International Journal of
eISSN: 2574-8084


Research Article Volume 6 Issue 5
1Head of Department, Department of Radiology, Dr Baba Saheb Ambedkar Medical College and Hospital, India
2Associate Professor, Department of Radiodiagnosis, AIIMS Rishikesh, India
Correspondence: Pankaj Sharma, Associate Professor, Department of Radiodiagnosis, AIIMS Rishikesh, India, Tel (091)09910661497, 0120-4109552
Received: July 17, 2019 | Published: September 26, 2019
Citation: Kumar RR, Sharma P, Gupta P. Sonographic evaluation of gynecological masses with its pathological correlation. Int J Radiol Radiat Ther. 2019;6(5):167-172. DOI: 10.15406/ijrrt.2019.06.00241
Introduction: The differentiation of adnexal masses as benign and malignant is difficult on imaging and first modality used for this purpose is Ultrasound.
Aim: To assess the usefulness of Gray Scale Ultrasound and Colour Doppler in differentiating benign and malignant adnexal masses in Indian population, by using a scoring system proposed by Alcazar, et al.
Materials and methods: The study was conducted in Department of Radiodiagnosis, Deen Dayal Upadhyay Hospital and Delhi over a one year period. Fifty patients were evaluated using scoring system proposed by Alcazar JL, et al. The efficacy of scoring system was evaluated by fine needle aspiration cytology or histopathological examination of the mass as a gold standard. Statistical analysis was done using the SPSS Stastical Package. Data was analyzed statistically by one way ANOVA and the Student t test for independent samples. The chi square test was used for categorical data. A probability value less than 0.05 was considered statistically significant.
Results: In present study, most significant parameters came out to be thick papillary projection i.e> 3mm (p=0.01) and thick septa i.e> 3mm (p=0.02) on grey scale and resistive index<0.4 (p=0.006), high velocity/low resistance flow (p=0.01) and moderate to abundant flow (p=0.01) on Colour Doppler.
Conclusion: Present study serves to emphasize the role of Ultrasound gray scale and Colour Doppler to differentiate benign from malignant adnexal mass and usefulness of Alcazar scoring system. Important parameters in this study, which helped in differentiating benign and malignant adnexal masses, were: thick papillary projection, thick septa and resistive index<0.4, high velocity/low resistance flow and moderate to abundant flow.
Keywords: ultrasonography, doppler, velocimetry, transvaginal, echotexture
Clinicians are faced with dilemma of differentiating malignant tumors from benign masses in patients presenting with pelvic mass. When evaluating pelvic mass, gynecologists first consider ovarian pathology, as ovarian pathology is responsible for 70% of pelvic masses found at exploratory surgery on patients with preoperative diagnosis of pelvic mass. Precise diagnosis is required to decide appropriate treatment in such patients. Benign masses can be treated conservatively or by minimal invasive technique.1 whereas malignant masses should be referred to tertiary care centers for proper diagnosis and management. Ultrasound is noninvasive, easily available test used for differentiating benign from malignant pelvic masses. It is possible to suspect malignancy on basis of ultrasound and Colour Doppler findings, but definite diagnosis cannot be done based on ultrasound and Colour Doppler findings.2,3 Sonographic scoring systems were first used for differentiating benign and malignant adnexal masses, by DePriest et al.4 and Sassone et al.5 But, both of these scoring system were based on Gray scale findings only. In 2003, new scoring system was proposed by Alcazar et al.6 This new scoring system included both Gray scale and Colour Doppler parameters for differentiating benign from malignant adnexal masses. Important parameters which were used to differentiate benign from malignant adnexal masses were: thick papillary projections, solid areas, blood flow location and velocimetry. The new scoring system proposed by Alcazar, et al had better diagnostic performance then scoring system used by DePriest et al. and Sassone et al. But, scoring system used by Alcazar, et al was based on study population in small geographical location in Spain only and needs further validation. Scoring system proposed by Alcazar, et al has yet not been evaluated on Asian population. The aim of this study was to assess the usefulness of Gray Scale Ultrasound and Colour Doppler in differentiating benign and malignant adnexal masses in Indian population, by using scoring system proposed by Alcazar JL, et al.
The study was conducted in Department of Radiodiagnosis, Deen Dayal Upadhyay Hospital and Delhi over a one year period between 1st Jan 2010–31 Dec 2011. This study was done as part of dissertation for post graduate qualification in Radiodiagnosis. Sample size was decided after discussion with Stastician in our Institution. Ethical approval for this study was taken from Institute Ethical Committee. Participants were enrolled for this study after taking Informed Consent.
Study population included patients fulfilling following criteria:
Exclusion criteria
A total of 1011 patients, suspected to have adnexal masses, were examined in Obstretics and Gynecology OPD in one year period and subsequently referred to Radiology department for TVS. Out of 1011 patients, only 650 patients came for TVS and 439 patients didn’t came for TVS due to personal reasons including long waiting period. Only 174 patients were found to have adnexal mass on TVS. Out of 174 patients, 101 patients did not come for follow up scans and changed the hospital because they were not satisfied with the treatment and long waiting period. Out of 73 patients, 12 patients were referred to higher centers for advance treatment and 11 patients refused for FNAC/Histopathological examination. Finally, 50 patients were evaluated using scoring system proposed by Alcazar, et al in 2003. This scoring system may yield a total score of 0 to 12, with the best cut off value as score of >6 (Table 1). TVS including Colour Doppler was done on Philips HD-11 with 10 MHz probe to assess: volume of tumor, distribution (unilateral/bilateral), wall thickness, inner wall structure, septations inside tumor, papillary projection thickness, presence of solid area and echogenicity, vascularization, resistance index and peak systolic velocity and velocimetry. Blood investigations including serum tumor marker: CA 125 and x ray chest was also done. Statistical analysis was done using the SPSS Statistical Package. Data was analyzed statistically by one way ANOVA and the Student t test for independent samples. The chi square test was used for categorical data. A probability value less than 0.05 was considered statistically significant.
|
Value |
Thick papillary projections |
Solid areas |
Blood flow locations |
Velocimetery |
|
0 |
No |
No |
Not present or peripheral |
Other |
|
2 |
Present |
- |
- |
High velocity/ low resistance |
|
4 |
- |
Present |
Central |
- |
Table 1 Scoring System used by Alcazar JL et al.6
The mean age of patients with benign tumor and malignant tumor was 31.68±8.1 years and 50.37±12.7 years respectively. Mean volume of malignant adnexal masses (938.37±659.37 cc) was significantly higher than benign adnexal masses (278.95±217.11). Table 1 shows parameters which were used for adnexal mass evaluation. Score of 0 or 2 was given depending on absence or presence of thick papillary projection. Score of 0 or 4 was given depending on absence or presence of solid areas. Score of 0 or 4 was given depending on blood flow location. If no flow or peripheral flow was present, then 0 score was given. However, if central flow was present, then score of 4 was given. If there was high velocity/low resistance, then score of 2 was given. If any other pattern of blood flow was present, then 0 score was given.
In our study, wall thickness>3mm did not relate with malignancy, but irregular wall structure (p=0.02) and thick papillary projection was significantly associated with malignancy (p=0.01). Presence or absence of septa did not show a significant association with malignancy (p=0.27). Presence of solid areas (p=0.037) or purely solid echogenicity (p=0.39) in adnexal masses was statistically important predictor of malignancy. W didn’t calculated odd ratio in our study. Central vascularization was significantly associated with malignancy (p=0.02). On applying univariate logistic analysis in Colour Doppler parameters, it was found that the amount and location of flow as well as resistive index<0.4 were statistically significant parameters for differentiating benign from malignant adnexal masses. Table 2 shows correlation of scoring system proposed by Alcazar, et al with FNAC/Histopathology report, in our study population. Alcazar scoring system was found to be associated with high sensitivity (100%), specificity (95.45%), positive predictive value (86.67%) and negative predictive value (100%), in our study population. The most significant parameters in our study were: thick papillary projection i.e> 3mm (p=0.01) and thick septa i.e> 3mm (p=0.02) on gray scale and resistive index<0.4 (p=0.006), high velocity/low resistance flow (p=0.01) and moderate to abundant flow (p=0.01) on Colour Doppler. Using this scoring system in our study and taking cut off value for malignancy > 6, we found that out of total 50 patients (Table 2), 35 (70%) had score between 0-5 and all of them were found to be benign on FNAC/histopathology. 15 (30%) cases had a score between 6-12, out of which 13 (86.67%) were malignant. Only 2 (13.33%) cases with score between 6-12 are benign (Figures 1−10).
|
FNAC/Histopathology Report |
Score (0–5) |
Score (6-12) |
|
Benign adnexal mass |
35 |
2 |
|
(Simple Cyst: 9, |
(Tubercular Tubo-ovarian abscess) |
|
|
Malignant adnexal mass |
0 |
13 |
|
(Mucinous Cystadenocarcinoma: 3, Serous Cystadenoma: 7, Fallopian tube carcinoma: 1, Clear cell carcinoma: 1 and Metastasis: 1) |
Table 2 Correlation of scoring system proposed by Alcazar JL et al.6 with FNAC/Histopathology report, in our study population (Figures 1 to 10)
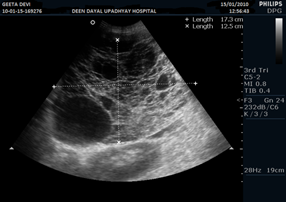
Figure 1 Ultrasound pelvis image in a 50 year female showing densely septated mass with irregular margins.
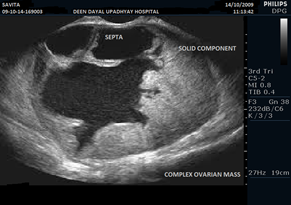
Figure 2 Ultrasound pelvis image in a 54 year female showing solid-cystic mass with thick septations, thick and irregular wall. Mural nodules are also seen.
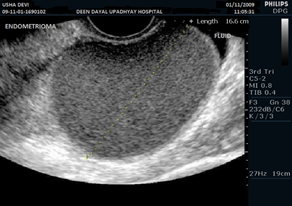
Figure 3 Ultrasound pelvis image in a 28 year female with endometrioma showing well defined, thin walled cyst with diffuse fine homogenous internal echoes.
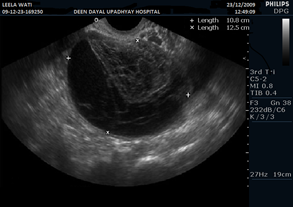
Figure 6 Ultrasound pelvis image in a 23 year female showing well defined, thin walled cyst with fine internal reticular pattern.
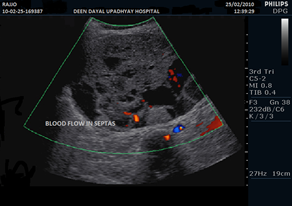
Figure 7 Ultrasound pelvis image in a 53 year female showing solid-cystic mass with septations. Blood flow in septa is also seen.
The adnexal masses represent a common problem in clinical practice, as it is very difficult to differentiate benign masses from malignant masses on imaging: Ultrasound, Computed Tomography and Magnetic Resonance Imaging. An accurate diagnosis is essential to establish the optimal treatment of patients presenting with adnexal mass. Ultrasound is usually first imaging modality used for this differentiation. To overcome the limitation of Ultrasonographic measurements, use of sonographic scoring system has been advocated. DePriest, et al evaluated 121 patients and differentiated benign and malignant adnexal masses using three gray scale criteria: tumor volume, wall structure and septal structure. Sasson, et al evaluated 143 patients and differentiated benign and malignant adnexal masses using combination of TVS and Aspiration Cytology. Limitation of study done by Depriest, et al and Sasson, et al was that in both these studies only gray scale features were included in scoring system and Colour Doppler parameters were not evaluated. Alcazar, et al evaluated 705 adnexal masses in 665 patients in first part of study in Spain, using scoring system which comprised both gray scale and Colour Doppler parameters. In second part of study, Alcazar, et al cross validated scoring system in 90 adnexal masses in 86 patients. Diagnostic performance was better using scoring system proposed by Alcazar, et al than scoring systems proposed by DePriest, et al and Sasson, et al. We used scoring system proposed by Alcazar, et al to evaluate adnexal masses in 50 Indian patients. Significant limitation of our study was that we were able to evaluate finally only 50 patients, even though we started with assessing 1011 patients. In our study, all 50 females were evaluated using TVS including Colour Doppler using scoring system advocated by Alcazar, et al. Findings were confirmed by FNAC or histopathological diagnosis of tissues obtained from laparotomy.
In our study, we had taken cut off of 6 to differentiate benign from malignant adnexal masses. All patients with score less than 6 were found to have benign adnexal masses, 13 patients with score more than 6 were found to have malignant adnexal masses & only 2 patients with a score more than 6 were found to have benign adnexal masses. Both these patients with score more than 6, had adnexal masses with solid echotexture with abundant central flow that showed high velocity/low resistance pattern. In these 2 patients, Differential Leucocyte count (DLC) showed lymphocytosis and Erythrocyte Sedimentation rate (ESR) was raised. X Ray Chest showed findings suggestive of Pulmonary Koch. Both patients responded when treated conservatively with antitubercular drugs. After three months of treatment, lesion regressed and ascites disappeared. There was one more case also of tuberculosis, presenting as tubo-ovarian mass, but qualified only score 4 because of presence of solid areas only, no flow and no papillary projections were noted. In this patient also, DLC showed lymphocytosis and ESR was raised. Chest X Ray was normal but ultrasound showed multiple enlarged conglomerated mesenteric lymph nodes with ascites. In our study, false positive results were due to tuboovarian mass of tubercular etiology.7
The main source of false positive result using scoring system proposed by Alcazar, et al, in previously published study include ovarian cystadenofibroma (unilocular cyst with solid areas and central flow) and ovarian fibroma (typically solid tumors).8 We did not come across any ovarian cystadenofibroma/ovarian fibroma in our study.
Ultrasonographic and Colour Doppler technique is highly operator dependent and hence a learning curve always plays a significant role in determining the efficacy.9−17 Operator experience is of utmost importance, when we use Ultrasound for adnexal mass evaluation. In our study, two Sonologists with seven and ten years experience respectively, evaluated all adnexal masses in 50 Indian patients.
Previously published studies have highlighted few non-ovarian cystic lesions, which can create confusion, when we are evaluating pelvic masses:18
Hence, we should be very careful and take into consideration all gray scale and Colour Doppler parameters, so that we are able to correctly differentiate benign from malignant adnexal masses. In postmenopausal women, our index of suspicion should be high for malignancy. When we compared our study with study published by Alcazar, et al (Table 3), we found Positive Predictive Value (PPV) to be 86.67 in our study as compared to PPV of 71.2 in study published by Alcazar et al.6 However, Sensitivity, Specificity and Negative Predictive Value (NPV) in our study were comparable to Sensitivity, Specificity and NPV in study published by Alcazar, et al. The cause of high PPV in our study done in India as compared to study done by Alcazar, et al in Spain is not clear.
|
Alcazar scoring system |
||
|
Original study published by Alcazar JL, et in 2003 |
Present study |
|
|
Sensitivity |
100 |
100 |
|
Specificity |
94.9 |
94.59 |
|
PPV |
71.2 |
86.67 |
|
NPV |
100 |
100 |
Table 3 Comparison of present study with original study done by Alcazar JL et al.6
We hereby conclude that scoring system proposed by Alcazar, et al can be reliably used to differentiate benign from malignant adnexal masses in Indian population, as this scoring system has high sensitivity and specificity. In our study population, two patients out of fifteen had score of more than 6 and were later found to have tuberculosis. Tuberculosis is a great mimicker, especially in Indian population and can result in false positive result. All patients with score less than 6 were found to have benign adnexal masses. Small sample size is significant limitation of our study and for reaching meaningful conclusion; we hereby propose that Scoring system proposed by Alcazar, et al should be validated by enrolling large population spread across different continents and follow up for at least one year.
None.
Nill.
Author declares that there is no conflict of interest.

©2019 Kumar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.