Journal of
eISSN: 2574-9943


Case Series Volume 8 Issue 3
1Private Practice, Belo Horizonte, MG, Brazil
2Federal University of São Paulo, São Paulo, Brazil
3Federal University of São Paulo, São Paulo, Brazil 3Department of periodontology and implantology, University of Guarulhos, Sao Paulo, Brazil
4Private Office, São Paulo, SP, Brazil
5Let´s HOF Academy, São Paulo, Brazil
Correspondence: Luiz Avelar, Clínica DOMANI BH, Private Practice, Belo Horizonte, MG, Brazil, Tel +5531 99982-0692
Received: July 30, 2024 | Published: August 13, 2024
Citation: Avelar LE, Haddad A, Carnevali ACN, et al. Advanced strategies for mental augmentation with hyaluronic acid – a case series using the profile approach. J Dermat Cosmetol. 2024;8(3):62-65. DOI: 10.15406/jdc.2024.08.00268
Objective: Hyaluronic acid (HA), due to its high reversibility, low incidence of adverse events, and patient acceptance, is a viable option for correcting mild to severe retrognathia. This work aims to systematize and suggest non-surgical options that impact facial profile through the ProT technique.
Methods: Depending on the level of retrognathia, HA injections are administered in varying depths, with severe cases also requiring neuromodulator treatment. Proper injection techniques and materials are recommended to enhance treatment effectiveness and durability.
Results: The case series showed significant improvements in mental region projection and definition, with 40%, 50%, and 70% enhancements for cases 1, 2, and 3, respectively. Case 2 also had a 15% increase in the distance from the oral commissure to the mandibular base and a 3.25 cc volumetric gain in the mental region. These results indicate substantial improvements in facial aesthetics following the intervention.
Limitations: We can consider individual anatomical variations, tissue response, and the clinician´s ability as limiting factors for technique reproducibility.
Conclusion: The Profile Technique (ProT) utilizes HA gels and, optionally, neuromodulators tailored to each patient's facial profile to effectively correct retrognathia. This approach results in significant improvements in facial aesthetics while ensuring safety, making ProT a minimally invasive and effective method for enhancing facial harmony.
Keywords: hyaluronic acid, mental region, facial profiles, customization techniques, aesthetic enhancement, rethrognatism
The number of professionals performing aesthetic procedures is increasing every year worldwide. However, there is still no validated and standardized methodology for training these new injectors.1 Due to the growing number of novice injectors, the development of clear and direct methodologies, such as the one presented in this case series, can provide significant support in performing hyaluronic acid (HA) procedures, facilitating the training of new professionals and enhancing patient safety.2
HA, with its high reversibility profile, low incidence of adverse events, high patient acceptance, and minimal recovery time, is a viable option for mental corrections in patients with mild, moderate, and severe retrognathia.3 It is evident that HA is not a substitute for established treatments like orthognathic surgery and orthodontics. However, it can serve as an enhancement to these treatments, as a preoperative mockup for self-image adjustment, or as an option for patients who, for various reasons, cannot or do not wish to undergo more extensive or invasive interventions. The diversity of HA fillers in combination with different application techniques represent a challenge for clinicians in selecting the correct products and planning the most appropriate techniques. It is essential to have a detailed understanding of the specific rheological properties of each HA product to determine its suitability for the desired correction according to each patient's facial profile. The careful choice of product and technique directly impacts the effectiveness of the aesthetic and functional outcomes, requiring a solid foundation of technical knowledge and clinical experience.4
For this reason, we propose the Profile Technique (ProT), a straightforward methodology to enhance the profile of the lower third of the face. This technique integrates the selective application of (HA) and, when necessary, neuromodulators. The selection and combination of products are carefully tailored based on the specific facial profile characteristics of each patient. Additionally, the technique provides specific options to guide the clinician, which will be demonstrated through clinical cases.
In this case series, we applied the (ProT) to three patients aiming to improve the lower third of the face, specifically the mental region. All subjects provided written informed consent prior to inclusion. The study followed guidelines for Good Clinical Practice and adhered to the Declaration of Helsinki for human investigations.5,6
Analysis of the mental region
Evaluating the facial profile is essential for an accurate treatment plan.7 For this analysis, the patient should look towards the horizon, avoiding cervical hyperextension. The alignment of the anatomical points glabella, subnasal, and pogonion classifies patient´s profile into straight (Orthognathic, Class I), convex (Retrognathic, Class II), or concave (Prognathic, Class III) (Figure 1). Mental augmentation is indicated for Class II patients.6,7
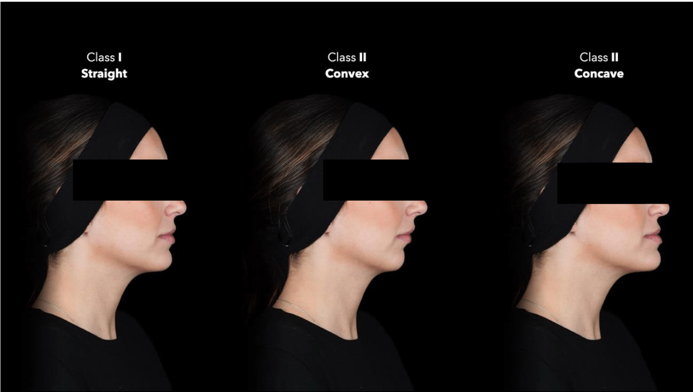
Figure 1 Demonstrating the different classes of facial profiles: Class I - straight (Orthognathic), Class II - convex (Retrognathic), and Class III - concave (Prognathic). Mental augmentation is indicated for Class II patients.
Then, the level of retrognathia is assessed using a vertical line, Ricket´s line, passing tangentially to the subnasal point and perpendicular to the Frankfurt plane. An ideal mental projection consists of the chin touching this line or being set back by up to 4mm. Additionally, the upper lip should pass 2 to 6 mm beyond this line, while the lower lip should touch the line or pass by 4 mm (Figure 2).8

Figure 2 Lateral view using a vertical line passing tangentially to the subnasal point and perpendicular to the Frankfurt plane.
The profile technique (ProT)
The ProT is a treatment strategy for the mental augmentation that focus on the aesthetic and functional needs. ProT utilizes neuromodulators to adjust muscular dynamic of the region, as well as HA to restore projection, volume, and mental symmetry if needed. This approach depends on the patient's level of mental projection. For a mild retrognathia (4 -7 mm setback of the chin), deep HA injections into a submuscular plane are indicated. For moderate retrognathia (7 - 10 mm setback from the chin), a deep (supraperiostial) and superficial (subcutaneous) approach should be performed. Finally, for severe retrognathia (greater than 10 mm setback), deep and superficial HA injections are used after neuromodulator treatment of the mentalis muscle.9
Importantly, for deep-supraperiostial injections, a firm (high G') HA with excellent vertical projection capacity is suggested. These injections should be done using needles positioned in a 90-degree angle in contact with the bone. For superficial-subcutaneous injections, flexible HA (low to moderate G') with better tissue integration are suggested. Application of superficial HA should be done using a 22-G cannula using linear retroinjections across the entire treated area. Neuromodulators injections into mentalis muscle enhance the durability and improve the projection capacity of the HA treatments.
Three female patients (35, 42 and 53 years) presented in this case series signed an informed consent form and authorization for image use. They all had the same primary complaint: deficiency in the mental region with varying severity degrees. Cases 1 and 3 were treated at the private clinic of the first author (LEA), while case 2 was treated at the private clinic of the last author (MG). Participants were instructed to wash their faces with water and soap, followed by facial asepsis using 2% alcoholic chlorhexidine (Riohex, Rioquímica, São Paulo, Brazil). Then, all participants were photographed and/or stereophotogrammetry images were taken. Marking points were drawn according to the treatment strategy (Figure 3), and local infiltrative anesthesia was administered (Mepisv, DFL, Brazil) just at the cannula entry point.
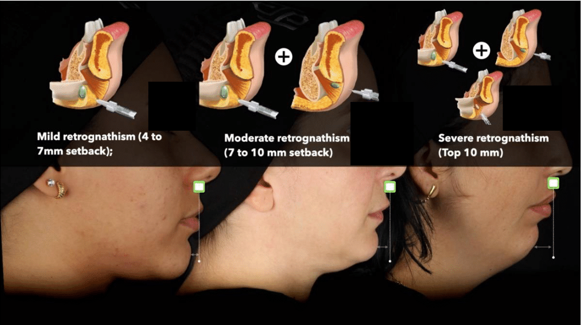
Figure 3 Presentation of the three types of retrognathia according to the vertical line, showing the setbacks of the chin from the subnasal point and the simulation of HA application.
In all cases, deep HA injections were performed using Restylane Lyft (Galderma, Uppsala, Sweden), a product with 1% cross-linking, NASHA technology, and high vertical projection capacity. In cases 2 and 3, subcutaneous applications were also performed using Restylane Defyne (Galderma, Uppsala, Sweden), a product with 8% cross-linking, OBT technology, and moderate projection capacity. Moreover, in case 3, a vial containing 500 Speywood units of abobotulinumtoxin A (Dysport, Ipsen, Wrexham, United Kingdom) was reconstituted with 2 ml saline solution and 10 U were using a 0.3 ml syringe (BD, Becton Dickinson, Juiz de Fora, MG, Brazil) into mentalis muscle (Table 1).
|
Case |
Device |
Hyaluronic acid |
Botulinum toxin |
Plane |
Amount HA |
Distance A - B after treatment |
|
1 |
Needle |
Restylane Lyft (RL) |
None |
Supraperiostial |
0,4 (Two points, each point 0,2 ml) |
60% / 100% |
|
2 |
Needle and Cannula |
Restylane Lyft (RL) and Restylane Defyne (RD) |
None |
Supraperiostial and subcutaneous |
3 ml (2ml RL. Four points, each point 0,5ml and 1ml RD) |
50% / 100% |
|
3 |
Needle and Cannula |
Restylane Lyft (RL) and Restylane Defyne (RD) |
Yes, 10U |
Supraperiostial and subcutaneous |
4 ml (2ml RL. Four points, each point 0,5ml and 2ml RD) |
30% / 100% |
Table 1 Presentation of the treatment approach, product used, neurotoxin application, application plane, quantity of product applied, and percentage reduction in chin distance from the nasal point
A noteworthy point regarding the results (Figure 4) is the quantitative reduction achieved in all cases and highlighted in Figure 5. Cases 1, 2, and 3 showed reductions of 40%, 50%, and 70% respectively, in the central distance from the chin to the Ricketts’ line post-treatment. Additionally, case 2 demonstrated a vertical improvement with a 15% increase in the distance from the oral commissure to the mandibular base. In the same case, the volumetric gain in the mental region measured by stereophotogrammetry was 3.25 cc.

Figure 4 (A) Before and after chin augmentation in a patient with mild retrognathia. (B) Before and after chin augmentation in a patient with moderate retrognathia. (C) Before and after chin augmentation in a patient with severe retrognathia.
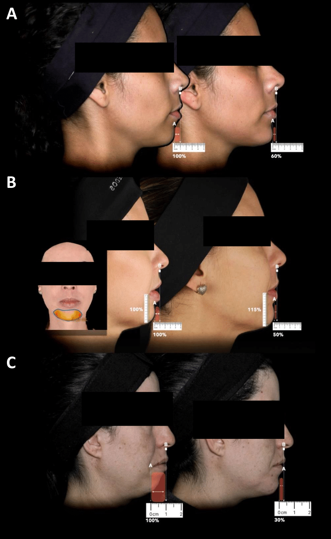
Figure 5 (A) Before and after chin augmentation in a patient with mild retrognathia, demonstrating the quantitative reduction of the vertical line distance. (B) Before and after chin augmentation in a patient with moderate retrognathia, demonstrating the quantitative reduction of the vertical line distance and the volumetric gain measured by stereophotogrammetry. (C) Before and after chin augmentation in a patient with severe retrognathia, demonstrating the quantitative reduction of the vertical line distance.
The results of this case series demonstrated significant improvements in the projection and definition of the mental region. Specifically, improvements of 40%, 50%, and 70% for cases 1, 2, and 3 respectively were observed. In case 2, there was also a 15% vertical increase in the distance from the oral commissure to the mandibular base, along with a volumetric gain of 3.25 cc in the mental region, as calculated by stereophotogrammetry. These results indicate a substantial improvement in the lower face of the participants, following the intervention. Undeniably, performing combined treatments enhanced our results,10 especially in cases of more severe retrognathia, which in the past would not have been mitigated so simply and with such a low level of morbidity. When we assess the incidence of adverse events associated with the use of HA in the mental region and compare them to surgical procedures, we observe a considerable positive difference (low event rate) in favor of injectables.11,12,13
Choosing the right HA, application plane, and the order of treatments is also relevant. In deeper planes, which are more affected by pressure and muscle force, firmer products like Restylane Lyft are the best option.14 For more superficial planes, products that offer moderate projection and high flexibility, such as Restylane Defyne, are more appropriate as they naturally follow the movements of the lower face.15,16
Ideally, neuromodulators should be administered before other procedures to maximize precision and minimize diffusion to adjacent muscles, particularly due to the potential for post-treatment edema with injectables. The waiting time between the neuromodulator application and the performance of other procedures should be around 15 to 20 minutes, respecting the drug's mechanism of action, which takes approximately 5 to 10 minutes to bond and/or internalize into motoneurons.17
The doses applied in our case series varied from 0.4 to 4 ml of HA. Despite some studies suggesting a potential risk of bone resorption in the mental region following HA application, the debate remains unclear regarding the actual risks of this phenomenon.18,19 In 2024, an interventional study (78 participants) and an observational study (95 participants) showed a significant association between HA injection and bone resorption, with 35.9% of patients exhibiting discernible resorption. There was no significant difference in resorption between the subgroups of high-volume (>1 ml) and low-volume (≤1 ml) injections.19
Therefore, patients should be informed about this possible complication and advised to undergo radiological examinations after multiple injections. Although bone resorption is a concern, its severity is generally minor, with no observed periapical lesions or significant aesthetic reduction. This suggests that while the complication should be acknowledged, it should be interpreted rationally and without excessive anxiety.19
The (ProT combines the application of different types of HA gels in different facial planes, with or without the use of neuromodulators, depending on the patient's facial profile. This case series highlights the technique's effectiveness in correcting mild to severe retrognathia, providing significant improvements in facial aesthetics with a favorable safety profile. Detailed analysis of the facial profile and the strategic application of HA and neuromodulators, based on the severity of retrognathia, resulted in notable reductions in the central chin distance and satisfactory volumetric gains. These findings reinforce the safety and efficacy of ProT as a minimally invasive and highly effective alternative for the correction of retrognathia, significantly improving the facial harmony of patients.
None.
The authors declare no conflict of interest.
This study received no funding.

©2024 Avelar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.