Journal of
eISSN: 2373-6437


Research Article Volume 1 Issue 4
1Department of Pediatrics, Cairo University, Egypt
2Department of Community Medicine, Cairo University, Egypt
Correspondence: Hanaa I Rady, Department of Pediatrics, Cairo University, Gameat el Doual Al Arabia Street, Mohandessin, Egypt, Tel +201001482444, Fax 0020233473960
Received: September 08, 2014 | Published: October 14, 2014
Citation: Rady HI, Emil A, Samy K, Baher S (2014) Prediction of Stress Related Gastrointestinal Bleeding in Critically III Children Using PRISM III Score. J Anesth Crit Care Open Access 1(4): 00023. DOI: 10.15406/jaccoa.2014.01.00023
Background: Stress -induced ulcer bleeding is one of the common complications in critically ill patients admitted to the intensive care unit. The PRISM (Pediatric Risk of Mortality) scoring systems can assess the severity of disease in a given population of sick children.
Aim: To set a cut off level of PRISM III score which can predict that at this point stress ulcer had occurred, and at this cut off level prophylactic treatment can be justified without appearance of fresh bleeding.
Methodology: One-hundred and Thirty-five Egyptian children, admitted in PICU of El Mounira Children hospital, Cairo University, with variable critically illness were included. PRISM III score was calculated for each child within 24 hours from admission with surveillance of patients who developed upper GIT bleeding during PICU stay.
Results: Overall mortality rate was 40%. The mean score of PRISM-III for total 135 PICU admissions was 6.02±5.48 (score range: 0-28). Thirty-nine (28.9%) of our cases had developed GIT bleeding, compared to 96 (71.1%) patients without bleeding. Mechanical ventilation was significantly associated with stress ulcer bleeding (P<0.0001). The cut-off point of 7 of PRISM III score has highest sensitivity and specificity as a better predictor of GIT bleeding. Among patients with PRISM III score less than 7; 91.5% had no GIT bleeding while 60% of cases with PRISM III score ≥ 7 had GIT bleeding, p < 0.0001.
Conclusion: At PRISM III score value ≥7, even if no clinical GIT bleeding, prophylactic treatment is justified.
Keywords: GIT bleeding, PRISM score, Intensive care, Stress ulcer
PRISM, Pediatric Risk of Mortality; GI, Gastrointestinal; ICU, Intensive Care Unit; PICU, Pediatric Intensive Care Unit; PRISM, Pediatric Risk of Mortality
Stress related gastrointestinal (GI) bleeding is one of the common complications in critically ill patients.1 In pediatric patients, the prevalence of GI bleeding ranges from 6 to 25%, with life threatening bleeding rarely seen.2,3 Within the first 24 hours after intensive care unit (ICU) admission, approximately 75% to 100% of critically ill patients admitted with thermal injuries or after major surgical intervention, have some endoscopic evidence of gastro-duodenal or upper GI lesions.4
For this reason, critically ill patients in the ICU may benefit from stress ulcer prophylaxis,5 but, it has been associated with major complications, such as hospital-acquired pneumonia with colonization of the gut due to decreased stomach acidity.6 The scoring systems that have been developed as scales for evaluation of ICUs’ function are helpful tools assisting basic decision making and further planning for progression.7 In any given pediatric ICU (PICU), there is a close correlation between PRISM III (Pediatric Risk of Mortality) score, the number of patients’ impaired organ systems during the first 12-24 h of admission and risk of mortality.8,9
The aim of this study was to set a cut off level of PRISM score which can predict that at this point stress ulcer had occurred, and at this PRISM value, prophylactic treatment can be justified before the appearance of frank bleeding.
A prospective cohort analytic study was done on all critically ill children admitted to the PICU of El Mounira Children hospital, Cairo University, over a period of 6 months from June 2012 to November 2012.
III. Calculating the PRISM III score for each child upon admission (Table 1).10
|
Variable |
Age Restrictions |
Score |
|||||||
|
Systolic blood pressure (mmHg) |
Neonate |
Infant |
Child |
Adolescent |
|
||||
|
40-55 |
45-65 |
55-75 |
65-85 |
3 |
|||||
|
<40 |
<45 |
<55 |
<65 |
7 |
|||||
|
Temperature |
All ages <33°C or >40°C |
3 |
|||||||
|
Mental status |
All ages: stupor or coma (GCS <8) |
5 |
|||||||
|
Heart rate |
Neonate |
Infant |
Child |
Adolescent |
|
||||
|
215-225 |
215-225 |
185-205 |
145-155 |
3 |
|||||
|
>225 |
>225 |
>205 |
>155 |
4 |
|||||
|
Pupillary reflexes |
All ages = One pupil fixed, pupil >3mm 7 All ages = Both fixed, pupil >3mm |
7 11 |
|||||||
|
Acidosis (pH) or total CO2 (mmol/L) |
All ages = pH 7.0-7.28 or total CO2 5-16.9 2 All ages = pH <7.0 or total CO2 <5 |
2 6 |
|||||||
|
pH |
All ages = 7.48-7.55 2 All ages >7.55 |
2 3 |
|||||||
|
PCO2 (mmHg) |
All ages = 50.0-75.0 1 All ages >75.0 |
1 3 |
|||||||
|
Total CO2 (mmol/L) |
All ages >34.0 |
4 |
|||||||
|
Arterial PaO2 (mmHg) |
All ages = 42.0-49.9 3 All ages <42.0 |
3 6 |
|||||||
|
Glucose |
All ages >11.0 mmol/L |
2 |
|||||||
|
Potassium |
All ages >6.9 mmol/L |
3 |
|||||||
|
Creatinine (mmol/L) |
Neonate |
Infant |
Child |
Adolescent |
|
||||
|
>75 |
>80 |
>80 |
>115 |
2 |
|||||
|
Urea (mmol/L) |
Neonate |
All other ages |
|
||||||
|
>4.3 |
>5.4 |
3 |
|||||||
|
White blood cells |
All ages < 3000 cells/mm3 |
4 |
|||||||
|
Prothrombin time (PT) or partial thromboplastin time (PTT) |
Neonate |
All other ages |
|
||||||
|
PT >22.0 sec or PTT >85.0 |
PT >22.0 sec or PTT >57.0 sec |
3 |
|||||||
|
Platelets (cells/mm3) |
All ages = 100,000 to 200,000 2 All ages = 50,000 to 99,999 4 <50,000 |
2 4 5 |
|||||||
Table 1 Pediatric risk of mortality score III.10
Blood samples were taken from the patients using wide-bore needle and withdrawn slowly from antecubital vein to avoid hemolysis of RBCs by careful venepuncture. These samples were divided into 3 aliquots, first aliquot was added to heparin tube for ABG measurements, second aliquot was added to EDTA tube for CBC counts and the third aliquot was added to a dry tube, allowed to be clotted for 30 minutes, and then separated by centrifugation at 4000 rpm for 5 minutes for measurements of serum glucose level, serum potassium level, serum creatinine level and blood urea nitrogen level.
Analysis of data was done by using SPSS (statistical program for social science version 15) as follows:
a) Description of quantitative variables as mean, SD and range
b) Description of qualitative variables as number and percentage
c) Unpaired t-test was used to compare two groups as regard quantitative variable in parametric data (SD<25% mean)
d) Mann Whitney Willcoxon test was used to compare two groups as regard non parametric data (SD>50% Mean)
This study was done on 135 Egyptian children [77 males (57%) and 58 females (43%)] admitted in PICU of El Mounira Children hospital, Cairo University, with variable critical illness. Their mean age was 26.44±20.86 months and the mean of their PRISM-III score was 6.02±5.48 (score range: 0-28). Table 2 showed that the frequancy of males was higher than females; respiratory problems (46.67%) represented the major indication for ICU admission and the mortality rate was 40%.
Characteristics Studied Cases (n=135) |
n (%) |
|
Gender |
Male |
77 (57.0) |
Female |
58 (43.0) |
|
Respiratory Support |
Not ventilated |
80 (59.3) |
Ventilated |
55 (40.7) |
|
GIT Bleeding |
No bleeding |
96 (71.1) |
Coffee ground |
22 (16.3) |
|
Hematemesis |
17 (12.6) |
|
Outcome |
Discharged |
81 (60.0) |
Died |
54 (40.0) |
|
Diagnosis-Related Groups |
Respiratory System |
63 (46.67) |
Central Nervous System |
39 (28.89) |
|
Cardiovascular System |
26 (19.26) |
|
Metabolic and electrolytes disturbance |
3 (2.22) |
|
Renal System |
2 (1.48) |
|
Gastrointestinal System |
2 (1.48) |
|
Table 2 Characteristics of children included in this study
Ninety six (71.1%) of admitted cases had no GIT bleeding, 22(16.3%) had coffee-ground colored bleeding and 17(12.6%) had fresh hematemesis. Thirty nine (28.9%) patients had GIT bleeding, compared to 96 (71.1%) patients without bleeding. GIT bleeding was more common among patients on mechanical ventilation (32 of mechanically ventilated cases had GIT bleeding vs 23 didn’t have GIT bleeding, P<0.0001). Mortality rate was significantly higher in the groups of children who developed gastrointestinal bleeding (P<0.0001). Although males (64.1%) were more affected with GIT bleeding than females (35.9%); it was statistically insignificant (p=0.422). Table 3 showed that PRISM III score cut-off value of (7) in relation to GIT bleeding had a sensitivity (82.05%) and specificity (86.46%), p=0.0001; with area under the curve (AUC) = 0.875 as shown in Figure 1.
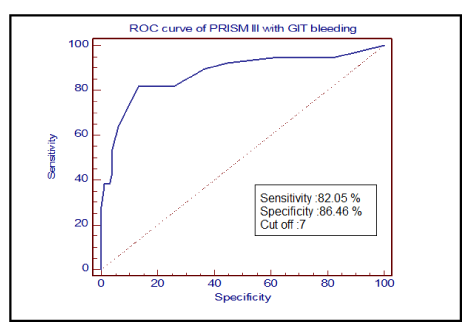
Figure 1 Showing PRISM III score and its relation to gastro-intestinal bleeding [Area under the curve (AUC) = 0.875].
PRISM |
Sensitivity |
Specificity |
±LR |
-LR |
Significance |
>2 |
94.87 |
38.54 |
1.54 |
0.13 |
0.0001 |
>4 |
89.74 |
63.54 |
2.46 |
0.16 |
|
>5 |
82.05 |
73.96 |
3.15 |
0.24 |
|
>7 * |
82.05 |
86.46 |
6.06 |
0.21 |
|
>8 |
64.10 |
93.75 |
10.26 |
0.38 |
|
>10 |
43.59 |
95.83 |
10.46 |
0.59 |
Table 3 PRISM III score in children with gastro-intestinal bleeding
PRISM III, Pediatric risk of mortality score III; +LR, Positive Likelihood Ratio; -LR, Negative likelihood ratio
Of the 135 studied cases, 82 patients had PRISM III score less than 7, only seven (8.5%) of them had GIT bleeding; while 53 patients had PRISM III score more than or equal 7; thirty two (60%) of them had GIT bleeding with statistically significant difference p < 0.0001 (Table 4). The mortality rate was 66% (35/53) in patient with PRISM III score more than or equal 7; compared to 23.2% (19/82) in patients with PRISM III score less than 7; p value < 0.0001 (Figure 2).
GIT Bleeding |
PRISM III Score < 7 |
PRISM III Score > 7 |
p Value |
No Bleeding |
75 (91.5 %) |
21 (39.6 %) |
<0.0001 |
Bleeding |
7 (8.5 %) |
32 (60.4 %) |
Table 4 PRISM III score and gastro-intestinal bleeding
PRISM III, Pediatric Risk of Mortality Score III
Our analytic study was done on 135 Egyptian children admitted in PICU of El Mounira Children hospital, Cairo University, with variable critical illness. The mean age of patients in this study was (26.44±20.86) months. The patients enrolled in the present study were younger than those in the original validation populations for PRISM III where the mean age of patients was ranged between 33 and 35 months.9,11,12 PRISM III scores have been studied extensively in more than one study.13‒17 By comparing our results with above mentioned studies it can be claimed that mortality rate of our PICU (40%) was close to these studies. They have mortality rates ranged from 35 to 38%.
Similar to our study, Aragao et al.18 observed that male patients had a higher risk of death than females. We found that GIT bleeding was more in mechanically ventilated cases and PRIM III cut-off value of ≥7 was related to the presence of GIT bleeding. A study by Chaïbou et al.19 found three independent risk factors for major upper gastrointestinal bleeding in critically ill children: respiratory failure, coagulopathy, and a pediatric risk of mortality (PRISM) score > 10. In agreement with our results, several studies have suggested that mechanical ventilation is one of the most significant of various probable risk factors for this condition.18
Similar to previous studies done in adults and children, the mechanical ventilation was the most significant risk factor for stress-induced gastrointestinal bleeding.5,19,20 In adults, the Blatchford risk score is a validated risk-stratification tool that can accurately identify patient risk using clinical and laboratory variables. The score ranges from 0 to 23. A score of 0 indentifies a low risk patient, while a score of 1 or above identifies a patient as high risk. Although externally validated, the Blatchford risk score is useful mostly in identifying low-risk patients because the high-risk category encompasses a wide range of scores (1-23).21
Moreover, the Rockall risk score can be used but it’s not validated in pediatric age group.22 We also found a high prevalence of overt upper gastrointestinal bleeding (28.9%), which is comparable to the retrospective report section from Kuusela et al.20 in neonates. The mortality rate was high (66%) in patient with PRISM III score ≥7 and (23.2%) only in patients with PRISM III score < 7 with; p value < 0.0001. In a study done by De Leon et al. [23] on 170 Mexican infants, the mean PRISM-III score and observed mortality rate in subgroups with PRISM-III ≥ 8 and < 8 were 52.2% and 24.7% respectively. These results are at the same direction as ours.
Also in agreement with our results, Tan et al.14 selected a cut-off point of 8 to be a better predictor of mortality. Analysis of the 2 groups PRISM III <8 and PRISM III ≥8, showed that there was a 15.8 times increased risk of mortality (95% CI: 2.0 to 127.8) in the latter group. While in Bellad et al.24 study, overall mortality was 16.7%. A cut off score of 15, was associated with 89.2% accuracy.
The cut-off value of PRISM III score 7 had highest sensitivity and specificity and can be used to predict GIT bleeding in PICU patients. At this PRISM III score value of ≥7 even if no clinical GIT bleeding, prophylactic treatment is justified.
None.
None.
Authors declare that there is no conflicts of interest.

©2014 Rady, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.