International Journal of
eISSN: 2574-8084


Research Article Volume 1 Issue 2
1Department of Physics, Science Faculty, Akdeniz University, Turkey
2Department of Nuclear Medicine, Akdeniz University, Turkey
Correspondence: Nina Tunçel, Akdeniz University, Science Faculty, Department of Physics, Dumlupinar Boulevard 07058 Campus Antalya, Turkey
Received: September 22, 2016 | Published: December 28, 2016
Citation: Tunçel N, Karayalçin B, Özkan GK, et al. The environmental dose measurements of high dose iodine-131 treated thyroid cancer patients during hospitalization period. Int J Radiol Radiat Ther. 2016;1(2):38-41. DOI: 10.15406/ijrrt.2016.01.00009
This study presents the risks associated with high dose 131I treatment which is used in nuclear medicine. Patients were confined to two isolation rooms which were completely covered with lead. Each room is designed for two beds which are separated by lead separators. In the fixed activity protocol, a high activity 3.7-7.4GBq (100-200 mCi) 131I was administered to 12 patients. In general, the patients were isolated for a period of 2-3days. The dose rates were measured at 1m from the patient’s thyroid and abdominal levels at different time intervals. The clean and unclean room dose rate measurements were performed at each isolated room. These were 0.43+0.56 mRh-1 and 1.49+1.99 mRh-1 respectively. The maximum dose rate was measured at the toilet bowl. Moreover the pillow had 5.02+4.35 mRh-1 at the unclean room. The dose measurements at surrounding rooms and service door-corridor were done with patients allocated in their room. There were 7.06+10.33 µRh-1 and 87.75+91.87 µRh-1, respectively. The measurements at the same places without patients were 1.17+8.84 µRh-1 and 32.92+12.98 µRh-1, respectively. The time dependent dose curves for each therapeutic value of 3.7, 5.5 and 7.4GBq were generated by exponential fitting curves for each patient. Average and standard deviation of cumulated dose(mR) at 1m about level of abdominal and thyroid were calculated along hospitalization period (maximum 65h).
Keywords: thyroid cancer, iodine-131, environmental dose, remnants, hospitalization, contamination, saliva, thyroid tissue, radiation, radioiodine
I-131, iodine-131; DTC, differentiated thyroid cancer; Ca, cancer
Radioiodine mostly 131I is one of the oldest clinical radionuclide types which used widely spread in diagnosis and currently used in the treatment of both thyreotoxicosis and thyroid cancer. This is an integral part of differentiated thyroid carcinoma therapy.1,2 For most thyroid cancer treatments, large doses of 131I are administered to ablate residual thyroid tissue and functional metastases from thyroid cancer. The success of thyroid ablation with 131I depends mainly on the mass of remaining thyroid tissue in the neck and the initial dose rate to this tissue.3 The activity to be used for radioiodine therapy still remains subject to discussion at differentiated thyroid cancer (DTC) for ablation of postsurgical thyroid remnants, destruction of metastases and etc. While it is performed by either administering an empiric fixed dose or using dosemetry-guided activities.3 There is a broad range of the conventional fixed activities of 131I recommended to be administered.4,5 Normally, the activity is limited for safety reasons to around 7.4 GBq.6 A summary on the use of fixed activities for the treatment of DTC can be found in a review articles.7‒9 The lesion-based dosemetry concept, mainly on the data of Maxon et al.,10,11 aims at improving the efficacy of the treatment by achieving an absorbed dose threshold of more than 300Gy to remnants. Because of radiation safety considerations, application of large doses of 131I greater than 800MBq requires patient hospitalization.12,13 Most of the administered radioiodine not taken up by thyroid tissue will be excreted from the patient primarily by the kidneys, and consequently, the patient should be encouraged to drink freely to minimize dose to kidneys, bladder and gonads. So, a great majority of the administered activity will appear in the urine.2 For most patients, 35%-75% of the administered dose is excreted within the first 24h after dose administration.13,14 The next most significant pathway is saliva. This will manifest in contamination of eating and drinking utensils, and pillow coverings (due to saliva excretion during sleep). Lesser pathways are sweat and faeces. The proportion of each (apart from urine) will vary widely.2 Radiation contamination could be expected from patient’s urine, perspiration and saliva over the course of the isolation period. For this reason, patients should be considered as a potential source of radiation contamination, especially during the first 48hours following administration.2 When considering radiation safety precautions for attending personnel, members of the general public and patients in adjacent rooms, it is important to remember that 131I emits both negative β particles and prominent gamma photons. Iodine-131 is typical of a complex beta decay scheme with physical half-life of 8.05days. There are five different nuclear energy levels that correspond to different values of Emax (maximum beta energy). Each negative beta emission for I-131 has one or more corresponding gamma emissions. The beta emission has an average energy of 192keV (max energy=607keV (90%), and 810keV (0.4%)) and the beta particle will deposit its energy within 2.2mm and 3.1mm, respectively of its site of origin with a mean tissue range of only 0.8mm.3 The β particles deliver the major portion of the radiation dose to the remnant thyroid tissue, whereas the penetrating gamma ray poses a potential radiation hazard to others outside the patient’s room. In addition to personnel irradiation, external and internal contaminations are potential hazards to personnel entering the patient’s room after dose administration. The administered radioiodine not taken up by thyroid tissue is excreted by the urine in the 48hours or so following administration. However, some is excreted by perspiration and saliva. For this reason, patients are considered as a potential source of radiation contamination, especially during the first 48hours following administration. Till few hours following administration, the gut may contain a significant amount of radioactive material, rapidly decreasing with time. Contaminations in clothing and room furniture are seen and need more concern with spread of low dose radiation hazards. Once the patient is dosed, regulations may require a short period of isolation in the medical facility, typically 2 to 3days, until radiation exposure rates drop to acceptable levels. It is during this time that the greatest potential exists for contamination and radiation exposure problems. Thoughtful planning, adequate radiation safety education for attending personnel and proper precautionary measures taken can minimize potential problems associated with such therapies. The modes of exposure to other people are: external exposure, internal exposure due to contamination, and environmental pathways.15 In order to properly evaluate the extent of potential problems associated with therapeutic oral doses of 131I, exposure rate or dose rate measurements are taken after each radionuclide therapy administration. It is recommended to measure the rooms for clean and unclean situations. Also the surroundings of isolation unit could be surveyed with and without patient occupation. In most circumstances, the risks from internal contamination of others are less significant than those from external exposure.16 Iodine-131 typically results in the largest dose to medical staff, the public, caregivers and relatives.15 The decision to hospitalize or release a patient after therapy should be made on an individual basis considering several factors including residual activity in the patient, the patient’s wishes, family considerations (particularly the presence of children), environmental factors, and existing guidance and regulations.15 Current recommendations regarding release of patients after therapy with unsealed radionuclide vary widely around the world. However, the decision to release a patient is based on the assumption that the risk can be controlled when the patient returns to their home.15 This is generally achieved by combining an appropriate release criterion with well tailored instructions and information for the patient that will allow them to deal effectively with the potential risk.16 In our country it is obligatory to hospitalize the patients receiving high doses of radioactive iodine, the same as European countries regulations. The limit for hospitalization is 800 Mega Becquerel (MBq) that defined by Turkish Atomic Energy Authority. Hospitalization is required for patients receiving doses above this amount. However, the patients whose house conditions are not suitable and who will receive doses <800MBq can be hospitalized.12 The Radioiodine-131 activity is supposed to remain <600MBq in patient’s body, so the external measurements received at the abdominal level from 1meter distance is required to be under 30 micro Sievert per hour (µSv/h) during their discharge. Additionally, in ‘protection from radiation guide, 97 Europe’ it was stated that this limit for the residual activity remaining in patient’s body needed to be 600MBq or the external measurement value received from 1meter distance was required to be <30µSv/h.17,18 This study presents the risks associated with treatment of high dose radioactive iodine in patients with differentiated thyroid cancer by day to day dose management during hospitalization period and release of them.
This retrospective study included 12 (7 female and 5 male) thyroid cancer patients. Radioiodine 131 was used in differentiated thyroid cancer (DTC) for ablation of postsurgical thyroid remnants (10 patients) and destruction of metastases (2 patients). In the fixed activity protocol a high activity, typically 3.7, 5.5 and 7.4GBq (100, 150 and 200mCi) 131I was administered to 5, 6 and 1 patients respectively. Therapeutic doses of 131I are administered orally in capsule form. In general, the patients remained in isolation for a period of 2-3days to confirm discharge limit according to national regulations. Patients were confined to the two isolation rooms having walls covered with lead. Each room is designed for two beds which were separated by a lead separator. This isolation therapy ward have been managed to protect other patients and staff based on the national regulations. In this study the patients were hospitalized in dedicated rooms under license taken from national regulations. The special delay tank at hospital ground is designed for radioactive waste disposal. For environment dose measurements the dose rate meter (Inspector Radiation Alert, S. E. International, Inc., USA) was used. The bed, bathroom and the furniture that belong to the hospital were surveyed before and after room cleaning. Surrounding rooms and service door-corridor measurements were done with patients and without patients. Moreover, the patient dose rate at 1m about thyroid and abdominal level measurements were performed for the first application time and 1st-3th days by the same device. The time dependent effective half life was calculated for fast and slow cleaning phases from the values that were obtained at level of the abdominal and thyroid, respectively. The time dependent dose curves for each therapeutic value of 3.7, 5.5 and 7.4GBq were generated by fitting curves equations. This dose analyzing method was performed on all patients by daily tracing.
The clean and unclean room dose rate measurements were performed at each isolated room. The overall results were 0.43+0.56 mRh-1 and 1.49+1.99 mRh-1 respectively. The maximum dose rate was measured at the toilet bowl for both situations 1.13+1.51 mRh-1 and 4.22+2.20 mRh-1, respectively. Moreover the pillow had 5.02+4.35 mRh-1 at the unclean room. Clean and unclean pillow dose rate range 0.03-2.12 mRh-1 and 1.33-13 mRh-1, also the median values were 0.15 mRh-1 and 3.25 mRh-1, respectively. Surrounding rooms and service door-corridor measurements with patients were 7.06+10.33 µRh-1 and 87.75+91.87 µRh-1, and without patients were 1.17+8.84 µRh-1 and 32.92+12.98 µRh-1, respectively. The background level was 0.014mRh-1 in the isolation area. The dose rate values at 1 m about level of abdominal and thyroid for the first application time, and 2-3thdays were plotted for each patient. The fast and slow cleaning time was calculated and the ranges were 6.7-43.2h and 6.7-79.6h, respectively. The average of fast and slow cleaning time was 17.3+9.4h and 27.7+20.2h, also the median values were 17.18h and 22.53h respectively.
The time dependent dose curves for each therapeutic value of 3.7, 5.5 and 7.4GBq were generated by exponential fitting curves for each patient. In this way, the accumulated dose was calculated based on the area under fitting curve of dose rate measurements at 1 m about level of abdominal and thyroid. The Figure 1 & Figure 2 are shown these curves about abdominal and thyroid levels respectively for five patients treated by 3.7GBq. The average and standard deviation of accumulated dose (mR) according to therapeutic value was calculated along hospitalization period. The results are shown in Table 1.

Figure 1 The time dependent dose curves for each therapeutic value of 3.7GBq were generated by exponential fitting curves for each of 5 patients about abdominal level at 1m.
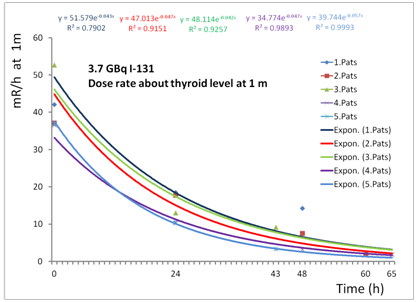
Figure 2 The time dependent dose curves for each therapeutic value of 3.7GBq were generated by exponential fitting curves for each of 5 patients about thyroid level at 1m.
Administrated activity (GBq) |
Average and standard deviation of accumulated dose (mR) along hospitalization period (maximum 65h) at 1m about level of |
|
Abdominal |
Thyroid |
|
3.7(5 patients) |
817.62+238.39 |
919.42+213.73 |
5.5(6 patients) |
1423.50+704.01 |
1497.93+695.62 |
7.4(1 patient) |
912.34 |
669.82 |
Table 1 The average and standard deviation of accumulated dose (mR) according to therapeutic value
When considering radiation safety precautions for attending personnel, members of the general public, and patients in adjacent rooms, it is important to consider gamma photon that poses a potential radiation hazard to others outside the patient’s room. It is the β particles that deliver the major portion of the radiation dose to the remnant thyroid tissue, and it is the other source of contaminations that present potential hazards to personnel entering the patient’s room after dose administration, and also after the patient is removed from the room. It is during this time that the greatest potential exists for contamination and radiation exposure problems. Thoughtful planning, adequate radiation safety processes for proper precautionary measures taken by staff can minimize potential problems associated with such therapies. To properly evaluate the extent of potential problems associated with therapeutic oral doses of 131I, we measured the rooms for clean and unclean situations. Also the surroundings of the isolation unit were surveyed with and without patient occupation. Surrounding rooms and service door-corridor measurement values were within normal limits during the patient’s isolation period. During the hospitalization period of high dose 131I treated thyroid cancer patients, the highest contamination was found at the toilet bowl and the pillows. Therefore maximum care should be given to the cleaning of these places and the patient and their relatives should be educated in this respect. Our results suggest that the dose value of ablated patients would be estimated by dose rate measurement at 1m about thyroid level. More data along first 24hours is needed to confirm the evaluating protection properties in hospitalization of patients receiving radionuclide treatment.
None.

©2016 Tunçel, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.