeutic ionizing radiation, iatrogenic immunosuppression, immunodeficiency states, genetic instability syndromes and occupational factors.6 The cause of BCC developing in our patient at a photo protected site at the site of previous therapeutic tattoo ink for guiding radiotherapy beam in the setting of multiple gastrointestinal and prostatic malignancies appears to be multifactorial. Majority of cases of melanoma and BCC reported in literature have been on black cosmetic tattoo pigments.7 Black tatoo contains polycyclic aromatic hydrocarbons, phenols, dibutylphthalate, bezophenone etc which may be genotoxic or cytotoxic.8 Also these compounds have been shown to release reactive oxygen species and other by products like nitroaniline, nitrotoluene and dichlorobenzene on radiation exposure and LASER therapy which have been found carcinogenic9 which could possibly explain the pathogenesis of BCC in our case. Therapeutic ionizing radiation is also an independent risk factor for development of basal cell carcinoma.10
Also our patient had multiple malignancies with Non Hodgkins lymphoma (NHL) at onset treated with radiotherapy and chemotherapy. NHL survivors have a 1.88 higher risk of second malignant neoplasms in comparison to general population owing to DNA damage to mutagenic chemotherapy from alkylating agents and radiation therapy triggering a multistage mechanism of carcinogenesis.4 This can possibly explain the multiple cancers our patient developed after the treatment of NHL 35years back. Genetic instability can also have a role in the pathogenesis of multiple cancers with syndromes like Lynch syndrome, Cowden syndrome and Muir-Torre syndrome associated with multiple gastrointestinal malignancies with specific mutations. Genetic studies could not be done for our patient; however there was no family history of multiple malignancies.
Our case highlights the multifactorial etiology, dermoscopic and histologic features of Basal cell carcinoma. Less than ten case reports exist in literature on basal cell cancers arising at sites of tattoos.7Malignant melanoma has been reported at sites of tattoo ink markings for radiotherapy in cancer survivors 11 but there are no reports of basal cell carcinoma arising in such a setting of concomitant therapeutic tattoo and ionizing radiation. The observation that the BCC occurred on a photo protected site at the site of tattoo ink exposed to ionizing radiation favors a strong argument for the cocarcinogenic effect of tattoo ink and therapeutic radiation. Other factors like trauma to skin involved in tattooing, iatrogenic immunosuppression, genetic instability syndromes leading to multiple malignancies or therapy for Non Hodgkins lymphoma as a causal factor for other malignancies including BCC cannot be ruled out.
None.
Authors declare that there is no conflict of interest.

©2018 Vashisht, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.