Journal of
eISSN: 2373-4396


Clinical Report Volume 17 Issue 4
Nursing Department, College of Health Sciences, Arsi University, Asella, Oromia Regional State, Ethiopia
Correspondence: Lidiya Tekle Gebreyohannes, Nursing Department, College of Health Sciences, Arsi University, Asella, Oromia Regional State, Ethiopia
Received: July 08, 2024 | Published: August 12, 2024
Citation: Gebreyohannes LT, Wake AD. Hypertension recommended self-care knowledge, attitude, practice and its predictors among hypertensive patients in Ethiopia: a cross-sectional study. J Cardiol Curr Res. 2024;17(3):92-100. DOI: 10.15406/jccr.2024.17.00611
Introduction: Globally, hypertension is a significant public health challenge. Elevated BP is responsible for 7.6 million deaths per annum globally, which is greater than any other risk factors. The aim of the study was to assess the hypertension recommended self-care knowledge, attitude, practice, and its predictors among hypertensive patients at follow-up clinic.
Methods: A cross-sectional survey was done on 120 hypertensive patients who were on follow-up clinic at Asella Referral and Teaching Hospital. The data were collected from patients from 23/12/2020 to 16/01/2021 by face-to-face interview and medical records review. Data were entered into Epi Data version 4.2.0.0 and exported to SPSS version 23.0 for statistical analysis.
Results: The level of good knowledge, favorable attitude, and good practice towards recommended self-care was 60.0%, 52.5%, and 50.8%, respectively. Formal education. AOR=3.615, 95%CI (1.262, 10.352), p=0.017 and receiving information about self-care from healthcare providers during follow-up. AOR=3.307, 95%CI (1.226, 8.926), p=0.018 were factors significantly associated with knowledge towards recommended self-care. Having good knowledge towards self-care. AOR=13.449, 95%CI (4.794, 37.728), p=0.000 was significantly associated with attitude towards recommended self-care. Receiving information about self-care from healthcare providers during follow-up was 3.887 times. AOR=3.887, 95%CI (1.232,12.261), p=0.021, having good knowledge towards self-care. AOR=3.195, 95%CI (1.161,8.794), p=0.025, having a favorable attitude towards self-care. AOR=3.093, 95%CI (1.198,7.990), p=0.020 were factors significantly associated with practice towards recommended self-care.
Conclusion: The level of good knowledge, favorable attitude, and good practice towards recommended self-care among hypertensive patients on follow-up was unsatisfactory. Health education programs about hypertension self-care need to take place to improve the knowledge, attitude, and practice of the patients.
Keywords: hypertension, knowledge, attitude, practice, self-care, predictors
Hypertension is a silent killer, a number of individuals with hypertension are unconscious of it due to the fact that it may have no warning clinical features.1 The global burden of hypertension exceeds 1.4 billion individuals.2 The rate of elevated SBP (110-115- and 140-mm Hg) raised considerably between 1990 and 2015 globally. Deaths associated with increased SBP also augmented.3 The prevalence of high systolic blood pressure (HSBP) is 18.9% in Brazil, with an annual 0.4% increase rate.4
The study done among adult residents in Arba Minch, Ethiopia, showed that the prevalence of hypertension was 18.92%,5 whereas 29.28% from the study conducted in Bahir Dar City, Ethiopia,6 27.4% from the study done in Gondar City, Ethiopia,7 12.5% from the study done in Debre Markos town, Ethiopia.8 In Ethiopia, the proportion of uncontrolled hypertension is high.9 The likelihood of having hypertension has been found to increase among advanced age, overweight, khat chewing, low fruit and/or vegetable consumption, and being from rich households.5
Globally, hypertension is a significant public health challenge.10 Worldwide, hypertension is the chief cause of cardiovascular disease (CVD) and premature death.11 High BP is a principal modifiable cause of premature death. It is one of WHO’s global targets for the prevention of non-communicable diseases (NCD).12 Elevated BP is responsible for 7.6 million deaths per annum globally, which is greater than any other risk factors.13 Hypertension is a major cardiovascular risk factor and the leading cause of mortality globally.14 Hypertension of ≥140/90 mm Hg SBP/DBP was a significant risk factor of CVDs mortality, particularly among individuals aged 35–59 years.15 Raised BP is a risk factor for mortality from coronary heart disease (CHD).16
CVD deaths associated with hypertension augmented from 171259 to 270839 between 2000 and 2018 in United States.17 There is an increased risk of all-cause, CVD-specific, heart disease or cerebrovascular disease related mortality among untreated hypertensive adults or those treated but not having control from a report of the USA.18 The study report from Mexico revealed that half of all cardiovascular deaths that happened yearly in individuals aged ≥50 years are related to above optimal levels of SBP.19
The study revealed that BP was strongly linked to vascular and kidney-related mortality among the Mexican population.20 The study conducted in China showed that the occurrence of hypertension among middle aged people raises the risk of CVD and stroke mortality.21 There are J or U shaped associations between BP parameters and mortality among individuals with chronic kidney disease.22 People with high BP at the beginning of TB treatment had a greater mortality rate at 2-year follow-up.23 A study also reported that there has been an association between the magnitude of hypertension and the human development index.243
In developing countries, a major concern was not given for hypertension. This is due to the fact that a health policy and research of the past years were mainly focused on infectious diseases.25 The risks for CVD have been growing intensely in Ethiopia. However, because of the high impact of communicable diseases, less emphasis is given to NCDs like hypertension.26 The complications related to hypertension had a substantial share of the medical ward mortality rate, according to a study report from Ethiopia. The complications that were common causes of hospitalization and inpatient death were cerebrovascular and cardiovascular complications.27
Monitoring high BP globally through understanding what is occurring at a country level is significant to find the solutions to address high BP.12 The evidence suggests that prevention, detection, treatment, and control of this issue should obtain high priority.10 As far as hypertension is a silent killer, it is desirable to create a system for aiding early detection and monitoring.5 Since the magnitude of uncontrolled hypertension is high in Ethiopia, the study suggests the level of adherence towards antihypertensive medication, physical exercise, and alcohol abstinence need to be improved.9
Despite the widespread use of antihypertensive medications, global mean BP has remained constant or reduced somewhat over the past 4 decades. However, a proportion of hypertension has augmented, particularly in low and middle-income countries (LMICs).11 Findings concerning the addressed hypertension recommended self-care knowledge, attitude, practice, and its predictors among hypertensive patients are substantial to developing crucial strategies compulsory to improve the impacts of hypertension. However, there is a limitation of study that has addressed hypertension recommended self-care knowledge, attitude, practice, and its predictors among hypertensive patients on follow-up clinics in a study area. Therefore, the aim of this study was to assesshypertension recommended self-care knowledge, attitude, practice and its predictors among hypertensive patients on follow-up clinics. The findings of this study are supportive of a government, hospitals, hypertensive patients, local policy implementers, stakeholders, and researchers to manage and control the serious impact of complications associated with hypertension, which are increasing dramatically worldwide.
Study area and period
The study was conducted at Asella Referral and Teaching Hospital from 23/12/2020 to 16/01/2021. It is located in the Arsi Zone, which is found in Oromia Regional State, 175km far from the capital city of Ethiopia, which is Addis Ababa. Asella Teaching and Referral Hospital was built by Ethio-Italian cooperation in 1958.28
Study design
An institutional based cross-sectional survey was conducted.
Source population
All hypertensive patients attended Asella Referral and Teaching Hospital.
Study population
The study population were hypertensive patients who fulfilled the inclusion criteria and volunteered to participate in the study.
Eligibility criteria
Inclusion criteria: All hypertensive patients aged ≥18 years.
Exclusion criteria: Hypertensive patients who were severely ill and physically incapable of being interviewed at the time of data collection.
Sample size determination
For this study, we have done the complete survey by census method of all hypertensive patients on follow-up clinic at Asella Referral and Teaching Hospital. We found the final sample size of 120 for this study. This is because since the survey was done, all hypertensive patients on follow-up clinic, who fulfilled the inclusion criteria and were willing to participate in the study were enrolled in this study.
Sampling techniques and procedures
The hypertensive patients were reached by using a medical registration card during conducting this study. Initially, we checked those hypertensive patients who fulfilled the inclusion criteria. Then, after we asked them for their volunteers to take part in this study, all hypertensive patients who were on follow-up on a day of survey and volunteered to take part were included in the study.
Study variables
Independent variables
Age, gender, educational status, average monthly income, residence, duration of hypertension, receiving information about self-care from healthcare provider, marital status, occupation, and presence of comorbidity.
Operational definition
Good Knowledge: when patients respond the mean or above means score out of the knowledge question.
Poor Knowledge: when patients respond below the mean score on knowledge question.
Favorable Attitude: when patients respond the mean or above mean score out of the attitude questions.
Unfavorable Attitude: when patients respond below the mean score on attitude questions.29
Good practice: when patients respond the mean or above mean score out of the practice questions.
Poor practice: when patients respond below the mean score on the practice questions.29-31
Data collection instrument
Different experts were involved to develop the questionnaires needed for this study. During this, the questionnaire was developed by reviewing the relevant literature.29-31 The questionnaires were designed in four parts. The sociodemographic characteristics of the patients, knowledge related questions, attitude related questions, and practice related questions.
Data quality control
The quality of data was kept by different schemes. The questionnaires were pretested on 16 hypertensive patients out of the study area. Training was provided for data collectors. Supervisors were involved, and they gave feedback on the spot. The completeness of data was cheeked throughout the work.
Data processing and analysis
Data was checked, coded, and entered into Epi-Data version 4.2.0.0 and then it was exported to Statistical Package for the Social Sciences (SPSS) version 23.0 for statistical analysis. The outcome variable was dichotomized and coded as (poor knowledge=0, good knowledge=1), (unfavorable attitude=0, favorable attitude=1), and (poor practice=0, good practice=1). Descriptive statistics were performed and finally summarized by using texts, tables, and figures. Both binary and multivariable regression analysis were done to identify the variables associated with knowledge, attitude, and practice towards self-care. The strength of the association was displayed by using crude odds ratio (COR) and adjusted odds ratio (AOR) with 95% confidence interval (CI). The variables with p-values <0.05 in the multivariable logistic regression were considered statistically significant.
Sociodemographic characteristics of respondents
A total of 120 hypertensive patients were enrolled into this study, providing a response rate of 95%. The majority 50(41.7%) of the patients were aged between 40-59 years with the mean age of 49.38 years, minimum 19 years, maximum 92 years, and standard deviation (SD) of 16.684. More than half 69(57.5%) of the patients were male. Concerning to the Ethnic background of the patients, 55(45.8%) were Oromo. 43(35.8%) of the patients were Muslim. 87(72.5%) of the patients have attended formal education. (Table 1).
|
Variable |
Category |
Frequency |
Percent |
|
Age |
19-39 years |
35 |
29.2 |
|
40-59 years |
50 |
41.7 |
|
|
≥60 years |
35 |
29.2 |
|
|
Gender |
Male |
69 |
57.5% |
|
Female |
51 |
42.5% |
|
|
Ethnicity |
Oromo |
55 |
45.8% |
|
Amhara |
36 |
30% |
|
|
Gurage |
16 |
13.3% |
|
|
Others |
13 |
10.8% |
|
|
Religion |
Orthodox |
33 |
27.5% |
|
Muslim |
43 |
35.8% |
|
|
Protestant |
32 |
26.7% |
|
|
Others |
12 |
10% |
|
|
Marital status |
Unmarried |
19 |
15.8 |
|
Married |
101 |
84.2 |
|
|
Educational level |
No formal education |
33 |
27.5 |
|
Formal education |
87 |
72.5 |
|
|
Occupation |
Employed |
32 |
26.7 |
|
Unemployed |
88 |
73.3 |
|
|
Average monthly income |
≤2500 Ethiopian Birr |
58 |
48.3 |
|
>2500 Ethiopian Birr |
62 |
51.7 |
|
|
Duration of the disease |
≤5 years |
83 |
69.2 |
|
>5 years |
37 |
30.8 |
|
|
Residency |
Urban |
68 |
56.7 |
|
Rural |
52 |
43.3 |
|
|
Presence of co-morbidities |
Yes |
39 |
32.5 |
|
No |
81 |
67.5 |
|
|
Receiving information about Self-care from HCP during follow-up |
Yes |
93 |
77.5 |
|
No |
27 |
22.5 |
Table 1 Socio-demographic characteristics of hypertensive patients attending Follow-up clinic at Asella Referral and Teaching Hospital, Ethiopia, 2021. [n= 120].
Knowledge of hypertensive patients towards recommended self-care
The hypertensive patients’ level of good knowledge towards recommended self-care was 60.0% [n=72, 95%CI; 51.7, 70]. (Figure 1)
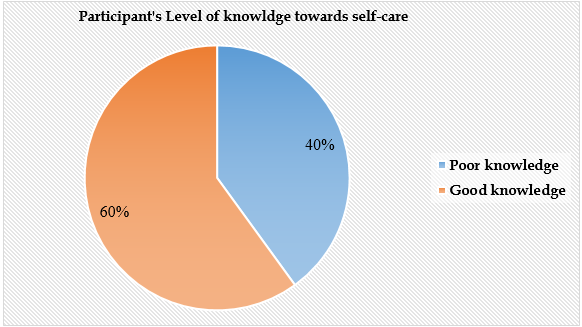
Figure 1 level of knowledge towards recommended self-care among adult hypertensive patients attending follow-up clinic at Asella referral and teaching hospital, Ethiopia, 2021. [n = 120]
Attitude of hypertensive patients towards recommended self-care
The hypertensive patients’ level of favorable attitude towards recommended self-care was 52.5% [n=63, 95%CI; 44.2, 61.6]. (Figure 2)
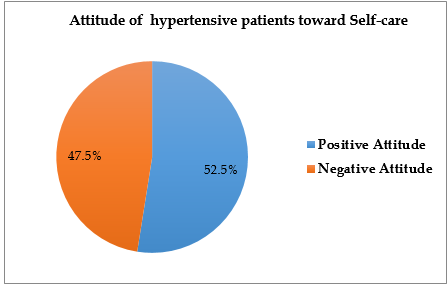
Figure 2 level of Attitude towards recommended self-care among adult hypertensive patients attending follow-up clinic at Asella referral and teaching hospital, Ethiopia, 2021. [n = 120]
Practice of hypertensive patients towards recommended self-care
The hypertensive patients’ level of practice towards recommended self-care was 50.8% [n=61, 95%CI; 43.4, 58.3]. (Figure 3)
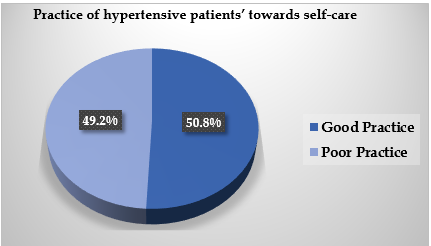
Figure 3 level of practice towards recommended self-care among adult hypertensive patients attending follow-up clinic at Asella referral and teaching hospital, Ethiopia, 2021. [n = 120]
Factors associated with knowledge towards recommended self-care
Age, gender, marital status, educational level, occupation, average monthly income, duration since diagnosis, residency, presence of comorbidities, and receiving information about self-care from healthcare providers during follow-up were entered into both bivariable and multivariable logistic regression analyses to identify factors significantly associated with knowledge towards recommended self-care. However, only educational level and receiving information about self-care were factors significantly associated with knowledge towards hypertension recommended self-care.
The odds ratio of having good knowledge towards recommended self-care among hypertensive patients who attended formal education was 3.615 times [AOR=3.615, 95%CI (1.262, 10.352), p=0.017] higher than their contraries. The likelihood of having good knowledge towards recommended self-care among hypertensive patients who were received information about hypertension self-care from healthcare providers during follow-up was 3.307 times [AOR=3.307, 95%CI (1.226, 8.926), p=0.018] higher than those hypertensive patients who were not received information about self-care from healthcare providers during follow-up. (Table 2)
|
Variable |
Category |
Knowledge |
COR [95%CI] |
AOR [95%CI] |
p-value |
|
|
Good |
Poor |
|||||
|
Age |
19-39 years |
18(51.4%) |
17(48.6%) |
1 |
1 |
|
|
40-59 years |
30(60%) |
20(40%) |
1.417(0.593,3.387) |
1.08(0.327,3.173) |
0.975 |
|
|
≥60 years |
24(68.6%) |
11(31.4%) |
2.061(0.778,5.458) |
1.333(0.294,6.052) |
0.709 |
|
|
Gender |
Male |
46(66.7%) |
23(33.3%) |
1.923(0.915,4.042) |
1.845(0.747,4.554) |
0.184 |
|
Female |
26(51%) |
25(49%) |
1 |
1 |
|
|
|
Marital Status
|
Unmarried |
8(42.1%) |
11(57.9%) |
1 |
1 |
|
|
Married |
64(63.4%) |
37(36.6%) |
2.378(0.878,6.443) |
3.73(0.96,14.495) |
0.057 |
|
|
Educational level |
No formal education |
15(45.5%) |
18(54.5%) |
1 |
1 |
|
|
Formal education |
57(65.5%) |
30(34.5%) |
2.28(1.009,5.153) |
3.615(1.262,10.352) |
0.017 |
|
|
Occupation
|
Employed |
22(68.8%) |
10(31.3%) |
1.672(0.709,3.944) |
1.014(0.341,3.017) |
0.980 |
|
Unemployed |
50(56.8%) |
38(43.2%) |
1 |
1 |
|
|
|
Average monthly income |
≤2500 ETB |
31(53.4%) |
27(46.6%) |
1 |
1 |
|
|
>2500 ETB |
41(66.1%) |
21(33.9%) |
1.7(0.814,3.553) |
1.036(0.405,2.649) |
0.941 |
|
|
Duration of the disease |
≤5 years |
48(57.8%) |
35(42.2%) |
1 |
1 |
|
|
>5 years |
24(64.9%) |
13(35.1%) |
1.346(0.603,3.006) |
0.876(0.256,2.996) |
0.833 |
|
|
Residency |
Urban |
41(60.3%) |
27(39.7%) |
1.029(0.492,2.149) |
0.576(0.216,1.537) |
0.271 |
|
Rural |
31(59.6%) |
21(40.4%) |
1 |
1 |
|
|
|
Presence of co-morbidities |
Yes |
24(61.5%) |
15(38.5%) |
1.1(0.503,2.406) |
0.931(0.354,2.448) |
0.884 |
|
No |
48(59.3%) |
33(40.7%) |
1 |
1 |
|
|
|
Receiving information about self-care from healthcare providers during follow-up |
Yes |
60(64.5%) |
33(35.5%) |
2.273(0.952,5.424) |
3.307(1.226,8.926) |
0.018 |
|
No |
12(44.4%) |
15(55.6%) |
1 |
1 |
|
|
Table 2 Bivariable and multivariable logistic regression analysis of factors associated with knowledge towards hypertension recommended self-care among adult hypertensive patients attending follow-up clinic at Asella referral and teaching hospital, Ethiopia, 2021. [n = 120]
Factors associated with attitude of towards recommended self-care
Age, gender, marital status, educational level, occupation, average monthly income, duration since diagnosis, residency, presence of comorbidities, receiving information about self-care from healthcare providers during follow-up and Knowledge towards self-care were entered into both bivariable and multivariable logistic regression analyses to identify factors significantly associated with attitude towards hypertension recommended self-care. However, only Knowledge towards self-care was factors significantly associated with attitude towards hypertension recommended self-care.
The likelihood of having favorable attitude towards self-care among hypertensive patients who had good knowledge towards self-care was 13.449 times [AOR=13.449, 95%CI (4.794, 37.728), p=0.000] higher than those hypertensive patients who had poor knowledge towards self-care. (Table 3)
|
Variable |
Category |
Attitude |
COR [95%CI] |
AOR [95%CI] |
p-value |
|
|
Positive |
Negative |
|||||
|
Age |
19-39 years |
18(51.4%) |
17(48.6%) |
1 |
1 |
|
|
40-59 years |
27(54%) |
23(46%) |
1.109(0.467,2.634) |
.701(0.190,2.587) |
0.594 |
|
|
≥60 years |
18(51.4%) |
17(48.6%) |
1.000(0.392,2.553) |
.779(0.139,4.357) |
0.776 |
|
|
Gender |
Male |
41(59.4%) |
28(40.6%) |
1.93(0.927,4.019) |
1.758(0.646,4.783) |
0.269 |
|
Female |
22(43.1%) |
29(56.9%) |
1 |
1 |
|
|
|
Marital Status
|
Unmarried |
9(47.4%) |
10(52.6%) |
1 |
1 |
|
|
Married |
54(53.5%) |
47(46.5%) |
1.277(0.478,3.407) |
|
|
|
|
Educational level |
No formal education |
15(45.5%) |
18(54.5%) |
1 |
1 |
|
|
Formal education |
48(55.2%) |
39(44.8%) |
1.477(0.66,3.303) |
0.494(0.144,1.69) |
0.261 |
|
|
Occupation
|
Employed |
19(59.4%) |
13(40.6%) |
1.462(0.644,3.318) |
0.785(0.237,2.604) |
0.692 |
|
Unemployed |
44(50%) |
44(50%) |
1 |
1 |
|
|
|
Average monthly income |
≤2500 ETB |
26(44.8%) |
32(55.2%) |
1 |
1 |
|
|
>2500 ETB |
37(59.7%) |
25(40.3%) |
1.822(0.882,3.760) |
1.910(0.663,5.503) |
0.230 |
|
|
Duration of the disease |
≤5 years |
45(54.2%) |
38(45.8%) |
1.25(0.575,2.716) |
1.434(0.321,6.397) |
0.637 |
|
>5 years |
18(48.6%) |
19(51.4%) |
1 |
1 |
|
|
|
Residency |
Urban |
39(57.4%) |
29(42.6%) |
1.569(0.759,3.245) |
2.264(0.736,6.963) |
0.154 |
|
Rural |
24(46.2%) |
28(53.8%) |
1 |
1 |
|
|
|
Presence of co-morbidities |
Yes |
17(43.6%) |
22(56.4%) |
1 |
1 |
|
|
No |
46(56.8%) |
35(43.2%) |
1.701(0.787,3.676) |
2.549(0.873,7.446) |
0.087 |
|
|
Receiving information about self-care from HCP during follow-up |
Yes |
53(57%) |
40(43%) |
2.252(0.932,5.444) |
1.559(0.499,4.871) |
0.445 |
|
No |
10(37%) |
17(63%) |
1 |
|
|
|
|
Knowledge towards self-care |
Poor |
10(20.8%) |
38(79.2%) |
1 |
|
|
|
Good |
53(73.6%) |
19(26.4%) |
10.6(4.433,25.345) |
13.449(4.794, 37.728) |
0.000 |
|
Table 3 Bivariable and multivariable logistic regression analysis of factors associated with Attitude towards hypertension recommended self-care among adult hypertensive patients attending follow-up clinic at Asella referral and teaching hospital, Ethiopia, 2021. [n=120]
Factors associated with practice towards recommended self-care
Age, gender, marital status, educational level, occupation, average monthly income, duration since diagnosis, residency, presence of comorbidities, receiving information about self-care from healthcare providers during follow-up, knowledge towards self-care and attitude towards self-care were entered into both bivariable and multivariable logistic regression analyses to identify factors significantly associated with practice towards hypertension recommended self-care. However, only receiving information about self-care from healthcare providers during follow-up, knowledge towards self-care, and Attitude towards self-care were factors significantly associated with practice towards hypertension recommended self-care.
The odds ratio of having good practice towards self-care among hypertensive patients who received information about self-care from healthcare providers during follow-up was 3.887 times [AOR=3.887, 95%CI (1.232,12.261), p=0.021] higher than those hypertensive patients who didn’t receive information about self-care from healthcare providers during follow-up. The likelihood of having good practice towards self-care among hypertensive patients who had good Knowledge towards self-care was 3.195 times [AOR=3.195, 95%CI (1.161,8.794), p=0.025] higher than those hypertensive patients who had poor knowledge towards self-care.
Furthermore, those hypertensive patients who had a favorable Attitude towards self-care were was 3.093 times [AOR=3.093, 95%CI (1.198,7.990), p=0.020] more likely to have good practice than those hypertensive patients who had an unfavorable attitude towards self-care. (Table 4)
|
Variable |
Category |
Practice |
COR [95%CI] |
AOR [95%CI] |
p-value |
|
|
Good |
Poor |
|||||
|
Age |
19-39 years |
15(42.9%) |
20(57.1%) |
1 |
1 |
|
|
40-59 years |
27(54%) |
23(46%) |
1.565(0.656,3.737) |
2.502(0.725,8.643) |
0.147 |
|
|
≥60 years |
19(54.3%) |
16(45.7%) |
1.583(0.616,4.068) |
3.313(0.624,17.602) |
0.160 |
|
|
Gender |
Male |
38(55.1%) |
31(44.9%) |
1.492(0.721,3.089) |
0.856(0.328,2.233) |
0.751 |
|
Female |
23(45.1%) |
28(54.8%) |
1 |
1 |
|
|
|
Marital Status
|
Unmarried |
9(47.4%) |
10(52.6%) |
1 |
1 |
|
|
Married |
52(51.5%) |
49(48.5%) |
1.179(0.442,3.146) |
0.601(0.143,2.533) |
0.488 |
|
|
Educational level |
No formal education |
15(45.5%) |
18(54.5%) |
1 |
1 |
|
|
Formal education |
46(52.9%) |
41(47.1%) |
1.346(0.602,3.009) |
0.993(0.319,3.091) |
0.990 |
|
|
Occupation
|
Employed |
17(53.1%) |
15(46.9%) |
1.133(0.504,2.549) |
0.518(0.163,1.644) |
0.265 |
|
Unemployed |
44(50%) |
44(50%) |
1 |
1 |
|
|
|
Average monthly income |
≤2500 ETB |
25(43.1%) |
33(56.9%) |
1 |
1 |
|
|
>2500 ETB |
36(58.1%) |
26(41.9%) |
1.828(0.886,3.771) |
1.748(0.626,4.877) |
0.286 |
|
|
Duration of the disease |
≤5 years |
42(50.6%) |
41(49.4%) |
1 |
1 |
|
|
>5 years |
19(51.4%) |
18(48.6%) |
1.030(0.475,2.237) |
0.600(0.147,2.454) |
0.477 |
|
|
Residency |
Urban |
37(54.4%) |
31(45.6%) |
1.392(0.675,2.874) |
1.352(0.477,3.834) |
0.571 |
|
Rural |
24(46.2%) |
28(53.8%) |
1 |
1 |
|
|
|
Presence of co-morbidities |
Yes |
19(48.7%) |
20(51.3%) |
1 |
1 |
|
|
No |
42(51.9%) |
39(48.1%) |
1.134(0.528,2.435) |
1.108(0.400,3.074) |
0.844 |
|
|
Receiving information about self-care from healthcare providers during follow-up |
Yes |
54(58.1%) |
39(41.9%) |
3.956(1.524,10.272) |
3.887(1.232,12.261) |
0.021 |
|
No |
7(25.9%) |
20(74.1%) |
1 |
1 |
|
|
|
Knowledge towards self-care |
Poor |
13(27.1%) |
35(72.9%) |
1 |
1 |
|
|
Good |
48(66.7%) |
24(33.3%) |
5.385(2.411,12.024) |
3.195(1.161,8.794) |
0.025 |
|
|
Attitude towards self-care |
Unfavorable |
17(29.8%) |
40(70.2%) |
1 |
1 |
|
|
Favorable |
44(69.8%) |
19(30.2%) |
5.449(2.493,11.910) |
3.093(1.198,7.990) |
0.020 |
|
Table 4: Bivariable and multivariable logistic regression analysis of factors associated with Practice towards recommended self-care among adult hypertensive patients attending follow-up clinic at Asella referral and teaching hospital, Ethiopia, 2021. [n=120]
Hypertension remains one of the most important public health problems worldwide because of the associated morbidity, mortality, and cost to society. Hypertension is still insufficiently controlled in a large number of patients globally, despite the availability of safe and effective antihypertensive medications and the existence of clear treatment guidelines.32 A quasi-experimental study done in Mansoura University Hospital, Egypt, on the lifestyle intervention program was found to be effective in the control of BP, which was via the adoption of healthy behaviors.33 This study was proposed to determine hypertension recommended self-care knowledge, attitude, practice, and its predictors among hypertensive patients on follow-up clinic at Asella Referral and Teaching Hospital, Ethiopia.
The hypertensive patients’ level of good knowledge towards self-care was 60.0% [n=72, 95%CI; 51.7, 70]. This study finding was lower when compared with a study conducted in Harar, Ethiopia, 73.0%,29 and Nekemte specialized hospital, Ethiopia, 79.28%.34 The variation might be because of the differences in sociodemographic characteristics of the study participants, sample size, and the tools used.
The odds ratio of having good knowledge towards self-care among hypertensive patients who attended formal education was 3.615 times [AOR=3.615, 95%CI (1.262, 10.352), p=0.017] higher than their contraries. This study finding was supported by the study done in Harar, Ethiopia.29 In fact, education is a power of personal change. In the context of this concept, as the individual updates himself/herself, they will be more knowledgeable of it. This study finding was supported by the study done on the effect of educational programs on hypertension management toward knowledge in hypertensive patients in Indonesia. This quasi-experimental study revealed that health education could improve hypertension management knowledge among uncontrolled hypertension.353 This was also supported by a study conducted in Isunjaba, Nigeria, which showed that there was marked improvement in knowledge of hypertension control after community health nursing intervention.36
The likelihood of having good knowledge towards self-care among hypertensive patients who were received information about self-care from healthcare providers during follow-up was 3.307 times [AOR=3.307, 95%CI (1.226, 8.926), p=0.018] higher than those hypertensive patients who were not received information about self-care from healthcare providers during follow-up. This might be due to having information about self-care would make them more knowledgeable about this issue. This is also supported by a clinical trial study conducted in Iran, which investigates the effect of training on knowledge in patients with hypertension. This study found that a training program was effective in improving the practice of hypertensive patients.37
The hypertensive patients’ level of favorable attitude towards recommended self-care was 52.5% [n=63, 95%CI; 44.2, 61.6]. This study finding was consistent when compared with a study conducted in Nepal 50.7%.26 However, this study finding was lower when compared with a study conducted in Harar, Ethiopia (66.4%),29 and Ahoe-Ho, Ghana (92.2%).38 The variation might be because of the differences in sociodemographic characteristics of the study participants, sample size, and the tools used.
The likelihood of having a favorable attitude towards self-care among hypertensive patients who had good knowledge towards self-care was 13.449 times [AOR=13.449, 95%CI (4.794, 37.728), p=0.000] higher than those hypertensive patients who had poor knowledge towards self-care. The possible justification could be that knowledge would play a vital role in altering the attitude of the individuals. This was supported by a clinical trial study conducted in Iran, which investigated the effect of training on attitude in patients with hypertension. This study found that a training program was effective in improving the attitude of hypertensive patients.37 This study finding was also supported by the study done on the effect of educational programs on hypertension management toward knowledge in hypertensive patients in Indonesia. This quasi-experimental study revealed that health education could improve hypertension management attitude among uncontrolled hypertension.35 This was also supported by a study conducted in Isunjaba, Nigeria, which showed that there was marked improvement in attitude towards hypertension control after community health nursing intervention.36
The hypertensive patients’ level of practice towards recommended self-care was 50.8% [n=61, 95%CI; 43.4, 58.3]. This study finding was consistent when compared with a study conducted in Harar, Ethiopia, (49.6%),29 (52.2%) Nepal,39 Dessie town, Ethiopia (49%),31 and Debre Tabor, Ethiopia, 54.1%.40 This study finding was lower when compared with a study conducted in Nekemte specialized hospital, Ethiopia, 68.92%,34 and Gondar, Ethiopia, 59.4%.41 However, this study finding was higher than a study done in SNNPR, Ethiopia, (27.3%),42 and Mizan Tepi University Teaching Hospital, Ethiopia, (33.3%).30 The variation might be because of the differences in sociodemographic characteristics of the study participants, sample size, and the tools used.
The odds ratio of having good practice towards self-care among hypertensive patients who received information about self-care from healthcare providers during follow-up was 3.887 times [AOR=3.887, 95%CI (1.232,12.261), p=0.021 higher than those hypertensive patients who didn’t receive information about self-care from healthcare providers during follow-up. This was supported by the study done in Mizan Tepi University Teaching Hospital, Ethiopia,30 and Desse town, Ethiopia.31
The likelihood of having good practice towards self-care among hypertensive patients who had good knowledge towards self-care was 3.195 times [AOR=3.195, 95%CI (1.161,8.794), p=0.025] higher than those hypertensive patients who had poor knowledge towards self-care. This was supported by the study done in Debre Tabor, Ethiopia.40 This is also supported by a clinical trial study conducted in Iran, which investigates the effect of training on practice in patients with hypertension. This study found that a training program was effective in improving the practice of hypertensive patients.37
This was also supported by a study conducted in Isunjaba, Nigeria, which showed that there was marked improvement in lifestyle relating to hypertension control after community health nursing intervention.36 Those hypertensive patients who had a favorable attitude towards self-care were 3.093 times [AOR=3.093, 95%CI (1.198,7.990), p=0.020] more likely to have good practice than those hypertensive patients who had an unfavorable attitude towards self-care. This was supported by the study done in Harar, Ethiopia,29 and Nepal.39 Despite this topic being vital, there are limitations of the studies about hypertension recommended self-care knowledge, attitude, practice, and its predictors among hypertensive patients on follow-up clinic in the study area. Nevertheless, this study would support being a baseline for the researchers who will conduct the study on the same topic.
The findings of this study revealed that the level of good knowledge, favorable attitude, and good practice towards self-care was 60.0%, 52.5%, and 50.8%, respectively. Educational level and receiving information about self-care from healthcare providers during follow-up were factors significantly associated with knowledge towards self-care. Having good knowledge towards self-care was significantly associated with attitude towards self-care. Whereas, receiving information about self-care from healthcare providers during follow-up, having good knowledge towards self-care, and having a favorable attitude towards self-care were factors significantly associated with self-care practice.
This study gives substantial evidence for a public health issue consideration. Understanding the hypertensive patients’ level of knowledge, attitude, practice, and associated factors towards recommended self-care would be a foundation to manage and control the morbidity and mortality associated with uncontrolled hypertension. Moreover, the result of this study also offers significant assistance to the healthcare providers to consider these issues during the follow-up care of the hypertensive patients as a self-management strategy. This is because hypertensive self-care has a crucial role in preventing the complications associated with uncontrolled hypertension. Lastly, we recommend that programs such as health education programs about hypertension self-care are needed to take place to improve the knowledge, attitude, and practice of the patients towards hypertension recommended self-care.
Ethical clearance was obtained from the nursing department, College of Health Sciences, Arsi University. Then, a letter of permission was sent to Asella Referral and Teaching Hospital for permission. The patients were informed regarding the significance of a study. Besides, they were assured about the confidentiality issues prior to data collection. Finally, the written informed consent was obtained from the patients.
The authors would like to thank Asella Referral and Teaching Hospital, patients, data collectors, and Arsi University for their cooperation. This manuscript is posted as a preprint on Research Square:43 https://assets.researchsquare.com/files/rs-2900667/v1/02ed4175-2841-48f3-84c6-272ecc97429d.pdf?c=1683581689.
All data supporting the findings are available in the manuscript .
Not applicable.
The authors received no financial support for this study.
The authors has contributed to the conception of the study, data analysis, drafting or revising the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
The authors declared no potential conflicts of interest with this work.

©2024 Gebreyohannes, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.