Journal of
eISSN: 2574-9943


Case Report Volume 4 Issue 1
1Department of Dermatology, Federal University of Bahia, Brazil
2Department of Pathology, Federal University of Bahia, Brazil
Correspondence: Bruno de Oliveira Rocha, Departments of Dermatology and Pathology, Federal University of Bahia, Salvador, Bahia, Brazil, Tel +55(71)99389-2323
Received: April 12, 2019 | Published: February 25, 2020
Citation: Rocha BO, Souza ES, Lordello L, et al. Back-to-basics of hemangiosarcoma of face and scalp: a case report. J Dermat Cosmetol. 2020;4(1):20-21. DOI: 10.15406/jdc.2020.04.00143
Introduction: Hemangiosarcoma is a rare vascular malignant neoplasm. Diagnosis is based on both clinical and histopathological features. Case Presentation: An 85-years-old white man presented with a 1-year history of progressive lesions on face and scalp. Physical examination revealed violaceous infiltrative plaques, with ulceration and bleeding, on the face and scalp, associated to numerous violaceous satellites papules. Histopathological examination revealed a neoplastic proliferation represented by slit-like anastomosing vascular channels that dissociated collagen fibers in the dermis, lined by atypical endothelium with moderately hyperchromatic and pleomorphic nuclei. Diagnostic conclusion was cutaneous angiosarcoma. Conclusions: Cutaneous angiosarcoma most often affects males (2:1), mostly Caucasian patients over 70 years old. It may originate from blood or lymphatic vessels. The most common form affects the face and scalp. There are varying degrees of cellular atypia, anastomosing slit-like channels, dissociation of collagen fibers, occasional hyaline globules and areas of hemorrhage. Immunohistochemistry confirmed blood vascular origin with diffuse positivity for CD34 and focally diffuse for factor VIII. We emphasize the need of clinicopathological correlation for early recognition and treatment.
Keywords cutaneous angiosarcoma, hemangiosarcoma
Hemangiosarcoma is a rare vascular malignant neoplasm with a predilection for the skin, involving head and neck in about 50% of cases.1 It is characterized by violaceous plaques, which progress to extensive infiltrative lesions that may ulcerate and bleed. The diagnosis is made by clinical and histopathological analysis, being necessary to rule out Kaposi’s sarcoma.2–3 We describe herein a case of cutaneous angiosarcoma with typical clinical presentation.
An 85-year-old white man presented with a 1-year history of progressive lesions on the face and the scalp was referred to our service. Initially, the lesion was a violaceous papule, measuring about 1cm, in frontal region. In the past 5 months, the patient noticed an increase in the lesion. Physical examination revealed violaceous infiltrative plaques, with ulceration and bleeding, on the face and the scalp, associated to numerous violaceous satellites papules (Figure 1). The patient reported hypertension, glaucoma, and cardiac use of pacemaker in medical history, without any evidence of immunosuppression.
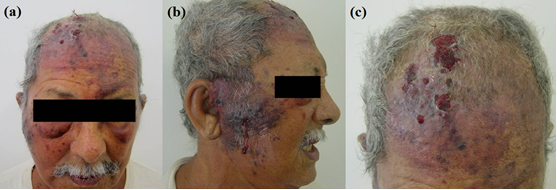
Figure 1 (a) Asymmetry of the face due to edema in the right parotid region and eyelid ecchymosis. (b) Violaceous infiltrated ulcerated and bleeding plaque in the right malar region, with peripheral violaceous papules. (c) The same aspect lesions in the scalp.
Histopathological examination revealed a neoplastic proliferation represented by slit-like anastomosing vascular channels that dissociated collagen fibers in the dermis, lined by atypical endothelium with moderately hyperchromatic and pleomorphic nuclei. There were some hyaline globules and areas of hemorrhage (Figure 2a). Immunohistochemistry revealed diffuse positivity for vimentin and CD34, and focally positivity for factor VIII. Human herpes virus 8/latency-associated nuclear antigen (LANA-1/HHV8) staining was negative, and the proliferation index (measured by Ki67) was between 15-20% (Figure 2b-2f). Diagnostic conclusion was cutaneous angiosarcoma.
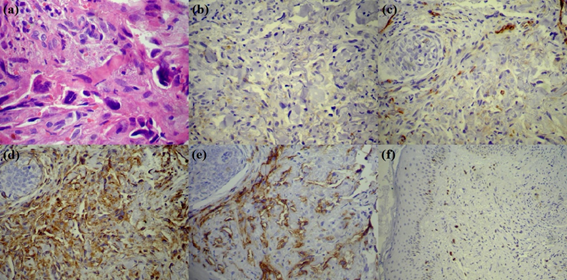
Figure 2 (a) Neoplastic vascular proliferation. Hemorrhage and dissociation of collagen in the periphery. Cellular atypia, hyperchromatism and nuclear pleomorphism (HE,400x). (b) LANA-1/HHV8, absence of nuclear staining (200x). (c) Factor VIII (von Willebrand), focal cytoplasmic staining in neoplastic cells (200x). (d) Vimentin, diffuse cytoplasmic staining in areas of anastomosis (200x). (e) CD34, diffuse membrane staining in cells lining the vascular slits (200x), (f) Ki67, proliferative index ranging from 15 to 20% (200x).
Laboratory studies revealed decreasing on serum hemoglobin (9.6g/dL), and increasing on serum creatinine (1.8mg/dL). Serology for HIV1/2 and HTLV1/2 were negative. CT scan showed no evidence of enlarged lymph nodes or lung metastases, noting expansive and infiltrative formation in soft tissues of the face and scalp. Parotid and thyroid US showed a diffuse and increased volume. There was a lymph node adjacent to the parotid and a cystic nodule in the thyroid, both without evidence of malignancy on cytopathologic examination after fine needle aspiration was performed.
Cutaneous angiosarcoma most often affects males (2:1), mostly Caucasian patients over 70 years old.4,5 It may originate from blood or lymphatic vessels. The most common form affects the face and scalp, being characterized by purplish lesions, often multiple, when starting on the scalp.4–6 In early stages, lesions may simulate benign aspect, even on histopathological evaluation, showing aspects similar to capillary hemangioma,2,3,5 as for instance with our patient. Progression of the lesions usually occurs, occasionally including ulceration and bleeding,3 as seen in this case.
As for the histopathological findings, there are varying degrees of cellular atypia, anastomosing slit-like channels, dissociation of collagen fibers, occasional hyaline globules and areas of hemorrhage,2,5 present in our patient’s biopsy. Immunohistochemistry confirmed blood vascular origin with diffuse positivity for CD34 and focally positivity for factor VIII. Despite the proliferation index between 15 and 20%, the loss of positivity for factor VIII suggests the presence of high-grade areas. LANA-1/HHV8 staining was negative, ruling out the possibility of Kaposi’s sarcoma.
The involvement of regional lymph nodes is observed in 20-30% of cases. Regarding prognostic factors, size seems to be the most important one. Lesions which are smaller than 5cm indicate better prognosis.5,6 The patient described had infiltrative extensive lesions, which indicate poor prognosis, with no metastasis observed up to the present date. Death rates are related to the local extension of the tumor, invasion and metastasis, especially to lungs and liver.7 Survival rates after 5 years are about 15%, with death estimated within 15 months after diagnosis in 50% of cases.8 The current treatment options are often not curative to extensive lesions. Radical surgery and postoperative radiation therapy modalities are used for most patients; however, relapses are common.5,9–11
It can be observed, therefore, that the diagnosis of hemangiosarcoma in the elderly patients is compatible with the clinical features in our patient, considering gender, ethnicity, age, and clinical aspect of lesions. We emphasize the need of clinicopathological correlation in cases like this, due to the fact that early recognition and treatment are crucial to the patient survival.
The author declare that there is no conflicts of interests.
None.
None.

©2020 Rocha, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.