Journal of
eISSN: 2373-6437


Research Article Volume 12 Isuue 3
1Anesthesiologist of Hospital Clínicas Municipal de São Bernardo do Campo, Brazil
2Anesthesiologist of Hospital Regional Wenceslau Lopes, Brazil
3Anesthesiologist of Hospital Clínicas Municipal São Bernardo do Campo, São Bernardo do Campo, Brazil
4Resident in Anesthesiology of Hospital Clínicas Municipal de São Bernardo do Campo, Brazil
5Master in Labour Economics, UFPB, Government employee of the State of Paraíba, CET/SBA Hospital Clínicas Municipal de São Bernardo do Campo, Brazil
Correspondence: Dr. Luiz Eduardo Imbelloni, Rua dos Coroados, 162 - Apto 45 - Bloco B, Vila Anastácio (Lapa), 05092-020 – São Paulo, SP – Brazil, Tel + 55.83.99962-4101
Received: May 14, 2020 | Published: May 21, 2020
Citation: Imbelloni LE, Ventura TB, Sakamoto JW, et al. Low hyperbaric bupivacaine doses for unilateral spinal anesthesia for open inguinal herniorrhaphy. a pilot study with 20 patients. J Anesth Crit Care Open Access. 2020;12(3):92-96. DOI: 10.15406/jaccoa.2020.12.00438
Background: Unilateral spinal anesthesia may have advantages over bilateral spinal anesthesia. Low doses of local anesthetic, slow injection speed and lateral position are facilitators to produce unilateral spinal anesthesia. The aim of this study was to perform inguinal hernia repair with unilateral spinal anesthesia and low doses of bupivacaine associated with morphine in a pilot study with 20 patients.
Material and methods: Spinal anesthesia with 0.5% bupivacaine and 26G Quincke needle was induced in a prospective pilot study in 20 patients physical status ASA I-II submitted to inguinal hernia repair. Spinal puncture was performed with patients previously placed with the side to be operated on facing downward and 5 mg of 0.5% hyperbaric bupivacaine plus 80 µg of morphine were injected at 1 mL/30 s. Sensory and motor blocks (pinprick and 0 to 3 scores) were compared between operated and contralateral sides. Hemodynamic changes, nausea and vomiting, pruritus and urinary retention were evaluated.
Results: All 20 patients were operated on using the technique employed, with no need for supplementation with sedation or general anesthesia. Unilateral block was induced in 100% of patients at 15 minutes and the end of the surgery. There has been hemodynamic stability in all patients. Urinary retention occurred in 8 patients (40%), pruritus in 4 patients (20%) and nauseas and vomiting in 4 patients (20%). No patient has developed post dural puncture headache.
Conclusion: This prospective pilot study with 0.5% hyperbaric bupivacaine (5mg) associated with morphine (80 µg) has provided predominantly unilateral block. Fifteen minutes were enough for blockade installation. Major unilateral spinal anesthesia advantages are hemodynamic stability, patients ’satisfaction and faster anesthetic recovery.
Keywords: Spinal anesthesia, unilateral spinal anesthesia, inguinal hernia repair
Unilateral spinal anesthesia is defined by placing the lateral patient on the operating table for 10-20 minutes after the subarachnoid injection of the local anesthetic. The use of unilateral spinal anesthesia in various types of surgery is to provide an adequate level of analgesia, to decrease the incidence of sympathetic block, to provide a lower incidence of lower limb motor block and depending on the dose used shorter anesthesia duration and patient satisfaction.
In 1961, a particular spinal anesthesia technique was described for patients undergoing orthopedic procedures on the lower limbs, which the authors called hemianalgesia.1 In 1985, the first article of unilateral spinal anesthesia using hypobaric tetracaine solution was published.2
In the beginning, this technique was practically used for orthopedic patients. Later, in 2004 an article appeared using unilateral spinal anesthesia to correct inguinal hernia with different solutions of hyperbaric local anesthetics. In a study comparing three solutions of hyperbaric local anesthetic (0.5% bupivacaine, 0.5% levobupivacaine and 0.5% ropivacaine) with different doses in patients undergoing open inguinal hernia repair, with patients maintained the lateral decubitus position for 15 min, a significant difference was observed in incidence of unilateral block between both sides (operated vs no-operated), but without obtaining a high incidence of unilateral spinal anesthesia.3
Comparing 15 mg of 0.5% hyperbaric bupivacaine plus 100 µg morphine for unilateral spinal anesthesia with lateral decubitus for 10 min at the same dose for bilateral spinal anesthesia, showed a significant difference between the two groups in the dispersion of analgesia and the degree of motor block.4 This dose did not produce unilateral spinal anesthesia in any patient. Comparing low doses (5 mg) of 0.5% hyperbaric, 0.5% isobaric and 0.15% hypobaric bupivacaine for orthopedic surgeries of lower limbs with patients remaining in lateral decubitus for 20 min, it was obtained unilaterally 80% with hypobaric, 76% with hyperbaric, significantly different from 28% with isobaric solution.5
Comparing the effect of 20 mg of 0.5% hyperbaric bupivacaine and remaining in the sitting position for 2 min or 60 min before being put in the dorsal decubitus, there is migration of the anesthetic site by changing the position.6 Result obtained in two articles.3,4 Using low doses of hyperbaric or hypobaric solutions of local anesthetics and with lateral decubitus for 10 to 20 minutes provides a restricted distribution of anesthesia on the operated side compared to the non-operated side.5,7,8
The objective of this pilot study with low doses (5 mg) of 0.5% hyperbaric bupivacaine associated with 80 µg of morphine for open surgical correction of inguinal hernia was to obtain asymmetric spinal anesthesia comparing both sides as well as the incidence of cardiocirculatory effects and patient satisfaction.
We conducted this study as a pilot prospective clinical trial. After gaining approval from the Ethics Committee Escola de Enfermagem Nova Esperança (011782/2013) and registration at Plataforma Brazil (CAAE: 14063513.3.0000.5179) we included 20 patients ASA (American Society of Anesthesiologists) I-II of both sexes between the ages of 17-88 years, who were due to undergo elective inguinal surgery and unilateral spinal anesthesia. As part of Program ACERTO, all patients drank a single 200 mL liquid oral hypercaloric nutritional supplement (1.5 Kcal /mL) without residue, clarified and without addition of lipid and fiber about 2 to 4 hours before surgery. The exclusion criteria for this study were infection at the subarachnoid puncture site, presence of hypovolemia, any coagulation disorder administration of thrombosis prophylaxis less than eight hours prior to the procedure, agitation and delirium, the presence of vesical catheter and mainly the patient's refusal to participate in the study after obtaining the Informed Consent Term.
Patients did not receive any pre-anesthetic medication in the ward. Upon arriving at the operating room, patients were monitored with noninvasive blood pressure, heart rate and pulse oximetry. After monitoring, venoclysis was performed with a 20G catheter and Ringer's with lactate was installed for hydration and administered intravenously 1 μg/kg fentanyl associated to 1 mg midazolam. All patients were placed in a horizontal position to perform the lumbar puncture with the side to be operated on downwards. Lumbar puncture was performed with a 26G needle with a cutting point between L3-L4 through the median or paramedian route and injected 5 mg of 0.5% hyperbaric bupivacaine with 80 µg of morphine at the rate of 1 mL/30 s. All patients were maintained in this position for 15 minutes and then placed in a horizontal dorsal decubitus. Proprioception on the 1st toe was assessed on the contralateral limb.
The sensory level of the block was assessed by the pinprick test after administration of the local anesthetic and morphine, while the degree of motor block in the lower limbs was assessed by the modified Bromage scale (grade 0 to grade 3). Both sensory and motor blocks were evaluated on both sides (operated and non-operated) at 15 minutes and after the end of the surgery. The duration of the surgery was noted.
Noninvasive blood pressure, heart rate and oximetry were assessed at 5-minutes intervals up to 15 minutes after anesthetic injection and then at 10-minute intervals until the end of surgery. If hypotension occurred was defined as 30% decrease as compared to baseline it would be treated with 5 mg intravenous ethylphenylephrine. Bradycardia was defined as HR below 50 bpm, treated with 0.5 mg intravenous atropine. A flow of 2 L / min oxygen was administered via a nasal catheter or Hudson’s mask.
Side effects, hypotension, urinary retention, nausea and vomiting and itching were noted during the procedure and until discharge from the post operative care unit. Treatment of postoperative complications included 4 mg IV ondansetron for nausea/vomiting and 0.08 mg IV naloxone for pruritus, in addition to performing urinary catheterization for urinary retention. Oral dypirone 30 mg/kg was administered at 8-hour intervals to provide additional postoperative analgesia.
All patients were followed up by telephone contact until the third postoperative day to obtain information about their satisfaction with the technique. The incidence of post dural puncture headache or transient neurological symptoms (TNS) was assessed up to the third postoperative day and until the 30th day for permanent neurological complications.
Association between categorical variables can be measured using McFadden-Puig-Kerschner performance measure, a nonparametric approach do the pseudo-R². The pseudo-R² is a measure of how well variables of the model explain some phenomenon. The McFadden-Puig-Kerschner performance measure can be obtained using kernel modal regression on mixed data. The software R performs kernel modal regression on mixed data, and finds the conditional mode given a set of training data, consisting of explanatory data and dependent data, and possibly evaluation data. Automatically computes various in sample and out of sample measures of accuracy. Association between quantitative variables can be measured using Wilcoxon rank sum test, with 5% of significance level.
Demographics data for the 20 patients are shown in Table 1. The average duration of surgery was 40.50 minutes and the average time of complete regression of unilateral spinal anesthesia was 83.50 minutes ranging from 7 to 110 minutes.
|
Data |
Results |
|
Age (years) (Extremes) |
54.65±19.67 (17 – 88) |
|
Weight (kg) (Extremes) |
65.80±11.10 (47 – 95) |
|
Heitht (cm) (Extemes) |
163.95±8.07 147 – 178 |
|
Gender: Female/Male |
1/19 |
|
Physical status: ASA I/II |
13/7 |
|
Surgery duration (min) (Extremes) |
40.50±6.26
|
|
Block duration (min) (Extremes) |
83.50±11,59 (70 – 115) |
Table 1 Demographics Data, Surgery Duration, Block Duration
Unilateral block was induced in 100% of patients at 15 minutes and also at the end of surgery. There was a significant difference in the cephalic dispersion of anesthesia at 15 minutes and at the end of surgery. The cephalad head dispersion mode was at T10 at both times, with no significant difference, as show by the McFadden-Puig-Kerschner performance measure, returning a numerical value 0.6225 (this value suggests that there is a significant dependence between the variables analyzed).
The dispersion of sensory block assessed by the pinprick test varied from T4 to T11 on the operated side at 15 minutes and from T9 to T12 at the end of surgery and there was no cephalad dispersion of analgesia on the contralateral side, resulting in 100% of unilateral spinal anesthesia (Figure 1). There was no loss of proprioception on the contralateral side assessed on the 1st toe.
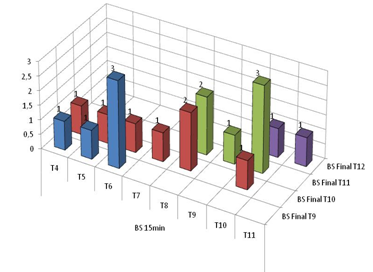
Figure 1 Sensory Block Cephalad in Operated Side and at 15 minutes and at the End of Surgery. On the Non-Operated Side, there was no Dispersion of Anesthesia.
The different degrees of block engine on the operated side at 15 minutes were: grade 3 in 16 patients (80%), grade 2 occurred in 4 patients (20%), with no block grade 1 or grade zero. At the end of the surgery, only 6 patients (30%) exhibited a complete motor block, 10 patients (50%) grade 2 and 4 patients (20%) grade 1. No degree of motor block was observed on the unoperated side either at 15 minutes as at the end of the surgery (Figure 2). Comparing the motor block on the operated side with the non-operated side at 15 minutes and at the end of the surgery, there was a significant difference using the Wilcoxon test surgery (p=0.001071) (Figure 3).
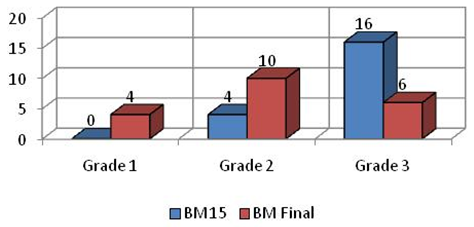
Figure 2 Motor Block Limb in Operated Side at 15 minutes and at the End of Surgery. On the Non-Operated Side, there was no Motor Block.
Unilateral spinal anesthesia was satisfactory for the surgical procedure and no patient needed general anesthesia complementation. There was no change in blood pressure and heart rate during surgery and in PACU. Urinary retention occurred in 8 patients (40%), pruritus in 4 patients (20%) and nausea and vomiting in 4 patients (20%). No patient had PDPH, or signs of TNS (back, buttock or leg pain). At the late neurological complications occurred. All patients were satisfied with the technique. All 20 patients with unilateral spinal anesthesia referred to a nice sensation of being able to feel the contralateral limb.
The results of this prospective pilot study using low doses (5 mg) of 0.5% hyperbaric bupivacaine associated with 80 µg of morphine demonstrated to produce a unilateral spinal block in 100% of patients, with no sensory block, motor block and proprioception on the contralateral side. All patients were happy with the technique and there has been no a cardiovascular change or neurological complications. In a previous study with patients undergoing unilateral lower limb surgery and using the same dose (5 mg of 0.5% hyperbaric bupivacaine without morphine unilateral spinal anesthesia was obtained in 85.7% of patients.8
Limiting the block to the operative side by just using small doses of local anesthetic, injected slowly through pencil-point or cut-point needles, in patients maintaining the lateral decubitus position for 10–15 minutes after the injection is a very simple and effective way to optimize the efficiency of unilateral spinal block.9
When unilateral spinal anesthesia is indicated, the main objectives of this technique are to provide analgesia and motor block in only one side, improving patient comfort and satisfaction, and preventing hemodynamic changes. Several factors have been linked to unsatisfactory results unilateral spinal anesthesia, including patient position during the subarachnoid puncture, the length of time in the lateral position, the injection speed, the dose of the local anesthetic and the density of the solution used in relation to the CSF.9 In a study comparing low dose of 5 mg of 0.5% isobaric, 0.15% hypobaric and 0.5% hyperbaric bupivacaine in orthopedic surgery the incidence of unilateral spinal anesthesia was obtained in 80% of patients with hypobaric, 76% with hyperbaric and only 28% with isobaric.5 This study showed that both hypobaric and hyperbaric solutions are ideal for unilateral spinal anesthesia. In the present study with the same dose of 0.5% hyperbaric, unilateral spinal anesthesia was obtained in 100% of patients for open surgical correction of inguinal hernia.
Unlike other authors who used high doses of local anesthetic hyperbaric (8 to 12 mg)3 or 15 mg hyperbaric bupivacaine,4 which obtained only difference between the operated and non-operated side, we used only 5 mg of hyperbaric bupivacaine and stay for 15 min, resulting in unilateral spinal block in all patients. Complete regression of spinal anesthesia occurred on average between 166 to 210 min3 and 223 min,4 different from the results with low dose of hyperbaric bupivacaine that varied between 70 and 115 minutes, similar result with same dose and isobaric, hypobaric and hyperbaric bupivacaine solutions for orthopedic surgeries.5
Recovery from spinal anesthesia depends on the type of anesthetic used (lidocaine, bupivacaine, procaine, ropivacaine, levobupivacaine) and mainly on the dose used. Unilateral spinal anesthesia with low dose (5 mg) of 0.5% hyperbaric bupivacaine was obtained for all patients.8 Studying different doses of 0.4% enantiomeric excess levobupivacaine (S75: R25) to obtain unilateral spinal anesthesia in orthopedic patients showed that the duration of anesthesia was dose dependent.10 Thus, doses of 4 mg, 6 mg and 8 mg provided recovery time from anesthesia of 75, 117, and 174 minutes, respectively, with positive correlation between doses,10 similar in duration with 5 mg of 0.5% hyperbaric bupivacaine in this study for unilateral inguinal herniorrhaphy.
The most important factor influencing the incidence of obtaining unilateral spinal anesthesia is the type of anesthetic (lidocaine, bupivacaine, procaine, levobupivacaine) and the dose used. Dose reduction is crucial for restrict the blockade to one side. However, an excessive reduction of local anesthetic can increase the rate of spinal anesthesia failure.1 Increasing the dose may decrease the incidence of unilateral spinal anesthesia and also increase the duration of the block.3,10
Low doses of local anesthetic injected into the subarachnoid space causes minimal hemodynamic changes, with great cardiovascular stability. Unilateral spinal anesthesia with either solution causes less arterial hypotension.5 In the present study for open correction surgeries of inguinal hernia, the dose of 5 mg of 0.5% hyperbaric bupivacaine in no patient showed cardiocirculatory changes.
Postoperative urinary retention is one of the postoperative complications causing much discomfort for patients. Its etiology has many factors and depends on the type of anesthesia, type and duration of surgery, and drugs used in perioperative period. Its incidence varies from 5 to 70%.11 Inguinal hernia repair has been characterized as high risk for urinary retention.12
The use of postoperative opioids can itself lead to a higher incidence of postoperative urinary retention.11 The most commonly used practice for spinal analgesia is often a mixture of local anesthetic. It was suggested that the combination of local anesthetic and opioids improves analgesic efficacy with fewer side effects. The meta-analysis evaluating the use of the association of opioids with the local anesthetic for single-shot spinal anesthesia in patients undergoing minor surgery showed that the dose of morphine ranged from 50 to 200 µg.13 The use of morphine increased the risk of nauseas and vomiting, urinary retention and itching. In this study with a smaller dose of hyperbaric bupivacaine associated with 80 µg of morphine there was 20% nausea and vomiting, 20% itching and 40% urinary retention, requiring bladder catheterization.
In conclusion, results of this prospective pilot study with 5 mg of bupivacaine associated with 80 µg of morphine is a technique that limits spinal anesthesia at the operative side for inguinal hernia repair, resulting in an average shortest duration of spinal anesthesia of 83.50 minutes. The association of morphine resulted in important side effects, such as urinary retention in 40% of patients. The use of peripheral blocks such as paravertebral block14,15, ilioinguinal iliohypogastric nerve block16 or combined ilioinguinal blockade and local infiltration anesthesia17 is advantageous in terms of prolonged postoperative analgesia and encourages early ambulation. It may be a better alternative for postoperative analgesia than the use of subarachnoid morphine.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.

©2020 Imbelloni, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.