Journal of
eISSN: 2373-6437


Case Report Volume 16 Issue 5
1Anesthesiologist at various hospitals, Brazil
2Anesthesiologist at the National Cancer Institute (INCA), Brazil
3Head of the Anesthesiology Service of the National Cancer Institute (INCA) Anesthesiologist, Responsible for the CET-SBA of the National Cancer Institute, Brazil
4INCA Anesthesiologist, Co-Responsible for the CET-SBA of the National Cancer Institute, Brazil
5Professor of Anesthesiology at the UFG Faculty of Medicine, Responsible for the CET-SBA of the HCUFG, Brazil
6Master’s in environmental sciences and health, Universidade Goiás, Brazil
7Master’s in labor economics, UFPB, João Pessoa-PB, PhD student in applied mathematics and modeling, Brazil
Correspondence: Dr. Luiz Eduardo Imbelloni, Anesthesiologist at various hospitals, Av. Epitácio Pessoa, 2356/203, Lagoa, 22411-072- Rio de Janeiro, RJ, Brazil, Tel + 55.11.99429-3637
Received: October 18, 2024 | Published: October 31, 2024
Citation: Imbelloni LE, Rivoli ALC, Neto SVL, et al. Comparison of a fixed dose of 0.15% Hypobaric and 0.5% Hyperbaric Bupivacaine for short-term unilateral lower limb orthopedic surgeries. Retrospective study with two videos. J Anesth Crit Care Open Access. 2024;16(5):139-143. DOI: 10.15406/jaccoa.2024.16.00605
Background: Unilateral spinal anesthesia in orthopedic surgery of a limb has its advantages, especially in patients undergoing outpatient basis surgeries. Low dose, slow speed of administration and remaining in lateral decubitus for a certain period facilitate unilateral distribution in spinal anesthesia. Isobaric solutions of local anesthetics are not suitable for this type of anesthesia. Hypobaric and hyperbaric solutions of bupivacaine were compared in unilateral spinal anesthesia in patients undergoing orthopedic surgeries of one limb on an outpatient basis.
Methods: Retrospective study carried out between 2002 and 2020 with 497 patients were randomly divided into two groups to receive 6 mg of 0.15% hypobaric bupivacaine or 6 mg of 0.5% hyperbaric bupivacaine. The solutions were administered in the L3-L4 space with the patient in the left lateral decubitus and remaining in this position for 15 minutes. Sensitive anesthesia was evaluated by the pin prick test. Motor blockade was determined by the modified Bromage scale. Both blockades were compared with the opposite side and among themselves.
Results: There was a significant difference between the side of the surgery and the opposite side in all two groups at 15 minutes, but the frequency of unilateral spinal anesthesia was 90.9% with the 0.15% hypobaric bupivacaine versus 93.2% with the 0.5% hyperbaric bupivacaine. Patients did not develop any hemodynamic changes. Post puncture headache and transitory neurological symptoms were not observed.
Conclusion: Spinal anesthesia with hypobaric and hyperbaric solutions present a higher frequency of unilateral anesthesia, without cardiocirculatory alteration, and patient satisfaction in remaining with a limb without anesthesia.
Keywords: Anesthetics: Bupivacaine; Anesthetic Solutions: Hypobaric, Hyperbaric; Anesthetic Techniques, Regional: Unilateral Spinal Block; Surgery, Orthopedics.
In 1984, in an excellent editorial, the production of bupivacaine was requested in Brazil, which presented numerous advantages, both in hyperbaric and isobaric solutions.1 In 1989, we carried out the first study with the 0.5% bupivacaine solution with glucose to evaluate the cephalic dispersion with the change of the horizontal decubitus position to a 10% cephalic inclination.2 As early as 1991, we conducted the first study with 0.5% isobaric bupivacaine being influenced by age.3
However, in no other country in the world have hypobaric solutions of local anesthetics been standardized by the pharmaceutical industry. In Brazil the most used anesthetics in spinal anesthesia remain with lidocaine, bupivacaine, ropivacaine and enantiomeric excess of bupivacaine (S75:R25), and hypobaric solutions are obtained from isobaric through dilutions with distilled water,4 and their density and baricity were recently evaluated.5 On some occasions, we have had the opportunity to evaluate the anesthesia we use on our patients when they undergo surgery. Thus, our group was an advocate of isobaric solutions of various local anesthetics, due to their great cardiocirculatory stability for almost all surgeries. Until I underwent a right inguinal hernia repair that lasted 50 minutes, but I had motor blockade of the lower limbs for 5 hours, with apprehension about whether I would need a bladder catheter.6 At that moment, I realized that motor blockade was not a quality of spinal anesthesia, and we started to look at several other options and used isobaric solutions only with specific indication. Thus, in 2006 we tried to explain the understanding of spinal anesthesia and its various solutions,7 with other articles for the complete understanding of the various hypobaric, isobaric, hyperbaric solutions and various puncture positions and table position.8,9
In a study with 150 patients comparing low doses of 5 mg of 0.5% hyperbaric, 0.5% isobaric and 0.15% hypobaric bupivacaine for unilateral spinal anesthesia, it was shown that there was a significant difference between the operated and non-operated sides in all three groups at 20 minutes, but a higher frequency of unilateral spinal anesthesia was obtained with the hyperbaric and hypobaric bupivacaine solutions.10 Unilateral spinal anesthesia with hypobaric and hyperbaric solutions provided a higher frequency of unilaterality. The isobaric solution should not be used for hemi spinal anesthesia. Several hypobaric and hyperbaric local anesthetics have been used for obtaining unilateral spinal anesthesia.
The objective of this retrospective study, in the period between 2002 to 2020, all spinal anesthesia for orthopedic surgeries of a single lower limb and on an outpatient basis, subarachnoid puncture was performed always in the left lateral decubitus position and comparing two solutions at the same dose of 6 mg: 0.15% hypobaric bupivacaine if the procedure was on the upper limb (upward), and the 0.5% hyperbaric bupivacaine was on left lower limb (downward), remaining in this position for 15 minutes.
The study was registered in the Brazil Platform (CAAE: 09061312.1.0000.5179). The Ethics Research Committee approved the study protocol (Number: 171,924) and was a retrospective study carried out in several hospitals. All unilateral spinal anesthesia with bupivacaine for orthopedic surgery were recorded in an Excel spreadsheet for further study. From 2002 to 2020, 530 spinal anesthesia’s were recorded 0.15% hypobaric and 0.5% hyperbaric bupivacaine according to the consort flowchart (Figure 1). Because the study was retrospective, the Free and Informed Consent Term was released, and all patients signed the authorization form for future publication. The density (g/ml) of 0.15% hypobaric and 0.5% hyperbaric bupivacaine solutions at 37oC was measured using a DMA 450 densimeter. All patients eligible for short-term orthopedic surgery were offered as the first option to spinal anesthesia with hypobaric bupivacaine solution compared with hyperbaric bupivacaine, at a fixed dose of 6 mg. We studied 530 patients over 18 years of age and under 80 years of age undergoing various orthopedic procedures below the knee, ASA physical status I, II, III of both genders. Inclusion criteria were normal blood volume, no pre-existing neurological disease, no coagulation disorders, without infection at the puncture site, which did not present agitation, mental confusion and/or delirium, did not make use of bladder indwelling catheters, with hemoglobin level >10 g%, who were not in the ICU, use of a pneumatic tourniquet, puncture with a 27G Quincke needle, puncture in left lateral decubitus (Figure 2). Exclusion criteria were lack of data in the spreadsheet, not using a tourniquet, under 18 years of age and injection of 7.5 mg of bupivacaine.
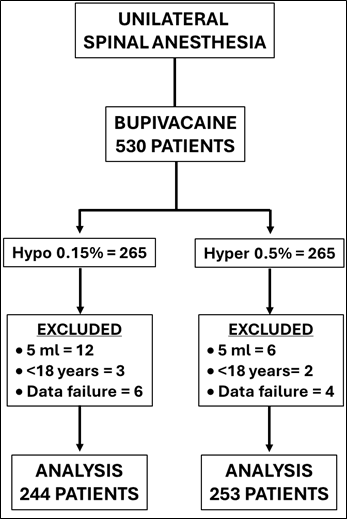
Figure 1 Consort flowchart 530 unilateral spinal anesthesia with both bupivacaine, performed between 2002 to 2020.
All patients received a pre-anesthetic visit by the anesthesiologist and the entire procedure was informed, but no pre-anesthetic medication was administered either orally or by muscle. An 20G catheter was inserted in the left hand for hydration and administration of drugs. The monitoring used in all patients was ECG continuously in the CM5 lead, non-invasive blood pressure, oxygen saturation and expired CO2 through the capnograph placed in the nose, and all data were recorded at 5-minute intervals until the incision and afterwards every 10 minutes. After monitoring was installed, patients received 1 mg of midazolam and 50 µg of fentanyl for placement in the left lateral decubitus for lumbar puncture, and the study covered two groups: upper limb surgery hypobaric group and lower limb surgery hyperbaric group with a fixed dose of 6 mg.
After asepsis and antisepsis with 70% alcohol or 0.5% alcohol chlorhexidine, the patients were placed in left lateral decubitus. Local anesthesia was performed with 1 ml of 1% lidocaine using a syringe and insulin needle, followed by 2 ml of the same solution using a 27G needle to introduce the spinal anesthesia needle. We performed a puncture of the subarachnoid space through a median or paramedian with a 27G cut needle without introducer between the L3-L4 interspaces. Free flow of CSF confirmed the position of the needle into the subarachnoid space, 6 mg (4 ml) of 0.15% hypobaric or 6 mg (1.2 ml) hyperbaric bupivacaine were injected. The solutions were injected at a rate of 1 ml/15 seconds with the hypobaric solution (Video 1) and 1 ml/30 seconds with the hyperbaric solution (Video 2), remaining in this position for 15 minutes. After this time, the patients were placed in a supine position to perform the surgery, and evaluate the parameters proposed in the study.
Video 1 Unilateral spinal anesthesia with 0.15% hypobaric bupivacaine.
Video 2 Unilateral spinal anesthesia with 0.5% hyperbaric bupivacaine.
The latency was defined as the time to the first loss of sensitivity in the L1 metamer in operated lower limb. The segmental level of analgesia (loss of needle prick sensation) was determined in the operated limb and in the contralateral (non-operated) limb at a one-minute interval at the beginning and every five minutes until 15 minutes. Motor block was assessed 15 minutes before the start of surgery by modified Bromage scale: 0 = free movement of the lower limbs, 1 = inability to raise the extended limbs, 2 = inability to flex knees, 3 = inability to move the ankle in the operated limb and in the contralateral limb. The duration of analgesia was considered as the return of sensitivity and motor block in the dermatome corresponding to L1.
Hypotension was defined as a decrease of more than 30% from the baseline systolic arterial blood pressure and treated with IV boluses of 2 mg ethilephryne. Bradycardia was defined as heart rate <50 bpm (beat per minute) and treated with atropine 0.50 mg. The numbers of hypotensive and bradycardic episodes were recorded. Anxiety was treated with midazolam 1 mg.
Postoperative analgesia was performed using lumbosacral plexus, depending on the innervation of interest to the surgical procedure. All blocks were performed with an HNS12 neurostimulator with A50, A100 or A150 needles depending on the depth of the plexus. After desired contraction to plexus stimulation, all blocks were injected with 0.25% enantiomeric excess levobupivacaine (S75:R25) at a dose of 30 to 40 ml, and the duration of analgesia was evaluated. During the study the hospital did not have an ultrasound device for performing peripheral nerve blocks.
Analgesia was performed via the veins with ketoprofen 100 mg every 8 hours and dipyrone 40 m/kg every 4 hours. Other postoperative events potentially related to either the surgical or anesthetic procedure, i.e., discomfort, nausea and vomiting, urinary retention, pruritus, headache, or other neurologic sequelae, were also recorded. All patients were followed before hospital discharge and on the 2nd and 3rd postoperatively up by telephone to check for neurological complications, and special attention to transient neurologic symptoms (TNS), and if any, it was correlated with the type of surgery.
The results were analyzed using non-parametric Fisher exact test and Mann-Whitney, with a p value<0.05 considered significant. The Mann-Whitney test is a non-parametric statistical test used to compare two independent samples and determine whether they come from populations with the same distribution. Fisher's Exact Test is a statistical test used to determine if there are nonrandom associations between two categorical variables, particularly in small sample sizes.
Demographic characteristics showed that there was no significant difference between the two groups (Table 1). The onset of blockade installation, duration of surgery and blockade (sensory and motor) were similar regardless of the hypobaric or hyperbaric bupivacaine solution, showing that the difference in volume did not alter any of the data evaluated (Table 2). The sensory and motor block assessments at 15 minutes and at the end of surgery in the operated and contralateral limb were practically the same with no significant difference (Figure 3). The dispersion of sensory blockade with 0.15% hypobaric bupivacaine in the operated limb ranged from L1 to T8, with the mode being T12. In the contralateral limb, at 15 minutes, 22 patients presented sensory blockade that ranged from L4 to L1. The dispersion of sensory blockade with 0.5% hyperbaric bupivacaine in the operated limb ranged from L1 to T8, with the mode being T12. In the contralateral limb, at 15 minutes, 17 patients presented sensory blockade that ranged from L4 to L1. At the end of surgery in the operated limb, regression was from L1 to L4 and 7 patients without any blockade with 0.15% hypobaric bupivacaine, and regression with 0.5% hyperbaric was from L1 to L4 and 10 patients without any blockade. At the end of surgery in the contralateral limb, no patient in either group presented any degree of sensory or motor blockade.
|
Data |
Bupivacaine 0.15% Hypobaric = 244 |
Bupivacaine 0.5% Hyperbaric = 253 |
Value P |
|
Age (yr) (Limits) |
39.79 ± 12.88 (18 – 80) |
39.16 ± 12.28 (18 – 80) |
0.001107 * |
|
Weight (kg) (Limits) |
67.57 ± 13.78 (43 – 100) |
70.78 ± 11.90 (43 – 97) |
0.0003724 * |
|
Height (cm) (Limits) |
165.10 ± 8.22 (149 – 195) |
168.72 ± 8.39 (150 – 193) |
0.000006343 * |
|
Gender: M / F |
112 / 132 |
149 / 104 |
0.4075 ** |
Table 1 Patient demographics data
* Mann-Whitney Test ** Exact Fisher Test
Is there no difference in degrees 2 and 3 of motor block in the operated limb (Table 2). The dose of 6 mg of 0.15% hypobaric bupivacaine and 0.5% hyperbaric bupivacaine for unilateral spinal anesthesia allowed excellent cardiocirculatory stability, as none of the 497 patients undergoing unilateral lower limb surgery required treatment for arterial hypotension or bradycardia.
|
Data |
Bupivacaine 0.15% Hypobaric = 244 |
Bupivacaine 0.5% Hyperbaric = 253 |
Value P |
|
Latency (min/s) |
0:57 ± 0.07 |
0:52 ± 0:13 |
0.000000002963 * |
|
Surgery duration (min) |
59 ± 6 |
59 ± 5 |
0.8299 * |
|
Block duration (min) |
73 ± 8 |
72 ± 7 |
0.7227 * |
|
Degrees of motor block MB O MB 1 MB 2 MB 3 |
0 0 27 (11%) 217 (89%) |
0 0 25 (9%) 228 (91%) |
0,7697 ** |
Table 2 Assessment of blocks in both groups
* Mann-Whitney Test ** Exact Fisher Test
In all patients, unilateral spinal anesthesia with either hypobaric or hyperbaric bupivacaine solution was satisfactory for the procedure and no patient required supplementation with general anesthesia. Tourniquet application of the operated limb was used in all patients in both groups, and none of them complained of pain during the surgical procedure. No patient had post-dural puncture headache or urinary retention. There were no complaints of back, buttock or leg pain in the subsequent three days. All patients were extremely satisfied with the anesthesia in the operated limb only. And since there was no pain in the operated limb, there was no involuntary movement of the contralateral limb.
To perform unilateral spinal anesthesia, it is necessary to introduce the local anesthetic in the correct location in contact with CSF, to avoid mixing and diluting it, administering it in a low volume and concentration that are sufficient to produce anesthesia and allow the surgical intervention to be performed without causing cardiovascular changes. It is essential to perform a lumbar puncture in the lateral decubitus position, and to use hypobaric solutions for the upper limb and hyperbaric solutions for the lower limb. In this study for short-term orthopedic surgeries and with a fixed dose of 6 mg of 0.15% hypobaric bupivacaine or the same dose of 0.5% hyperbaric bupivacaine, practically the same result was obtained with both solutions. It is essential to remain in the left lateral decubitus position for 15 minutes to avoid anesthesia in the contralateral limb.
The injection of non-isobaric local anesthetic, in lateral decubitus and remaining in this position depending on the dose and the local anesthetic, can influence the spread of anesthesia preferentially in one of the lower limbs, providing minimal hemodynamic effects. Several factors such as the type and gauge of the needle, the baricity of the anesthetic in relation to the CSF, the concentration of the anesthetic, the dose, and the injection speed.4 In this retrospective study comparing two bupivacaine solutions for unilateral spinal anesthesia, a 27G Quincke needle was used, with success in all patients.
Unilateral spinal anesthesia has been used for inguinal herniorrhaphies with hyperbaric solutions of bupivacaine, ropivacaine, and levobupivacaine, with excellent results, patient satisfaction and discharge home on the same day after surgery.11,12 Recently, ropivacaine in hyperbaric and hypobaric solutions has been recommended for unilateral spinal anesthesia.13 In this retrospective study, bupivacaine was used in both hypobaric and hyperbaric solutions, and there was no difference between the two solutions in achieving unilaterality. The higher the dose, the greater the need to remain in the lateral decubitus position to achieve unilaterality. With the fixed dose of 6 mg, 15 minutes were sufficient to maintain the solution in the operated limb, with slight passage to the contralateral limb.
Although it is believed that the injection rate has little relevance in cephalic dissemination, our group has a standard rate for both hypobaric and hyperbaric solutions.4 Depending on the type of local anesthetic used and the dose, we use 5 to 20 minutes of lateral decubitus to obtain unilaterality.4 Several studies have shown that conventional injection eventually causes turbulence and provides rapid mixing of the anesthetic in the lumbar CSF, especially when fine needles are used.4 In this study with the fixed dose of 6 mg, we always left the patient in the left lateral decubitus position for 15 minutes, both for the hypobaric and hyperbaric solutions, with the same needle gauge there was no difference between the two solutions in the cephalic spread of anesthesia. For unilaterality, the injection speed is fundamental, which must be different with the hypobaric solution (1 ml/15 s) than with the hyperbaric solution (1 ml/30 s).
A small dose of local anesthetic injected into the subarachnoid space causes minimal hemodynamic changes, with great cardiovascular stability, and unilateral blockade, with any of the solutions, causes less arterial hypotension. This fact occurred in this retrospective study, where no patient presented arterial hypotension or bradycardia during the surgical procedure.
The recovery in unilateral spinal anesthesia depends on the type and dose of anesthetic used. The average duration of the blockade was around 75 minutes with both solutions and influenced earlier hospital discharge. Postoperative analgesia was performed at the end of the procedure by blocking the nerves involved in the surgical wound with the aid of a peripheral nerve stimulator and the injection of 0.25% enantiomeric excess levobupivacaine (S75:R25) provided a duration of around 20 hours in both groups.
In a recent network meta-analysis due to the very low quality of evidence among currently available studies, future research efforts are needed to evaluate alternatives to lidocaine in the development of transient neurological symptoms.14 In our study with a fixed dose of 6 mg of 0.15% hypobaric or hyperbaric bupivacaine for unilateral spinal anesthesia with 497 patients, no case of TNS was observed.
Obtaining unilateral spinal anesthesia depends on the anesthetic used, the needle gauge, the dose used, the injection speed, and the time spent in the lateral decubitus position. In unilateral spinal anesthesia, isobaric anesthetic should not be used, and hypobaric and hyperbaric local anesthetics are indicated as they provide a greater incidence of unilaterality. Puncturing in a sitting position and immediately placing the patient in lateral decubitus is not a good technique for obtaining unilateral spinal anesthesia. Those who only use the sitting position must train to perform the procedure in lateral decubitus, which can be on the left or right side. However, choosing the left lateral decubitus position is essential, especially for much of the anesthesiology population in which the right hand is dominant, facilitating training in the same position and using hypobaric and hyperbaric solutions depending on the limb to be operated on.

©2024 Imbelloni, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.